
Incidence, Severity, and Short-Term Outcome of Acute Kidney Injury in Hospital Admissions of Hong Kong
*Corresponding Author(s):
Cheuk-Chun SzetoLi Ka Shing Institute Of Health Sciences Lihs And Faculty Of Medicine, The Chinese University Of Hong Kong, Shatin, NT, Hong Kong
Tel:+852 35053101,
Email:ccszeto@cuhk.edu.hk / cheukchunszeto@gmail.com
Abstract
Background: Acute Kidney Injury (AKI) is a common problem in hospitalized patients and is associated with poor clinical outcome. We studied the incidence, severity, and short-term outcome of AKI amongst patients admitted to a general hospital in Hong Kong.
Methods: All hospital admission to a regional hospital of Hong Kong in 2012 were reviewed in a retrospective cohort study. Serum creatinine levels before, during, and after the hospitalization were retrieved from the electronic health record. AKI episodes were identified by the serum creatinine criteria of the Kidney Disease: Improving Global Outcomes (KDIGO) AKI guideline.
Results: Among the 125,517 adult hospital admissions, AKI was present in 11456 episodes (9.1%) of 6280 patients. With a catchment of 523,831 adults, the annual population incidence of AKI was 2.2%. Amongst the stage 2 or 3 episodes, 806 (56.4%) were admitted to the medical unit, 144 (4.5%) required temporary dialysis support, median hospital stay was 8 days (Inter-Quartile Range [IQR] 4 to 16 days), and only 68.9% had complete recovery. Recurrent AKI episode developed in 2326 patients (37.0%), and 1129 (18.0%) had more than one recurrent episodes. The median time to the recurrent AKI episode was 26 days (IQR 12 to 58 days).
Conclusion: AKI was present in 9.1% of all adult hospital admissions in Hong Kong. A substantial proportion of patients developed recurrent AKI episodes or did not have complete recovery. Further research should be directed to the identification of risk factors and prevention measures for AKI recurrence.
Keywords
Acute kidney injury; Hospitalized patients; Kidney disease; Serum creatinine
Introduction
Acute Kidney Injury (AKI) is a major public health problem that affects millions of patients worldwide, and it is associated with poor short-term morbidity and mortality [1,2]. In addition, survivors of AKI incur long-term risks for developing Chronic Kidney Disease (CKD) [3] and progression to dialysis-dependent End-Stage Renal Disease (ESRD) [4,5].
There are numerous published studies on the incidence of AKI on a community-based population [6-9]. For example, Lafrance et al. [6], reported that using the ratio definition of serum creatinine level, the incidence of AKI ranged from 12.5% to 18.3% of all hospital admissions. From a population-based point of view, Ali et al. [7], reported that the incidences of AKI and acute-on-chronic renal failure were 1811 and 336 per million population, respectively. Using the KDIGO definition, a meta-analysis of 312 studies estimated that 1 in 5 adults and 1 in 3 children worldwide experience AKI during a hospital episode of care [8]. Furthermore, the incidence of AKI has been rising over the past 2 decades. Hsu et al. [9], reported that the incidence of non-dialysis requiring AKI increased from 322.7 to 522.4 per 100,000 person-years from 1996 to 2003.
Recently, the clinical importance of recurrent AKI is increasingly recognized. Recurrent AKI is common among patients after a first hospitalized AKI and has a high potential to be associated with cardiovascular events, mortality, and CKD development [10,11]. Around 23% to 31% of patients admitted with AKI experienced a second hospitalization with AKI [12,13], with the second episode of AKI occurring a median of 216 days years after the first hospitalization [12]. Older age, black race, Hispanic ethnicity, lower baseline estimated Glomerular Filtration Rate (GFR), proteinuria, anemia, and a higher Acute Physiology and Chronic Health Evaluation score were associated with recurrent AKI [12,13]. Non-recovery of renal function following any AKI episode was a particularly important risk factor for a further AKI episode [14].
However, most of the available epidemiological studies on recurrent AKI were conducted in the western world by using hospital-based data, which are inevitably confounded by variations of the local hospitalization and admission rate. The objective of our present study is to determine the incidence, severity, and short-term outcome of AKI amongst patients admitted to a general hospital in Hong Kong. We specifically examined the incidence and risk factors of recurrent AKI in hospitalized patients. Since the public hospital system in Hong Kong provides the health care of over 95% of the population, our study would provide representative data on the incidence of AKI in community patients and help the planning of renal service provision.
Patients and Methods
This is a retrospective study approved by the Joint Chinese University of Hong Kong-New Territories East Cluster Clinical Research Ethics Committee. All study procedures were in compliance with the Declaration of Helsinki. We reviewed all adult patients admitted to the Prince of Wales Hospital, Shatin, Hong Kong in 2011 by retrieving the following data from the hospital electronic patient record: sex, date of birth, date of admission, discharge date, admission department, major comorbid conditions, and admission diagnosis.
Serum creatinine levels checked within 3 months prior to admission, during the hospital stay and within 90 days after hospital discharge were retrieved. For each hospital admission, the following serum creatinine parameters were determined: (1) Best serum creatinine prior to admission; (2) Serum creatinine on admission; (3) Peak serum creatinine during hospital admission; (4) Best serum creatinine since presentation; and (5) The last serum creatinine within 90 days after hospital discharge.
Case Definitions
Estimated Glomerular Filtration Rate (GFR) was calculated by the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation [15]. Since the information on urine output was not available from the hospital electronic patient record, the occurrence of AKI was defined only by the creatinine criteria of the Kidney Disease: Improving Global Outcomes (KDIGO) AKI guideline [1]. In essence, subjects who had increased in serum creatinine by 26.5µmol/l from baseline, or had increased in serum creatinine to 1.5 times of baseline were defined to have an episode of AKI. Subjects who had ≥2 times and <3 times increase in serum creatinine were classified as stage 2 AKI, while those with ≥3 times increase in serum creatinine were classified as stage 3 AKI.
In addition, the following patterns of AKI were determined: (1) AKI on admission, defined by comparing serum creatinine upon admission with the level prior to admission if available, or the best serum creatinine ever achieved if there is no serum creatinine level prior to admission was available; (2) AKI during hospitalization, defined by comparing the peak serum creatinine during hospital admission with the one checked upon admission; and (3) Mixed type, when an episode has both components.
Outcome measures
For all AKI episodes, the following outcome parameters were retrieved: need of temporary dialysis, admission to the Intensive Care Unit (ICU), duration of hospital stay, the in-patient mortality, and 30-day mortality. The outcomes of an AKI episode was determined by comparing the best serum creatinine within 90 days after discharge and were classified into 3 categories: (1) Episodes that had the best serum creatinine <1.2 times of baseline creatinine were defined as complete recovery; (2) Episodes that had the best serum creatinine >80% of peak serum creatinine were defined as no recovery; and (3) Episodes that had the best serum creatinine levels in between were classified as partial recovery.
Statistical analysis
Statistical analysis was performed by IBM SPSS Statistics software version 24.0 (IBM, Armonk, NY). All data were expressed as mean ± standard deviation or median (Inter-Quartile Range [IQR]) as appropriate. Data between groups were compared using Chi square test, Student’s t-test, or one way Analysis of Variance (ANOVA) as appropriate. A p value of less than 0.05 was considered significant. All probabilities were two-tailed.
Results
In 2012, there were a total of 146,956 episodes of hospital admissions to the Prince of Wales Hospital, including 50,409 admissions through the emergency department, 87,200 elective admissions, 7219 newborn, and 2,128 episodes transferred from other hospitals. Amongst these admissions, 21,439 episodes belonged to the pediatric group and were excluded from analysis. The remaining 125,517 admissions belonged to the adult population and were analysis.
From October 2011 to March 2013, we identified 618,885 subjects who had serum creatinine checked and recorded under the Hong Kong Hospital Authority database, of which 59551 subjects had 2 or more serum creatinine levels checked. When the serum creatinine database was merged with the hospitalization data, we identified 11456 episodes (9.1%) of AKI among all the hospital admissions in 2012. Specifically, stage 1 AKI was present in 8257 episodes (6.6%) of all hospital admissions, and stage 2 to 3 AKI was present in 3199 episodes (2.5%). Their baseline demographic information is summarized in table 1. According to the Hong Kong population census in 2011 [16], the catchment area of the Prince of Wales Hospital had a population of 630,273, of which 523,831 were adults. The population-based annual incidence of AKI was 2.2% for all stages, 1.6% for stage 1, and 0.6% for stage 2 or 3 AKI.
|
|
All Episodes |
Stage 1 |
Stage 2 |
Stage 3 |
P Value |
|
No. of episode |
11456 |
8257 |
2216 |
983 |
|
|
No. of patients |
6280 |
5100 |
1594 |
740 |
|
|
Male sex (%) |
3498 (55.7%) |
2852 (55.9%) |
852 (53.5%) |
417 (56.4%) |
p=0.2 |
|
Age (year) |
71.9±15.9 |
72.3±15.8 |
72.9±15.4 |
71.6±15.4 |
p=0.2 |
|
Serum creatinine (µmol/L) |
|
|
|
|
|
|
Baseline |
111.6±96.1 |
117.8±99.0 |
96.1±90.8 |
94.8±74.7 |
p<0.0001 |
|
Admission |
190.7±174.4 |
169.9±133.5 |
201.6±199.9 |
341.4±296.9 |
p<0.0001 |
|
Peak |
207.2±191.9 |
175.9±140.5 |
225.9±217.9 |
427.6±314.9 |
p<0.0001 |
|
Follow-up at 90-day |
178.7±189.4 |
163.2±149.5 |
182.0± 15.5 |
301.1±329.9 |
p<0.0001 |
|
Types of AKI, no. of episode (%) |
|
|
|
|
p<0.0001 |
|
Present at admission |
4914 (42.9%) |
3549 (43.0%) |
950 (42.9%) |
415 (42.2%) |
|
|
Developed during hospital stay |
1138 (9.9%) |
434 (5.3%) |
357 (16.1%) |
347 (35.3%) |
|
|
mixed |
5404 (47.2%) |
4274 (51.8%) |
909 (41.0%) |
221 (22.5%) |
|
|
Outcomes, no. of cases (%) |
|
|
|
|
p<0.0001 |
|
Complete recovery |
8391 (73.2%) |
6487 (78.7%) |
1434 (64.7%) |
457 (46.5%) |
|
|
Partial recovery |
1131 (9.9%) |
423 (5.1%) |
438 (19.8%) |
270 (27.5%) |
|
|
No recovery |
1934 (16.9%) |
1334 (16.2%) |
344 (15.5%) |
256 (26.0%) |
|
Table 1: Baseline demographic and clinical information.
Amongst the 3199 episodes of stage 2 or 3 AKI, 1,806 episodes (56.4%) were admitted to the medical unit, 507 episodes (15.8%) to the surgical unit, and 434 episodes (13.6%) to the oncology unit (Figure 1). In total, 72 episodes (2.2%) required acute dialysis initiated in the Intensive Care Unit (ICU), 67 (2.1%) had temporary hemodialysis initiated outside ICU, and 5 episodes (0.2%) received acute peritoneal dialysis. Amongst the stage 2 or 3 AKI episodes, pre-existing diabetes, hypertension, and ischemic heart disease were present in 915 (28.6%), 1592 (49.7%), and 842 (26.3%) patients, respectively; 868 patients (27.1%) received angiotensin converting enzyme inhibitor or angiotensin receptor blocker therapy prior to the onset of AKI. Recent exposure to iodinated contrast was documented in 343 episodes (10.7%), and recent use of Non-Steroidal Anti-Inflammatory Drugs (NSAID) was noted in 255 episodes (8.0%). Active glomerulonephritis was diagnosed in 57 patients (1.8%).
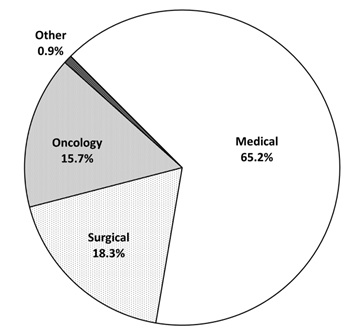 Figure 1: Distribution of specialties amongst patients who had stage 2 or 3 acute kidney injury (AKI).
Figure 1: Distribution of specialties amongst patients who had stage 2 or 3 acute kidney injury (AKI).
Outcome and recurrent AKI
The clinical outcome is summarized in table 1. The median length of hospital stay of the episodes with stage 2 to 3 AKI was 8 days (IQR 4 to 16 days). For the episodes with stage 2 to 3 AKI, 2,203 (68.9%) had complete recovery, 551 (17.2%) had partial recovery within 90 days, and 445 (13.9%) had no recovery of kidney function. The in-patient mortality of stage 2 or 3 AKI was 13.0%, 90-day mortality was 27.3%, 1-year mortality was 47.3%, and 2-year mortality was 57.3%. Ten patients (0.5%) developed end stage kidney disease and required long term dialysis.
Amongst the 6280 patients, 2326 (37.0%) developed recurrent episodes of AKI, and 1129 (18.0%) had more than one recurrent episodes (Figure 2). The characteristics of patients with and without recurrent AKI episode are compared and summarized in table 2. The distribution of time to the recurrent AKI episode is summarized in figure 3. The median time to the recurrent AKI episode was 26 days (IQR 12 to 58 days); 55.7% of the recurrent AKI episodes developed within 30 days of the original episode, and 76.2% of the recurrent episodes within 60 days.
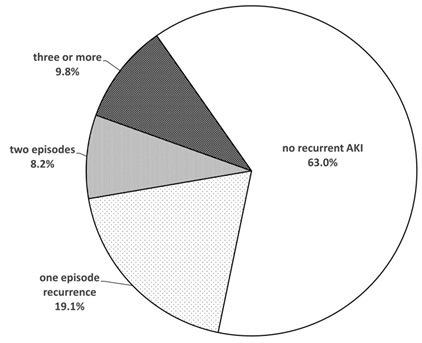 Figure 2: Number of recurrent acute kidney injury (AKI) episodes after the index episode.
Figure 2: Number of recurrent acute kidney injury (AKI) episodes after the index episode.
|
|
No Recurrent AKI |
With Recurrent AKI |
P Value |
|
No. of patients |
3954 |
2326 |
|
|
Male sex, no. of case (%) |
2216 (56.0%) |
1282 (55.1%) |
p=0.5 |
|
Age (year) |
70.8±16.3 |
73.9±15.0 |
p<0.0001 |
|
AKI stage, no. of case (%) |
|
|
p<0.0001 |
|
stage 1 |
3016 (76.3%) |
1652 (71.0%) |
|
|
stage 2 |
630 (15.9%) |
493 (21.2%) |
|
|
stage 3 |
308 (7.8%) |
181 (7.8%) |
|
|
Types of AKI, no. of episode (%) |
|
|
p=0.003 |
|
present at admission |
1261 (31.9%) |
777 (33.4%) |
|
|
developed during hospital stay |
279 (7.1%) |
211 (9.1%) |
|
|
mixed |
2414 (61.1%) |
1338 (57.5%) |
|
|
Outcomes, no. of cases (%) |
|
|
p<0.0001 |
|
Complete recovery |
3022 (76.4%) |
1982 (85.2%) |
|
|
Partial recovery |
326 (8.2%) |
167 (7.2%) |
|
|
No recovery |
606 (15.3%) |
177 (7.6%) |
|
Table 2: Comparison of characteristics between patients with and without recurrent AKI.
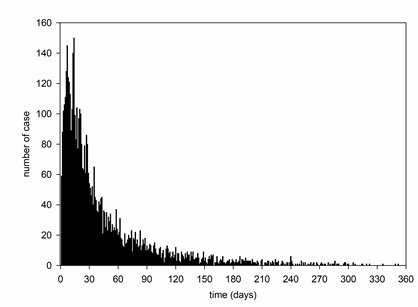 Figure 3: Time lapse from the resolution of the previous acute kidney injury (AKI) episode to the onset of the recurrent episode.
Figure 3: Time lapse from the resolution of the previous acute kidney injury (AKI) episode to the onset of the recurrent episode.
Discussion
In this study, we found that AKI is present in 9.1% of all adult hospital admissions, with a population incidence of 2.2 episode per 100-patient-years of follow up. Moreover, 37% patients developed recurrent AKI episodes, and over 30% episodes of stage 2 or 3 AKI did not have complete recovery.
The incidence of AKI in our study is similar to previous reports [6-9,17-20]. Nonetheless, it is important to note that the reported incidence of AKI varies considerably between studies because of difference in study design as well as various confounding factors [6,17-19]. For example, some studies attempted to use diagnostic coding to detect the incidence of AKI, but this approach has a low sensitivity and underestimates the true incidence [20]. In our present study, AKI episodes were defined by the change in serum creatinine level and the data were retrieved from the electronic health record system in order to ascertain complete case identification. We did not use the urine output criteria because the record of urine output in general wards were often incomplete, so that “oliguria” tended to be over-diagnosed. We did not use ICD coding to detect AKI episodes because the coding “acute renal failure” or “acute kidney injury” were usually not keyed in by the responsible clinicians as the coding does not affect doctor reimbursement or allocation of healthcare resource.
Our study provides reliable but possibly slightly over-estimated data on the epidemiology of AKI in Hong Kong. The catchment area of our hospital covers around 10% of the Hong Kong population, and the Hong Kong Hospital Authority provides 95% of all medical service. On the other hand, our hospital is also a tertiary referral center for major trauma, neurosurgical, cardiothoracic and complicated abdominal surgical patients-all of them had a high risk of AKI. For our study, we believe the incidence of AKI in patients admitted to medical ward should be an accurate estimate for the general population, but that for surgical patients needs to be adjusted by a larger denominator.
In this study, we found around 37% of patients developed recurrent AKI episodes after recovery from a previous AKI episode. It is important to note that the incidence of recurrence may be underestimated in our study because recurrent episodes within the same hospital stay may be missed. The incidence we found is therefore higher than 23% to 31% as described in previous reports [12,13]. We believe the discrepancy could be explained by our exhaustive effort of retrieving serum creatinine levels for at least 3 months after the initial AKI episode, and, being a tertiary referral center of cardiothoracic, neurological and complex abdominal surgery, a high propensity of taking care of patients who required repeated intervention radiological and surgical procedures. The latter consideration would also explain the short delay to the development of a recurrent AKI episode (median 26 days, and over 75% within 2 months) in our study as compared to the report of Liu et al. [12].
The result of our study implies that therapeutic strategies should be developed the prevention of recurrent AKI episodes, which is a neglected area of research to date. Although we found that advanced age is a risk factor of recurrent AKI, the absolute difference in age between patients with and without recurrent AKI was small (Table 2). Contrary to our expectation, patients with no recovery from the AKI episode were less likely to develop a recurrent episode. We believe this is related to our clinical practice and case identification. In essence, patients without recovery were more likely to stay in the hospital and any further loss of renal function would be counted as one episode by our definition.
There are several inadequacies of our present study. First, our case identification is based on fluctuation in serum creatinine level. AKI episodes admitted with a poor kidney function but no baseline serum creatinine level to compare with and no recovery of renal function would not be recognized by our algorithm of case identification. Second, similar to many published studies that are based on electronic database, the cause of AKI episodes could not be ascertained in our study. Because the data on background comorbidity and concomitant drug usage came from our electronic health care record, it was probable that the information was incomplete. The input of diagnosis coding for comorbid conditions were often not exhaustive, and, in Hong Kong, many medications (notably non-steroidal anti-inflammatory drugs and anti-hypertensive drugs) are available over-the-counter without a prescription record. Further study with direct chart review would be necessary to determine the scope of this problem.
In summary, we found that AKI was present in 9.1% of all adult hospital admissions in Hong Kong, and the population incidence was 2.2 episode per 100-patient-years. More importantly, a substantial proportion of patients developed recurrent AKI episodes or did not have complete recovery. Further research should be directed to the identification of risk factors and prevention measures for AKI recurrence.
Acknowledgement
This work was supported in part by the Chinese University of Hong Kong research accounts 6905134 and 7101215. The funders do not have any role in study design, data collection, analysis, result interpretation, report writing, or the decision to submit the report for publication. The results presented in this paper have not been published previously in whole or part. All authors declare no conflict of interest.
References
- Khwaja A (2012) KDIGO Clinical practice guidelines for acute kidney injury. Nephron Clin Pract 120: 179-184.
- Li PKT, Burdmann EA, Mehta RL (2013) Acute kidney injury: Global health alert. Kidney Int 83: 372-376.
- Rifkin DE, Coca SG, Kalantar-Zadeh K (2012) Does AKI truly lead to CKD? J Am Soc Nephrol 23: 979-984.
- Lafrance JP, Miller DR (2010) Acute kidney injury associates with increased long-term mortality. J Am Soc Nephrol 21: 345-352.
- Hsu CY, Chertow GM, McCulloch CE, Fan D, Ordoñez JD, et al. (2009) Nonrecovery of kidney function and death after acute on chronic renal failure. Clin J Am Soc Nephrol 4: 891-898.
- Lafrance JP, Miller DR (2010) Defining acute kidney injury in database studies: The effects of varying the baseline kidney function assessment period and considering CKD status. Am J Kidney Dis 56: 651-660.
- Ali T, Khan I, Simpson W, Prescott G, Townend J, et al. (2007) Incidence and outcomes in acute kidney injury: A comprehensive population-based study. J Am Soc Nephrol 18: 1292-1298.
- Susantitaphong P, Cruz DN, Cerda J, Abulfaraj M, Alqahtani F, et al. (2013) World incidence of AKI: A meta-analysis. Clin J Am Soc Nephrol 8: 1482-1493.
- Hsu CY, McCulloch CE, Fan D, Ordoñez JD, Chertow GM, et al. (2007) Community-based incidence of acute renal failure. Kidney Int 72: 208-212.
- Rodríguez E, Arias-Cabrales C, Bermejo S, Sierra A, Burballa C, et al. (2018) Impact of recurrent acute kidney injury on patient outcomes. Kidney Blood Press Res 43: 34-44.
- Kaul A, Bhadauria D, Prasad N, Gupta A, Sharma RK (2018) Recurrent acute kidney injury in tropics-epidemiology and outcomes. J Assoc Physicians India 66: 18-21.
- Liu KD, Yang J, Tan TC, Glidden DV, Zheng S, et al. (2019) Risk factors for recurrent acute kidney injury in a large population-based cohort. Am J Kidney Dis 73: 163-173.
- Hounkpatin HO, Fraser SDS, Glidewell L, Blakeman T, Lewington A, et al. (2019) Predicting risk of recurrent acute kidney injury: A systematic review. Nephron 142: 83-90.
- Holmes J, Geen J, Williams JD, Phillips AO (2019) Recurrent acute kidney injury: Predictors and impact in a large population-based cohort. Nephrol Dial Transplant 35: 1361-1369.
- Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF et al. (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150: 604-612.
- Census and Statistics Department (2020) The Government of the Hong Kong Special Administrative Region. 2011 Population Census.
- Liaño F, Pascual J (1996) Epidemiology of acute renal failure: A prospective, multicenter, community-based study. Madrid Acute Renal Failure Study Group. Kidney Int 50: 811-818.
- Obialo CI, Okonofua EC, Tayade AS, Riley LJ (2000) Epidemiology of de novo acute renal failure in hospitalized African Americans: comparing community-acquired vs. hospital-acquired disease. Arch Intern Med 160: 1309-1313.
- Wang Y, Cui Z, Fan M (2005) Retrospective analysis on Chinese patients diagnosed with acute renal failure hospitalized during the last decade (1994-2003). Am J Nephrol 25: 514-519.
- Waikar SS, Wald R, Chertow GM, Curhan GC, Winkelmayer WC, et al. (2006) Validity of international classification of diseases, ninth revision, clinical modification codes for acute renal failure. J Am Soc Nephrol 17: 1688-1694.
Citation: Pang WF, Li PKT, Chan MHM, Ho PWL, Chan GCK, et al. (2021) Incidence, Severity, and Short-Term Outcome of Acute Kidney Injury in Hospital Admissions of Hong Kong. J Nephrol Renal Ther 7: 063.
Copyright: © 2021 Wing-Fai Pang, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

