
Influence of Antenatal Health Care Visit on modern Contraceptive Use among Postpartum Women in Ghana
*Corresponding Author(s):
Desmond KluInstitute Of Health Research, University Of Health And Allied Sciences, PMB 31, Ho-Volta Region, Ghana
Tel:+233 241596523,
Email:kludesmond12@gmail.com
Abstract
Background: Antenatal health care visit and the use of contraceptives are important issues in maternal and child well-being. However, there is paucity of research on the changes in contraceptive use among postpartum women who are regularly exposed to contraceptive education and counselling during attendance at antenatal clinics and the factors contributing to these changes in contraceptive behaviour. Therefore, the aim of this study is to track the changes in contraceptive use among postpartum women who visit antenatal clinics in Ghana using a national representative cross-sectional survey 2003 to 2014 and to discuss the factors contributing to these changes.
Methods: The study used three rounds of the Ghana Demographic and Health Survey conducted in 2003, 2008 and 2014. Postpartum women in their reproductive ages 15-49 who had given birth within the last 0-23 months were selected for this study. Binary logistic regression model was used to examine the influence of antenatal visits and socio-demographic factors on modern contraceptive use over the years.
Results: Results suggest that increased in modern contraceptive use was positively correlated with women visiting antenatal health care centres four or more times and women residing in urban areas but negatively correlated with increasing age, no education and married women.
Conclusion: In Ghana utilisation of maternal health care services has the ability to influence high contraceptive use among postpartum women. However, demographic, social and economic factors have influenced changes in contraceptive use among women in Ghana and must also be taken into a consideration in policy formulation.
Keywords
Antenatal visit; Contraceptive use; Ghana; Health; postpartum women
BACKGROUND
Antenatal health care and the use of contraceptives are important issues in maternal and child well-being [1]. Antenatal health care improves the survival and health of babies directly by reducing stillbirths and neonatal deaths and indirectly by providing an entry point for health contacts with the woman at a key point in the continuum of care. Globally, the proportion of women receiving ANC at least once during pregnancy was 83 per cent during the period 2007-2014 [2]. However, only 64 per cent of pregnant women received the recommended minimum of four visits [2]. In sub-Saharan Africa, 77 per cent of pregnant women have at least one antenatal care visit WHO, 2015 [2]. In Ghana, 70 per cent of women reported four or more antenatal visits [3]. Antenatal care is considered part health care setup which is part of services provided at local health facility such as Community-based Health Planning and Services (CHPS) in the case of Ghana [4,5].
One of the means to ensuring safe motherhood and good sexual and reproductive health outcome is using modern contraceptives; therefore, there is a relationship between contraceptive use and antenatal health care service utilisation. Furthermore, modern contraceptive use among postpartum mothers leads to the prevention of unintended pregnancy and healthy birth spacing [6,7]. This is possible through frequent visit to antenatal health care centres which serve as one of the major sources of information about contraceptives. It also serves as an appropriate time for women to begin considering using contraceptives based on informed choices. The uptake of antenatal health care service helps to ensure that women have an understanding of how quickly their ovulation may return after birth and the risks associated with closely-spaced pregnancies and how this can be prevented through the effective use of modern contraceptives [8]. Other services provided at antenatal clinics include, ultrasound scan, laboratory testing for HIV, Malaria and Haemoglobin (Hb) checking to detect anaemia, dispensing services and education on pregnancy and pregnancy related issues.
Despite the number of studies on contraceptive use among postpartum women who utilize maternal health care services [6,9-19], there are still some gaps in understanding contraceptive behaviour among these women. Thus, what is missing in the literature are the changes in contraceptive use among postpartum women who are regularly exposed to contraceptive education and counselling during attendance at antenatal clinics and the factors contributing to these changes in contraceptive behaviour. Therefore, the aim of this study is to track the changes in contraceptive use among postpartum women who utilise antenatal health care services in Ghana using a national representative cross-sectional survey (Ghana Demographic and Health Survey) 2003 to 2014 and to discuss the factors contributing to these changes. This paper seeks to contribute to knowledge and literature by examining the trends in modern contraceptive use among women utilising antenatal health care services from 2003 to 2014. This paper will therefore contribute to knowledge by providing insight and helping to understand the contraceptive use among postpartum women over the years that regularly have contact with the health care system and have the highest unmet need for limiting and spacing birth. Again, this paper will contribute to achieving Sustainable Development Goal target (3.7) of ensuring universal access to sexual and reproductive health issues including family planning, information and education as well as integrating sexual and reproductive health issues into national strategies and programmes. It will also contribute to achieving Ghana’s Population Policy goal of 50 per cent contraceptive prevalence rate by 2050 at its current of 27 per cent [20].
METHOD
Sources of data
The study used three rounds of the Ghana Demographic and Health Survey conducted in 2003, 2008 and 2014. The Ghana Demographic and Health Survey is a nationally representative cross-sectional survey which collects information on issues such as housing characteristics and household population, marriage and sexuality, fertility and fertility preferences, family planning, infant and child mortality, maternal health, child and early development. It further includes issues on nutrition of children and women, malaria, HIV and AIDS related knowledge, attitudes, and behaviour, HIV prevalence, adult health and lifestyle, women empowerment and demographic and health outcomes. For the purpose of this study, data on antenatal visit, and modern contraceptive use by postpartum women were used to establish a relationship among these three reproductive health concepts. The rationale for using such data is as follows that at the International Conference on Population and Development (ICPD) held in 1994 Cairo-Egypt, Ghana endorsed the Programme of Action of the ICPD and adopted the ICPD definition of reproductive health which has safe motherhood, family planning and other reproductive health issues as its key components.
Sample used
Postpartum women in their reproductive ages 15-49 who had given birth within the last 0-23 months were selected for this study. This enabled the research to fully examine the relationships among the two variables of interest (ANC visit and modern contraceptive use). Thus, the months following birth, these women are likely to be in close contact with the maternal health care system and will also be more exposed to family planning or contraceptive counselling, hence may influence their contraceptive use and behaviour.
Second, these are women with the highest unmet need for family planning [13,21]. This is further consistent with studies that have found that two-thirds of postpartum women within one year of their last birth have an unmet need for family planning [22,23]. In all the three rounds of the GDHS conducted in 2003, 2008 and 2014, women who had their last birth preceding each survey year and observing up to 23 months of postpartum were extracted from the data. The number of eligible women for the three separate surveys is presented in table 1 (see appendices).
|
Survey Year |
Number of eligible women |
|
GDHS 2003 |
1,421 |
|
GDHS 2008 |
1,178 |
|
GDHS 2014 |
2,264 |
|
Total |
4,863 |
Table 1: Eligible women in the GDHS by year.
Source: Generated from Ghana Demographic Health Survey Data (GSS et al., 2004, 2009, 2015)
Methods of analysis
The analysis comprises the description of the variables of interest using frequency and per centage distribution tables, diagrams and charts such as bar graphs and pie-charts. It consists of the number of women who visit antenatal clinics and uses modern contraceptives. It further describes the background characteristics of women including their current age, educational level, and that of their partners, the number of living children (parity), their place of residence, ethnicity, current marital status, fertility intentions, and sexual activity after birth, exposure to family planning information in the media, sex of the head of household and household wealth quintile. This is intended to understand the socio-demographic and economic characteristics of these women as they relate to the two variables of interest (ANC visits and modern contraceptive use).
The bivariate analysis used in this study was to determine the empirical relationship between the variables of interest (ANC visit and modern contraceptive use). Thus, the analysis at this stage seeks to explain the relationships that exist between these variables on one hand and the dependent variable on the other. Again, a chi-square analysis was done relating the control variables (maternal age, woman’s educational level, partner’s educational level, the number of living children (parity), place of residence, religion, marital status, fertility intention and exposure to family planning information in the media to the dependent variable (modern contraceptive use) within the context of antenatal health care service utilisation.
The third stage of analysis specifically uses the binary logistic regression model. The purpose for using this model is because the outcome variable was categorized into two; those who use modern contraceptives and those who do not. Binary logistic regression model was used to identify variables independently associated with modern contraceptive use in the three different survey years. Thus, this regression model was adopted to determine the strength of relationship between modern contraceptive use and number of antenatal visits while other variables are controlled for. The first model analyses the likelihood of modern contraceptive use among postpartum women who attended antenatal clinics in the three survey years. The last model examined the likelihood of modern contraceptive use among postpartum women who visit antenatal health clinics for the three survey years while controlling for their background characteristics (GDHS 2003, 2008 & 2014).
The general binary logistic regression model that was used for the multivariate analyses is as follows:
 Where;
Where;
P=Probability of modern contraceptive use (1 if using, else 0)
χ1-χn= Main predictor variable [Key independent variable- ANC visits] and selected socio-demographic (individual and household) characteristics.
βo, β1…...βn= Regression coefficients
Measurement of variables
The main independent variable is the uptake of antenatal health care services. The study used this statement to measure this variable:
- Whether a woman received antenatal health care services and the number of times she visits health centres for antenatal care (antenatal visits) [No Visit=1; 1-3 Visits=2; 4 or more Visits=3]
The dependent variable of interest in this study is modern contraceptive use after the last childbirth. The information came from the birth and contraceptive use calendar included in the Demographic and Health Survey women’s questionnaire which records month-by-month all events related to pregnancy, pregnancy outcomes, child breastfeeding, and contraceptive use for 60 months before the survey.
For the categorization of modern contraceptive use, women who are using modern contraceptives were included. The modern contraceptive methods for this study include pills, intrauterine device, injections, diaphragm, condom (male and female), female sterilization, norplant and foam or jelly). However, women who used only traditional methods of contraceptives such as withdrawal were taken out of the sample. The reason is that, over the years the proportion of women using traditional methods of contraception has been declining in Ghana. According to statistics from the Ghana Demographic and Health Survey (1988-2014), the proportion of postpartum women using traditional contraception declined from 10 per cent in 1988 to 4.2 per cent in 2014 [20]. Because of the relatively small proportions in postpartum women using traditional methods, doing separate analyses would not have been meaningful. The measurement of the intermediate variable of contraceptive counselling was done in the qualitative data collection. For the purposes of this study socio-demographic characteristics of women were considered as control variables.
Ethics
The ICF (Inner City Fund) Institutional Review Board (IRB) and Ghana Health Service Ethical Review Committee approved the protocol for the 2003, 2008 and 2018 GMHSs conducted by Ghana Statistical Service. However, ethical approval was not needed for this study since it involved secondary data analysis devoid of personal identifies to women and their households. Nonetheless, the researcher obtained permission from ICF for the use of the datasets and the terms of use have been strictly adhered to
RESULTS: DESCRIPTIVE
Trend in antenatal care services uptake among postpartum women in Ghana
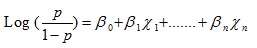
Figure 1 (see appendices) illustrates the proportion of postpartum women who did not utilize antenatal health care services, those who utilized in 2003, 2008 and 2014 in Ghana. 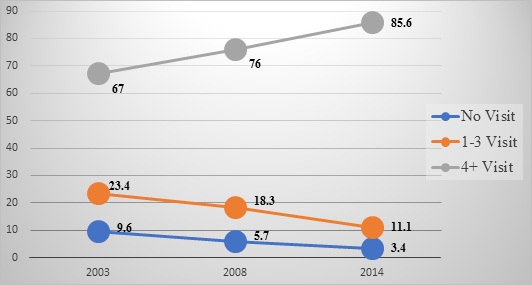 Figure 1: Trend in antenatal health care visit among postpartum women in Ghana (%).
Figure 1: Trend in antenatal health care visit among postpartum women in Ghana (%).
Source: computed by author using the GDHS 2003, 2008, 2014.
It is seen from figure 1 that; the proportion of postpartum women did not visit health centres for antenatal care has been low. Specifically, this low proportion in 2003, 2008 and in 2014 is represented by 9.6 per cent, 5.7 per cent and 3.4 per cent respectively. Thus, there has been a consistent decline in the proportion of postpartum women who are not visiting health centres for antenatal care. This phenomenon may be explained by the introduction of the free maternal health policy, changing attitudes of antenatal health care personnel [24], health insurance and educational attainment of women [25]. Other reasons are the positive perception of women on antenatal health care as normal part of pregnancy and after birth [26].
Similar observation of could be made among postpartum women who reported visiting antenatal clinic 1-3 times. It declined from 23.4 per cent in 2003 to 18.3 per cent in 2008 and further declined to 11.1 per cent in 2014. For postpartum women who visit antenatal clinics four or more times, the results indicated an increase in the proportion from 67 per cent in 2003 to 76 per cent in 2008 and further increased to85.6 per cent in 2014.In general, between the survey years (2003-2014), the proportion of postpartum women who had four or more visits to health centres for antenatal care in Ghana has been generally high. The possible explanation for this phenomenon may be increasing skilled health care personnel [27] and increasing trust in the health care system [15]. In summary, the trend analysis shows that there has been a high uptake of antenatal health care services among women with four or more visits.
Trend in Contraceptive use among postpartum women in Ghana (2003-2014)
Contraception plays an essential role in the reproductive health of women during their postpartum period as it aids in preventing unwanted pregnancy and reducing mortality among children and their mothers [28-30]. This is possible through delaying subsequent births and lengthening pregnancy intervals. Figure 2 discusses the trend in modern contraceptive use among postpartum women in Ghana. The general observation is that throughout the three survey years (2003, 2008 & 2014), the trend in the proportion of postpartum women using modern contraceptives declined from 15.3 per cent in 2003 to 14.3 per cent in 2008 before increasing to 21 per cent in 2014. Despite this increasing trend in modern contraception among women observing postpartum over the years, this is relatively lower compared to contraceptive prevalence rate among women which stand at 27 per cent.
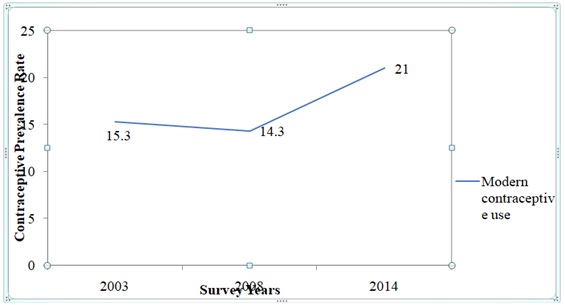 Figure 2: Trend in Contraceptive use among Postpartum Women in Ghana (2003-2014).
Figure 2: Trend in Contraceptive use among Postpartum Women in Ghana (2003-2014).
Source: computed by author using the GDHS 2003, 2008, 2014
Background characteristics of postpartum women in Ghana
Table 2 discusses the background characteristics of postpartum women in Ghana using data from Ghana’s Demographic and Health Surveys (2003, 2008 & 2014). Table 2 indicates that in all the three surveys, a relatively higher proportion of postpartum women were within the age group 15-29 years: 55.4 per cent in 2003, 59.5 per cent in 2008 and 52.9 per cent in 2014 compared to other age categories. This outcome is expected because studies on childbirth among women have consistently found a higher proportion of births to be mostly occurring among women of 15-29 years. Other studies especially within sub-Saharan African countries indicate the proportion of women likely to give birth and observing postpartum at the same time is most likely to be higher among the 15-29 groups [31,32]. On the other hand, postpartum women with the least proportion in all three surveys were recorded in age group 40-49 years. This may be because women within the age group 40-49 years may be entering their menopause and so only a small per centage of them may still be giving birth.
|
Background characteristics |
2003 |
2008 |
2014 |
|
Current age |
N (%) |
N (%) |
N (%) |
|
15-29 |
788 (55.4) |
700 (59.5) |
1198 (52.9) |
|
30-39 |
522 (36.7) |
392 (33.3) |
895 (39.5) |
|
40-49 |
112 (7.9) |
85 (7.2) |
171 (7.5) |
|
Maternal education |
|||
|
No Education |
572 (40.3) |
363 (30.8) |
606 (26.8) |
|
Primary |
322 (22.7) |
288 (24.5) |
431 (19.0) |
|
Secondary+ |
526 (37.0) |
526 (44.7) |
1227 (54.2) |
|
Partner’s Education |
|||
|
No Education |
514 (36.2) |
310 (26.4) |
487 (21.5) |
|
Primary |
116 (8.2) |
110 (9.4) |
415(18.4) |
|
Secondary+ |
790 (55.6) |
757 (64.3) |
1361 (60.1) |
|
Parity |
|||
|
1-2 |
668 (47.0) |
592 (50.2) |
1091 (48.2) |
|
3-4 |
408 (28.7) |
370 (31.4) |
700 (30.9) |
|
5+ |
345 (24.3) |
216 (18.4) |
473 (20.9) |
|
Place of residence |
|||
|
Urban |
477 (33.5) |
455 (38.6) |
1009 (44.6) |
|
Rural |
944 (66.5) |
723 (61.4) |
1255 (55.4) |
|
Religion |
|||
|
Catholic |
172 (21.1) |
147 (12.5) |
217 (9.6) |
|
Protestant |
205 (14.5) |
149 (12.7) |
278 (12.3) |
|
Pentecostal/Charismatic |
623 (43.8) |
546 (46.4) |
1193(52.7) |
|
Moslem |
268 (18.9) |
218 (18.5) |
412 (18.2) |
|
Traditional |
58 (4.1) |
68 (5.7) |
75 (3.3) |
|
No Religion |
94 (6.6) |
49 (4.2) |
88 (3.9) |
|
Marital status |
|||
|
Never Married |
52 (3.9) |
81 (6.9) |
203 (9.0) |
|
Currently Married |
1289 (90.7) |
1052 (89.4) |
1967 (86.9) |
|
Formerly Married |
80 (5.6) |
44 (3.7) |
93 (4.1) |
|
Fertility intention |
|||
|
Have Another |
893 (62.9) |
778 (66.1) |
1319 (58.3%) |
|
Undecided |
39 (2.7%) |
54 (4.6%) |
217 (9.6%) |
|
No More |
488 (34.4%) |
346 (29.3%) |
727 (32.1%) |
|
Exposure to FP info in the media |
|||
|
Yes |
530 (37.3%) |
434 (36.9%) |
896 (39.6%) |
|
No |
891 (62.7%) |
743 (63.1%) |
1368 (60.4%) |
Table 2: Per centage distribution of background characteristics of postpartum women in Ghana 2003, 2008 and 2014.
Source: Computed by author using the GDHS 2003, 2008, 2014; N=Number of Postpartum Women; %=Per cent; Secondary+ =secondary and/or higher education
Furthermore, with exception in 2003, the proportion of postpartum women who had attained secondary or higher level of education has been high. This proportion was represented by 44.7 per cent in 2008 and 54.2 per cent in 2014. The proportion of postpartum women who had primary level of education throughout the three survey years was the least that is 22.7 per cent in 2003, 24.5 per cent in 2008 and 19 per cent 2014. The results also show that in the three surveys (2003-2014), the proportion of partners of postpartum women who have secondary or higher level of education have been generally high. Thus, the proportion increased from 55.6 per cent in 2003 to about 60.1 per cent in 2014. Similar trends were observed among partners of postpartum women who have attained primary education even though they constitute the least proportion. On the other hand, the proportion of those who had no formal education has been low between 2003 and 2014. For instance, the proportion of partners of postpartum women who had no formal education was relatively higher in 2003 (36.2%), but a much lower proportion was recorded in 2014 (21.5%). Overall, there has been a general improvement in the level of education attained by partners of postpartum women in Ghana.
Again, a higher proportion of postpartum women with parity 1-2 throughout the survey years compared to other parity categories. More specifically, there has been a general decline in the proportion of postpartum women who had five or more children. Thus, it had a relatively higher proportion of 24.3 per cent in 2003 but in 2008 the proportion was relatively lower (18.4%). However, in 2014 it recorded a relatively higher proportion of 20.9 per cent. Further, a higher proportion of postpartum women had between three to four children both in 2008 (31.4%) and 2014 (30.9%). Throughout the three survey years, majority of postpartum women in Ghana were from the rural areas compared to the urban. This outcome may be as a result of the higher rural fertility compared to the urban fertility.
However, it is worthy to note that throughout the three survey periods, while the proportion of postpartum women who reside in the urban areas is relatively lower (33.5% in 2003; 38.6% in 2008; 44.6% in 2014), the proportion residing in rural areas has been higher, representing 66.5 per cent in 2003, 61.4 per cent in 2008 and 55.4 per cent in 2014. This trend can be explained within the context of Ghana’s urbanization trends. Ghana is becoming increasingly urbanized where the number of urban settlements has with population 5,000 or more increased from 41 in 1984 to 388 in 2015 [20]. This rise in urbanization has been attributed to three demographic processes: rural-urban migration, natural increase in towns and cities (development of peri-urban areas) and re-classification as villages grow into towns once they attain the threshold population of 5000 or more.
With regards to religion, the result indicates majority of the women belong to the Pentecostal/charismatic faith in the three survey years. This is represented by 43.8 per cent in 2003, 46.4 per cent in 2008 and 52.7 per cent in 2014. Least proportion of these women belongs to the traditional religion. The results of the descriptive statistics in table 2 show clearly that an overwhelming majority of postpartum women in Ghana throughout the three surveys are currently married. However, there is a trend towards reduction in the proportion currently married from 2003 to 2014 (from about 91% to about 87% in 2014). Those who were never married and formerly married represented a small proportion of the postpartum women in each of the survey years. What is quite clear is the result that the proportion of women who had never married were lower in 2003 (3.7%) but higher in 2008 and 2014 representing 6.9 per cent and nine per cent respectively.
From table 2, it could clearly be seen that the proportion of postpartum women who have an intention of giving birth to another child was relatively higher in 2003 (62.9%) and in 2008 (66.1%), but was lower in 2014 that is, 58.3 per cent. For those who are undecided on their fertility intentions, the proportion of postpartum women had consistently increased from 2.7 per cent in 2003 to 4.6 per cent in 2008 to about 10 per cent in 2014. The reason for this may probably be due to the fact that fertility decisions are jointly made by women and their partners; hence, the decision of child birth does not lie only in their hands. Furthermore, the results indicate that relatively lower proportion of postpartum women want no more children compared to those who desire to have another child. In addition, smaller proportions (2003:37.3%; 2008:36.9%; 2014:39.6%) of postpartum women in Ghana are exposed to family planning messages compared to those who are not exposed (2003:62.7%; 2008:63.1%; 2014:60.4%). One factor that accounts for this phenomenon is a substantial increase in the ownership of electronic gadgets [33,34].
In conclusion, the key observations reveal higher proportion of postpartum women in the three surveys have four or more visits to health centres for antenatal care. The study further indicated that majority of these women within the ages 15-29 years and has attained secondary or higher level of education. Another important observation was that majority of the women have a desire to give birth to another child and have one to two living children and most of these women also belong to the Pentecostal/charismatic faith Again, most of the women were not exposed to family planning information in the media (Television, radio, newspapers, etc.,). Most importantly, high proportions of these women are currently not using modern methods of contraception.
Association between Antenatal visits, socio-demographic characteristics and modern contraceptive use among postpartum in Ghana
This section examined the associated between number of antenatal visits, women background characteristics and modern contraceptive use. These are presented in table 3 (see appendices). Modern contraceptive use was highest among women who visited antenatal clinics four or more times in 2003 (18.7%), 2008 (15.6%) and 2014 (22.5%) compared to contraceptive use among women with 1-3 antenatal visit and no visits. Thus, there was significant association (p<0.05) between number of antenatal visit and modern contraceptives use in the three years.
|
Variables |
Modern Contraception |
||||||||
|
|
2003 |
2008 |
2014 |
||||||
|
Antenatal Visit |
Not Using (%) |
Using (%) |
P-Value |
Not Using (%) |
Using (%) |
P-Value |
Not Using (%) |
Using (%) |
P-Value |
|
No Visits |
91.9 |
8.1 |
0.000 |
92.5 |
7.5 |
0.044 |
93.5 |
6.5 |
0.000 |
|
1-3 Visits |
91.3 |
8.7 |
89.4 |
10.6 |
86.0 |
14.0 |
|||
|
4+ Visits |
81.3 |
18.7 |
84.4 |
15.6 |
77.5 |
22.5 |
|||
|
Age |
|||||||||
|
15-29 |
85.0 |
15.0 |
0.333 |
86.7 |
13.3 |
0.503 |
75.9 |
24.1 |
0.001 |
|
30-39 |
83.1 |
16.9 |
84.4 |
15.6 |
82.6 |
17.4 |
|||
|
40-49 |
88.4 |
11.6 |
83.7 |
16.3 |
81.3 |
18.7 |
|||
|
Maternal Education |
|||||||||
|
No Edu |
91.4 |
8.6 |
0.000 |
91.8 |
8.2 |
0.000 |
85.6 |
14.4 |
0.000 |
|
Primary |
81.4 |
18.6 |
84.7 |
15.3 |
73.8 |
26.2 |
|||
|
Secondary+ |
79.3 |
20.7 |
82.1 |
17.9 |
77.5 |
22.5 |
|||
|
Partners’ Edu |
|||||||||
|
No Edu |
92.6 |
7.4 |
0.000 |
93.2 |
6.8 |
0.000 |
86.9 |
13.1 |
0.000 |
|
Primary |
78.4 |
21.6 |
80.9 |
19.1 |
74.9 |
25.1 |
|||
|
Secondary+ |
80.3 |
19.7 |
83.4 |
16.6 |
77.4 |
22.6 |
|||
|
Parity |
|||||||||
|
1-2 |
85.0 |
15.0 |
0.771 |
85.8 |
14.2 |
0.477 |
80.0 |
20.0 |
0.007 |
|
3-4 |
83.6 |
16.4 |
84.3 |
15.7 |
75.1 |
24.9 |
|||
|
5+ |
85.2 |
14.8 |
|
88.0 |
12.0 |
|
82.2 |
17.8 |
|
|
Place of residence |
|||||||||
|
Urban |
76.7 |
23.3 |
0.000 |
83.5 |
16.5 |
0.000 |
79.3 |
20.7 |
0.737 |
|
Rural |
88.8 |
11.2 |
87.1 |
12.9 |
78.7 |
21.3 |
|||
|
Religion |
|
|
|
|
|
|
|
|
|
|
Catholic |
84.3 |
15.7 |
0.000 |
80.4 |
19.6 |
0.090 |
77.5 |
22.5 |
0.037 |
|
Protestant |
85.4 |
14.6 |
83.9 |
16.1 |
77.7 |
22.3 |
|||
|
Pentecostal/Charismatic |
80.6 |
19.4 |
85.0 |
15.0 |
77.3 |
22.7 |
|||
|
Moslem |
88.4 |
11.6 |
90.4 |
9.6 |
82.0 |
18.0 |
|||
|
Traditional |
98.3 |
1.7 |
91.2 |
8.8 |
89.3 |
10.7 |
|||
|
No Religion |
91.5 |
8.5 |
85.7 |
14.3 |
85.2 |
14.8 |
|||
|
Marital status |
|||||||||
|
Never Married |
90.4 |
9.6 |
0.184 |
95.1 |
4.9 |
0.005 |
79.3 |
20.7 |
0.815 |
|
Currently Married |
84.1 |
15.9 |
84.5 |
15.5 |
79.1 |
20.9 |
|||
|
Formerly Married |
90.0 |
10.0 |
95.6 |
4.4 |
76.3 |
23.7 |
|||
|
Fertility intention |
|||||||||
|
Have Another |
85.5 |
14.5 |
0.537 |
87.0 |
13.0 |
0.002 |
78.4 |
21.6 |
0.057 |
|
Undecided |
84.6 |
15.4 |
96.3 |
3.7 |
85.3 |
14.7 |
|||
|
No More |
83.2 |
16.8 |
80.9 |
19.1 |
78.1 |
21.9 |
|||
|
Exposure to FP in Media |
|||||||||
|
No |
88.1 |
11.9 |
0.000 |
87.9 |
12.1 |
0.006 |
78.3 |
21.7 |
0.322 |
|
Yes |
79.1 |
20.9 |
82.0 |
18.0 |
80.0 |
20.0 |
|||
Table 3: Association between antenatal visits, socio-demographic characteristics and modern contraceptive use among postpartum in Ghana.
Source: computed by author using the GDHS 2003, 2008, 2014; %=Per cent; Secondary+ =secondary and/or higher education
Regarding age of women and use of modern contraceptives, the association between these two was significant only in 2014, which shows higher modern contraceptive use among women within the age bracket 15-29 relative to other age categories (30-39 and 40-49). With educational level of women, use of modern contraceptives was high among women who attained secondary and higher education compared to women with primary and no formal education in the three survey years which also showed significant association. With respect to educational level of their partners, the practice of modern contraception was most common among partners of women who had attained primary education relative to those who had no formal education and secondary or higher education throughout the three survey years.
Only in 2014 that the association between parity and modern contraception was significant at 0.05 level. The use of modern contraceptives was more prevalent among women who had 3-4 children compared to those who had 1-2 children as well as five or more children. The result further indicates relatively higher modern contraceptive prevalence rate among women who belong to the Pentecostal/Charismatic faith compared to the other religious affiliations in 2003 and 2014. High modern contraceptive use was recorded among women who were currently married relative to those formerly married and single. Contraceptive use tends to be more prevalent among women who do not desire any more children compared to their counterparts who desire another child or undecisive. Modern contraceptive use was higher among women who were exposed to family planning formation in media compared to women who were not.
Influence of number of antenatal visit on modern contraceptive use among postpartum women in Ghana
Table 3 (see appendices) presents the results from the binary regression model used to examine the relationship between the main independent variable (Number of antenatal visits) and modern contraceptive use. The modern contraceptive use variable was dichotomous with ‘1’ representing postpartum women who used modern contraceptives after their last birth preceding the survey, and ‘0’ representing postpartum women who did not use modern contraceptives after their last birth.
DISCUSSION OF RESULTS
The general observation from the regression model in the three survey years is that visiting health centres for antenatal care four or more times was significantly associated with the use of modern contraceptives among postpartum women. This shows a positive relationship between number of antenatal care visit and modern contraceptive use. Specifically, there was a higher probability of modern contraceptive use among postpartum women with four or more visit to antenatal health care centres in Ghana compared to women who had not visited health centres for antenatal care during pregnancy.
Results from table 4 suggest that in 2003, women who reported visiting health care centres for antenatal care four or more times were 2.61 times more likely to use modern contraceptives compared to women with no antenatal visits. Also, in 2014, women with four or more antenatal visits were 4.43 times more likely to use modern contraceptives compared to women with no visits. These findings are consistent with literature which showed that antenatal service intensity was significant in predicting postpartum contraception in Kenya and Zambia [15]. A significant association was established between antenatal health care service utilisation and postpartum contraceptive use in Bangladesh. The study indicated that more than half (62.4%) of the total antenatal care seekers used modern contraceptive methods in Bangladesh [35].
|
Variable |
2003 OR (95%CI) |
2008 OR (95%CI) |
2014 OR (95%CI) |
|
Antenatal visit |
|||
|
No visit (RC) |
1.00 |
1.00 |
1.00 |
|
1-3 Visit |
1.09 (0.53, 2.25) |
1.47 (0.53, 4.04) |
2.42 (0.89, 6.51) |
|
4+ Visit |
2.61 (1.38,4.95) ** |
2.32 (0.92,5.89) |
4.33 (1.71, 10.98) ** |
Table 4: Results of binary logistic regression showing the changes modern contraceptive use among postpartum women in the context of antenatal health care utilisation on in Ghana, 2003, 2008 & 2014.
Note: ***= P value < 0.001; **= pvalue<0.01; * p value<0.05
(RC)=Reference Category; C.I=Confidence Interval
Source: computed by author using the GDHS 2003, 2008 & 2014
There are two possible explanations for the strong association between antenatal care and modern contraceptive use. First, education on contraception is considered an essential component of maternal health care; therefore, women who utilize these services go through contraceptive counselling [36]. Secondly, integrating contraceptive counselling into routine antenatal care gives women the chance to benefit from multiple counselling.
Factors affecting changes in contraceptive use among postpartum women in the context of antenatal health care
This section attempts to examine the demographic, social and economic factors affecting relationship between utilisation of antenatal health services and modern contraceptive use among postpartum women in Ghana. Generally, it could be seen in table 5 (see appendices) that after controlling for the demographic and socio-economic characteristics of the women, only in 2014 was number of antenatal visit significant in predicting modern contraceptive use. This underlines the influence of background characteristics on antenatal health care services and modern contraceptive use.
|
ANC Visit |
2003 OR (95%CI) |
2008 OR (95% C.I) |
2014 OR (95% CI) |
|
No Visit (RC) |
1.00 |
1.00 |
1.00 |
|
1-3 Visit |
0.92 (0.45, 2.05) |
1.39 (0.49,3.93) |
2.77 (1.01, 7.63) * |
|
4+ Visit |
1.76 (0.89,3.47) |
1.67 (0.63,4.42) |
5.00 (1.92,13.03) ** |
|
Maternal age |
|||
|
15-29(RC) |
1.00 |
1.00 |
1.00 |
|
30-39 |
0.93 (0.61,1.41) |
1.09 (0.70,1.72) |
0.56 (0.43, 0.73) ** |
|
40-49 |
0.62 (0.28, 1.34) |
1.68 (0.76,3.68) |
0.70 (0.42,1.16) |
|
Maternal education |
|||
|
No education |
0.64 (0.40,1.41) |
0.56 (0.33,0.95) * |
0.69 (0.49,0.97) * |
|
Primary |
1.09 (0.75,1.60) |
0.91(0.60,1.40) |
1.25 (0.95, 1.65) |
|
Secondary+ (RC) |
1.00 |
1.00 |
1.00 |
|
Partner’s education |
|||
|
No education |
0.54 (0.34, 0.84) ** |
0.55 (0.31, 0.98) * |
0.64 (0.44,0.92) * |
|
Primary |
1.59 (0.94, 2.68) |
1.46 (0.82, 2.58) |
1.38 (0.96,1.96) |
|
Secondary+(RC) |
1.00 |
1.00 |
1.00 |
|
Parity |
|||
|
1-2 |
0.64 (0.35.1.15) |
1.51 (0.75, 3.04) |
0.64 (0.42, 0.98) |
|
3-4 |
0.84 (0.52, 1.35) |
1.44 (0.81, 2.58) |
1.19 (0.84,1.68) |
|
5+(RC) |
1.00 |
1.00 |
1.00 |
|
Place of residence |
|||
|
Urban |
1.63 (1.15, 2.29) ** |
1.03 (0.70,1.52) |
0.94 (0.75,1.18) |
|
Rural (RC) |
1.00 |
1.00 |
1.00 |
|
Marital status |
|||
|
Never married |
0.82 (0.24, 2.82) |
1.05 (0.16, 6.90) |
0.54 (0.27, 1.10) |
|
Currently married |
1.83 (0.83,4.01) |
4.31 (0.90,20.65) |
0.80 (0.48, 1.34) |
|
Formerly married (RC) |
1.00 |
1.00 |
1.00 |
|
Religion |
|||
|
Catholic |
1.08 (0.44, 2.61) |
1.26 (0.47,3.33) |
1.25 (0.62, 2.52) |
|
Protestant |
0.88 (0.37, 2.14) |
0.89 (0.33, 2.40) |
1.12 (0.56,2.24) |
|
Charismatic |
1.24 (0.55, 2.78) |
0.90 (0.36,2.23) |
1.18 (0.62,2.23) |
|
Moslem |
1.07 (0.46, 2.50) |
0.83 (0.30, 2.26) |
1.00 (0.52,1.96) |
|
Traditional |
0.18 (0.02,1.82) |
1.06 (0.31, 3.62) |
0.69 (0.26, 1.85) |
|
No religion (RC) |
1.00 |
1.00 |
1.00 |
|
Fertility intention |
|||
|
Have Another |
0.98 (0.66, 1.45) |
0.66 (0.42,1.03) |
1.09 (0.82,1.45) |
|
Undecided |
1.39 (0.53, 3.64) |
0.16 (0.03, 0.74) * |
0.58 (0.38, 0.91) * |
|
No more (RC) |
1.00 |
1.00 |
1.00 |
|
Exposure to FP in the media |
|||
|
No (RC) |
1.00 |
1.00 |
1.00 |
|
Yes |
1.10 (0.76, 1.55) |
1.20 (0.83,1.75) |
0.80 (0.63, 1.00) |
Table 5: Results of binary logistic regression showing the factors that affecting changes in modern contraceptive use among postpartum women in Ghana in the context of antenatal health care visit, 2003, 2008 & 2014.
Note: ***= P value < 0.001; **= pvalue<0.01; * p value<0.05
(RC)=Reference Category; C.I=Confidence Interval
Source: computed by author using the GDHS 2003, 2008 & 2014
Again, results in table 5 suggests that in 2003 only two (partner’s educational level and place of residence) out of the ten variables included in the model were statistically significant factors affecting modern contraceptive use among postpartum women at the 0.05 significant level. This suggests that the demographic, social and economic characteristics are also important in affecting modern contraceptive use, thereby neutralizing the effect of antenatal health care services on modern contraceptive use. Furthermore, results in 2003 indicate that postpartum women whose partners had no formal education were 46 per cent less likely to use modern contraceptives compared to postpartum women whose partners had secondary or tertiary education. Again, women who resided in urban areas had higher odds (1.63) of using modern contraceptives compared to those in the rural areas.
In summary, the results in 2003 indicate that partner’s educational level and place of residence) were statistically significant in predicting modern contraceptive use among postpartum women at the 0.05 significance level. Again, after the inclusion of the control variables in the model, antenatal health care was no longer significant in predicting modern contraceptive use among postpartum women. Results in 2008 suggest that out of the thirteen variables included in the model, only three (maternal education, partners’ education and fertility intention) were significant in predicting modern contraceptive use. Again, the results indicate that women and their partners with no formal education were 44 per cent and 45 per cent less likely to use modern contraceptives compared to women whose partners had secondary or higher education. This outcome is expected because women and their men with higher educational level would have better understanding of contraceptives and be more receptive towards the use of modern contraceptives. Further, fertility intention of postpartum women was significant in predicting modern contraceptive use among them in Ghana. In 2008, the results show that postpartum women who were undecided on their fertility had a lower probability of using modern contraceptives compared to women who did not want to have any children. That is, postpartum women who are undecided on their fertility intention were 84 per cent less likely to use modern contraceptives relative to those whose fertility intention is to have no more children. The finding of this study is consistent with the findings of other studies which have shown fertility intention as an important predictor of modern contraceptive use [37-41]. These studies reported that women who desire more children do not intend to use a modern contraceptive method. The general observation of the results in 2014 suggest that out of the thirteen variables included in the model, five (antenatal health care, maternal age, maternal education, partners’ education and fertility intention) were significant in predicting modern contraceptive use. Furthermore, the results showed that compared to postpartum women who reported no antenatal visit, the probability of using modern contraceptives is higher among postpartum women who visited antenatal clinics 1-3 times and four or more times.
Also, the results indicate a significantly inverse relationship between current age of postpartum women and modern contraceptive use. Thus, as the age of a woman increases the prevalence rate of contraception also decreases. For instance, the odds ratios show that compared to postpartum women within 15-29 years, the likelihood of not using modern contraception is 44 per cent lower among women within the age groups 30-39 years. This statistically significant relationship is consistent with the findings of other studies on age and modern contraceptive use among women [37,42-44]. According to these studies, modern contraception is mostly prevalent among postpartum women within their 20s and 30s; and that the prevalence decreases drastically beyond 40 years. The reasons for this phenomenon are well documented in literature. Thus, age is used to make the claim that younger women are more dynamic and may be more willing to use modern contraceptives compared to older women. Also, most of these women had reached the older menopause, stopped bearing children and will have little or no need for modern contraceptives. Again, older women (40 years and over) may perceive to have a lower risk of pregnancy due to less frequent sexual activity or lower fecundity. Other studies, however, found no significant relationship between maternal age and modern contraception among women [45,46]. Educational level of women was also significant (P<0.05) in predicting modern contraceptive use among postpartum women in Ghana only in 2014. From the results, postpartum women with no formal education were 31 per cent less likely to use modern contraceptive compared to postpartum women who had attained secondary or higher education. Similar observation was made among women who partners had no formal education who had the lower likelihood of modern contraceptive use relative to partners with secondary or higher education. This result reiterates the important role formal education plays in modern contraceptive use.
Within the Ghanaian context, the results show that the relationship between number of antenatal visits and modern contraceptive use is highly influenced by women’s demographic and socio-economic characteristics. In the three survey years, factors such as place of residence, fertility intention, marital status, current age of women and their level of education of their partners were strong predicted of modern contraceptive use [47-50].
CONCLUSION AND RECOMMENDATIONS
In conclusion, Ghana as well as most sub-Saharan African countries has the potential of achieving high modern contraceptive prevalence if policies are put in place to ensure that quality and efficient contraceptive education is offered to people especially women in their postpartum period who are exposed to the risk of unintended pregnancy. Laying more emphasis on the important role antenatal health care service utilisation play in the contraceptive behaviour of women and to a large extent their sexual and reproductive health is of relevance. In other words, the utilisation of antenatal health care services could influence contraceptive use among postpartum women. However, demographic, social and economic factors have influence to a large extent the changes in contraceptive use among women in Ghana and must also be taken into a consideration. This also has relevance and implications to the realisation of the United Nations Sustainable Development Goal 3. This goal has a target of ensuring that by 2030 there will be universal access to sexual and reproductive health care services. These services include family planning information, education as well as the integration of reproductive health into national strategies and programmes.
CONTRIBUTORSHIP
DK conceptualised and design the study. DK analysed and interpreted the data. DK also drafted the entire manuscript. DK reviewed and revised the manuscript.
FUNDING
The authors have not declared a specific grant for this research form any funding agency in the public, commercial or not-for-profit sectors.
PATIENT AND PUBLIC INVOLVEMENT
No patient involved in the design, or conduct, or reporting of this research
ETHICS APPROVAL
The ICF Institutional Review Board (IRB) approved the protocol for the 2003, 2008 and 2014 GDHSs. However, ethnical approval was not needed for this study since it involved secondary data analysis devoid of personal identifies to women and their households. Nonetheless, the researcher obtained permission from ICF for the use of the datasets and the terms of use have been strictly adhered to.
DATA AVAILABILITY/SHARING STATEMENT
All data relevant to the study uploaded as supplementary information. Data is however openly available and can be accessed via https://dhsprogram.com/
REFERENCES
- World Health Organization (2013) WHO recommendations on postnatal care of the mother and newborn. WHO, Geneva, Switzerland.
- World Health Organization (2015) World health statistics 2015. WHO, Geneva, Switzerland.
- AbouZahr C, Wardlaw T (2003) Antenatal care in developing countries: Promises, achievements and missed opportunities - an analysis of trends, levels and differentials, 1990-2001. WHO, Geneva, Switzerland.
- Rutstein SO (2005) Effects of preceding birth intervals on neonatal, infant and under-five years mortality and nutritional status in developing countries: Evidence from the demographic and health surveys. Int J Gynaecol Obstet 89: 7-24.
- Hale L, DaVanzo J, Razzaque A, Rahman M (2009) Which factors explain the decline in infant and child mortality in Matlab, Bangladesh? Journal of population research 26: 3-20.
- Akinlo A, Bisiriyu A, Esimai O (2014) Use of maternal health care as a predictor of postpartum contraception in Nigeria. African Population Studies 27: 288-300.
- Mengesha ZB, Worku AG, Feleke SA (2015) Contraceptive adoption in the extended postpartum period is low in Northwest Ethiopia. BMC pregnancy and childbirth 15: 160.
- World Health Organization, United Nations Population Fund (2009) Mental health aspects of women's reproductive health: A global review of the literature. WHO, Geneva, Switzerland.
- Simmons R, Koenig MA, Huque AA (1990) Maternal-child health and family planning: User perspectives and service constraints in rural Bangladesh. Stud Fam Plann 21: 187-196.
- Hotchkiss DR, Magnani RJ, Rous JJ, Azelmat M, Mroz TA, et al. (1999) The effects of maternal-child health service utilization on subsequent contraceptive use in Morocco. J Biosoc Sci 31: 145-165.
- Lewin S, Munabi?Babigumira S, Glenton C, Daniels K, Bosch?Capblanch X, et al. (2010) Lay health workers in primary and community health care for maternal and child health and the management of infectious diseases. Cochrane Database Syst Rev 2010: CD004015.
- Ahmed S, Mosley WH (2002) Simultaneity in the use of maternal-child health care and contraceptives: Evidence from developing countries. Demography 39: 75-93.
- Borda MR, Winfrey W, McKaig C (2010) Return to sexual activity and modern family planning use in the extended postpartum period: An analysis of findings from seventeen countries. Afr J Reprod Health 14: 72-79.
- Ekabua JE, Ekabua KJ, Odusolu P, Iklaki CU, Agan TU, et al. (2010) Factors associated with contraceptive use and initiation of coital activity after childbirth. Open access journal of contraception 1: 85-91.
- Do M, Hotchkiss D (2013) Relationships between antenatal and postnatal care and post-partum modern contraceptive use: Evidence from population surveys in Kenya and Zambia. BMC Health Serv Res 13: 6.
- Speizer IS, Fotso JC, Okigbo C, Faye CM, Seck C (2013) Influence of integrated services on postpartum family planning use: A cross-sectional survey from urban Senegal. BMC Public Health 13: 752.
- Lauria L, Donati S, Spinelli A, Bonciani M, Grandolfo ME (2014) The effect of contraceptive counselling in the pre and post-natal period on contraceptive use at three months after delivery among Italian and immigrant women. Ann Ist Super Sanita 50: 54-61.
- Achyut P, Mishra A, Montana L, Sengupta R, Calhoun LM, et al. (2016) Integration of family planning with maternal health services: An opportunity to increase postpartum modern contraceptive use in urban Uttar Pradesh, India. J Fam Plann Reprod Health Care 42: 107-115.
- David M, Brenne S, Breckenkamp J, Razum O, Borde T (2015) Postpartum Contraception: A Comparative Study of Berlin Women with and without Immigration Background. Geburtshilfe Frauenheilkd 75: 915-922.
- GSS, GHS, ICF Macro (2009) Ghana Demographic and Health Survey 2008. GSS, GHS and ICF Macro, Accra, Ghana.
- Obaid TA (2009) Fifteen years after the International Conference on Population and Development: What have we achieved and how do we move forward? Int J Gynaecol Obstet 106: 102-105.
- Ross JA, Winfrey WL (2001) Contraceptive Use, Intention to Use and Unmet Need During the Extended Postpartum Period. International family planning perspectives 27: 20-27.
- Widyastuti L, Saikia US (2014) Postpartum contraceptive use in Indonesia: recent patterns and determinants. Institute for Population and Social Research (IPSR), Bangkok, Thailand.
- Asundep NN, Jolly PE, Carson A, Turpin CA, Zhang K, et al. (2014) Antenatal care attendance, a surrogate for pregnancy outcome? The case of Kumasi, Ghana. Matern Child Health J 18: 1085-1094.
- Nketiah?Amponsah E, Senadza B, Arthur E (2013) Determinants of Utilization of Antenatal care Services in Developing Countries: Recent Evidence from Ghana. African Journal of Economic and Management Studies 4: 58-73.
- Pell C, Meñaca A, Were F, Afrah NA, Chatio S, et al. (2013) Factors affecting antenatal care attendance: Results from qualitative studies in Ghana, Kenya and Malawi. PLoS One 8: 53747.
- Dahiru T, Oche OM (2015) Determinants of antenatal care, institutional delivery and postnatal care services utilization in Nigeria. Pan Afr Med J 21: 321.
- Yadav D, Dhillon P (2015) Assessing the impact of family planning advice on unmet need and contraceptive use among currently married women in Uttar Pradesh, India. PloS one 10: 0118584.
- Kavanaugh ML, Anderson RM (2020) Contraception and Beyond: The Health Benefits of Services Provided at Family Planning Centers. Guttmacher Institute, New York, USA.
- Lindegren ML, Kennedy CE, Bain?Brickley D, Azman H, Creanga AA, et al. (2012) Integration of HIV/AIDS services with maternal, neonatal and child health, nutrition, and family planning services. Cochrane Database Syst Rev 12: CD010119.
- Cohen B (1993) Fertility levels, differentials, and trends. Demographic change in sub-Saharan Africa 15: 8-67.
- Singh S, Sedgh G, Hussain R (2010) Unintended pregnancy: worldwide levels, trends, and outcomes. Stud Fam Plann 41: 241-250.
- Bankole A, Rodriguez G, Westoff CF (1996) Mass media messages and reproductive behaviour in Nigeria. J Biosoc Sci 28: 227-239.
- Parr N (2001) Mass media promotion of family planning and the use of modern contraception in Ghana. International Union for the Scientific Study of Population (IUSSP), Salvador, Brazil.
- Tisha S, Haque SMR, Tabassum M (2015) Antenatal Care, an Expediter for Postpartum Modern Contraceptive Use. Res Obstet Gynecol 3: 22-31.
- Day T, Raker CA, Boardman LA (2008) Factors associated with the provision of antenatal contraceptive counseling. Contraception 78: 294-299.
- Campbell EK, Campbell PG (1997) Family size and sex preferences and eventual fertility in Botswana. J Biosoc Sci 29: 191-204.
- Bankole A, Singh S (1998) Couples' Fertility and Contraceptive Decision-Making In Developing Countries: Hearing the Man's Voice. International family planning perspectives 24: 15-24.
- Islam MM, Bairagi R (2003) Fertility intentions and subsequent fertility behaviour in Matlab: Do fertility intentions matter? J Biosoc Sci 35: 615-619.
- Roy DK, O'Neill TW, Finn JD, Lunt M, Silman AJ, et al. (2003) Determinants of incident vertebral fracture in men and women: Results from the European Prospective Osteoporosis Study (EPOS). Osteoporos Int 14: 19-26.
- Agadjanian V (2006) Fraught with Ambivalence: Reproductive Intentions and Contraceptive Choices in a Sub-Saharan Fertility Transition. Population Research and Policy Review 24: 617-645.
- Gupta N, Katende C, Bessinger R (2003) Associations of mass media exposure with family planning attitudes and practices in Uganda. Stud Fam Plann 34: 19-31.
- Mawajdeh S (2007) Demographic profile and predictors of unmet need for family planning among Jordanian women. J Fam Plann Reprod Health Care 33: 53-56.
- Bbaale E, Mpuga P (2011) Female Education, Contraceptive Use, and Fertility: Evidence from Uganda. Consilience 6: 20-47.
- Agampodi SB, Agampodi TC, Chandrasekara P (2009) Family Planning Prevalence Among Postpartum Mothers Attending Child Welfare Clinics - A Sri Lankan Experience. Indian J Community Med 34: 265-266.
- Mahmood SE, Srivastava A, Shrotriya VP, Mishra P (2012) Infant feeding practices in the rural population of north India. J Family Community Med 19: 130-135.
- Smith KB, Van Der Spuy ZM, Cheng L, Elton R, Glasier AF (2002) Is postpartum contraceptive advice given antenatally of value? Contraception 65: 237-243.
- Smith R, Ashford L, Gribble J, Clifton D (2009) Family planning saves lives. Population Reference Bureau, Washington DC, USA.
- Hertrich V (2017) Trends in Age at Marriage and the Onset of Fertility Transition in sub?Saharan Africa. Population and Development Review 43: 112-137.
- Anasel MG, Mlinga UJ (2014) Determinants of contraceptive use among married women in Tanzania: Policy implication. African Population Studies 28: 976-988.
Citation: Klu D (2020) Influence of Antenatal Health Care Visit on modern Contraceptive Use among Postpartum Women in Ghana. J Reprod Med Gynecol Obstet 5: 054.
Copyright: © 2020 Desmond Klu, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

