
Influence of Music/Exercise Therapy at Home on Levels of Adiponectin and Homocysteine in Caregivers of Patients with Dementia in Japan: A Randomized Controlled Study
*Corresponding Author(s):
Akemi HiranoDepartment Of Adult Nursing, Shubun University, Faculty Of Nursing, 6 Nikko-cho, Ichinomiya, Aichi, 491-0938, Japan
Tel:+81 586452101,
Fax:+81 586454410
Email:hirano@med.nagoya-u.ac.jp
Abstract
Objectives: While many factors could contribute to the high incidence of vascular events in caregivers of patients with dementia, one mechanism may involve their high blood coagulability, which reportedly is higher than that of non-dementia caregivers. One factor that may account for this phenomenon is the psychological stress associated with caregiving. This study aimed to determine whether an in-home activity program that incorporates music/exercise therapy for dementia caregivers can reduce stress associated with caregiving, and thereby improve levels of atherosclerosis-promoting factors such as adiponectin, homocysteine, and high sensitivity C-Reactive Protein (hs-CRP).
Methods: Participants were older caregivers of patients with Alzheimer-type dementia, who were randomly assigned to either an intervention or control group. The intervention group took part in an activity program that incorporated music/exercise therapy (20 minutes/twice a week for 12 weeks), while the control group carried on with routine daily care.
Results: Forty-two caregivers participated, and levels of adiponectin and homocysteine improved in both groups. Geriatric Depression Scale (GDS) score improved significantly in the intervention group, but did not change in the control group. While the Zarit Burden Interview score did not significantly change in the intervention group, it significantly worsened in the control group.
Conclusion: Music/exercise therapy had a positive effect on the intervention group. Given reports that decreased levels of adiponectin are related to the severity of depression, changes in levels of adiponectin despite the lack of increase in total physical activity in the control group may have involved a psychological factor.
Keywords
Adiponectin; Caregiver burden; Dementia, Homocysteine; Intervention
INTRODUCTION
Caregivers of patients with dementia are considered to experience a large psychological burden due to various behavioral and psychological symptoms their care recipients present compared with caregivers of patients with other medical conditions [1,2]. Dementia caregivers often suffer from hypertension [3], ischemic heart disease [4], reduced immune function [5] and have a high mortality rate [6]. While many factors are considered to be involved in the higher incidence of medical events in dementia caregivers, their higher blood coagulability may be an important aspect [7]. One factor that could contribute to this is the psychological stress associated with caregiving. We previously reported that the severity of sense of burden in older dementia caregivers is related to lower physical activity, particularly a reduced amount of leisure activity [8].
Many intervention studies aimed at reducing the sense of burden in caregivers have taken counseling and education-based approaches. One study demonstrated that satisfaction with leisure improved after caregivers of patients with dementia were educated on communication skills [9]. The need for education/activity programs, respite programs, information resources, support, and education programs that advocate for caregivers, as well as the need for leisure activity, have also been suggested [10]. Another study involving leisure activity that targeted dementia caregivers found that participation in various types of leisure activities away from home (e.g., dancing, eating at restaurants, and going to concerts) by caregivers and care recipients improved both physical symptoms and depression in the caregivers [11]. Likewise, another study found improvements in the relationship between caregivers and care recipients after participating together in a program that included leisure activities [12].
Rapid aging of the society in Japan is inevitably increasing the social burden related to the care of older people [13]. The time spent by older caregivers to care for their dementia care recipients generally restricts opportunities for recreational activities, which may affect their physical/mental health. Against this backdrop, we focused on the potential benefits of music/exercise therapy. Such therapy is reportedly not only effective against various clinical symptoms, but can also reduce psychological burden resulting in depression [14] and increase the motor balance function of older people [15]. However, no study to date has investigated the efficacy of music/exercise therapy in reducing caregiver burden by jointly involving dementia patients and their older caregivers.
We previously reported that periodic aerobic exercises effectively reduced the sense of burden in older dementia caregivers who suffer from chronic diseases such as hypertension and dyslipidemia [16]. Yet, these caregivers often had physical or movement disorders that restricted movement. Moreover, some reports have suggested that these caregivers find it difficult to secure the time needed to travel to facilities that offer activity programs, and thus cannot increase their participation in activities, as doing so would require them to leave dementia patients at home alone [17]. To this end, the present study aimed to assess whether the joint participation of dementia patients and their older caregivers in music/exercise therapy at home can help maintain caregiver health and reduce their sense of burden.
METHODS
Participants
Participants were 42 elderly caregivers aged ≥65 years who lived together with Alzheimer-type dementia patients diagnosed according to DSM-IV criteria by geriatricians. Eligible caregivers were those who did not routinely exercise to music (i.e., more than once a week). While we targeted healthy caregivers, those with chronic diseases (e.g., hypertension, diabetes and dyslipidemia) that were well-controlled through periodic treatment at a medical facility were also included. We excluded those with a history of cerebrovascular or heart diseases, such as cerebral infarction and myocardial infarction, or liver diseases.
Study design
Caregiver/dementia patient pairs were randomly assigned to the intervention or control group. Basis design was parallel, Rundomization unit was Individual, Open-no one is blinded. The intervention group engaged in an activity program that incorporated music/exercise therapy, whereas the control group continued with their regular daily routine. We assessed whether our program affected care burden by comparing various parameters before and 12 weeks after the intervention.
Assessed factors and scales for caregivers
The primary outcome measure was the score of the Japanese version of the Zarit Burden Interview (ZBI) [18]. The Japanese version of the ZBI is a 22-item questionnaire that scores care burden as the sum of physical burden, psychological burden, and economic difficulty that caregivers experience as they provide care at home to those with care needs. The secondary outcome measure was levels of atherosclerosis-promoting factors, including adiponectin, homocysteine and hs-CRP. The levels of these factors were assessed after blood was sampled. Blood sample measurements were outsourced to a blood test company which provided us with the measurement data. The short version of the Geriatric Depression Scale (GDS), widely used for evaluating depressive mood in older people with physical complications [19], was used in this study. The amount of total physical activity of caregivers was calculated by the sum of the housework score, sports score, and leisure score, with higher total scores indicating greater amounts of physical activity [20]. Leisure activities (drawing (sketching), watercolor painting and calligraphy) were defined as physical activities other than housework and sports activities (walking, swimming and physical exercise). Adverse events were not reported.
Intervention program
The activity program which incorporated music/exercise therapy comprised activities falling under the scope of sports score and leisure score, both of which are subscales of total physical activity. In addition to daily care routines, the intervention group engaged in the activity program (twice a week, 20 minutes/session), whereas the control group carried out only daily care routines. The intervention group performed exercises from among those we provided as options at baseline. These activities were those which could be carried out on a continuous basis by caregivers along with popular memorable songs, children’s songs, or folk songs. In principle, the amount of physical activity was set to 1.5-2.0 METs, and if similar in degree, activities other than those we originally presented as options were allowed. Activities excluded from the program included those with an extremely low amount of physical activity that did not require constant movement of the hands/fingers (e.g., listening to music).
Scale for dementia patients
As a simple measure to evaluate the mental function of dementia patients, we used the Japanese version of the Mini-Mental State Examination (MMSE) [21].
Statistical analysis
Statistical analyses were conducted with SPSS software (version 25.0). The Mann-Whitney U test was used to compare baseline background characteristics between the two groups. The Wilcoxon signed-rank test was used in baseline and post-intervention comparisons of the two groups. P<0.05 was considered statistically significant.
Ethical considerations
This study was approved by the Nagoya University Graduate School of Medicine Ethics Committee. Written consent was obtained from all participants. Appropriate ethical measures were taken, such as making it clear that participation in the study was strictly voluntary. Data were collected Nagoya University Hospital in Japan.
RESULTS
In total, 110 caregiver/dementia patient pairs were selected by geriatricians as potential candidates for inclusion in the study. Of these, 65 pairs (59%) declined to participate or were excluded, including 44 pairs in which the caregiver refused, and 21 pairs for various reasons (e.g., no time, busy with caregiving, live too far away, do not want to participate, did not meet inclusion criteria, exercise habits (e.g., dancing) two or more times a week, back pain, dizziness). Of the remaining 45 pairs, 3 were discontinued (busy with caregiving, 2; feeling unwell, 1), while the rest were randomized into either the intervention group (22 pairs) or the control group (20 pairs) (Figure 1). Baseline characteristics were similar between the intervention and control groups (Table 1). Table 2 shows differences before and after the intervention. In both the intervention and control groups, levels of adiponectin and homocysteine significantly improved (p<0.05). However, hs-CRP and BMI did not significantly change. While the ZBI score did not significantly change in the intervention group, it significantly worsened in the control group (p<0.05). The GDS score significantly decreased in the intervention group (p<0.05), but did not change in the control group. Housework and sports scores significantly increased in the intervention group. Regarding cognition, MMSE scores of dementia patients showed no significant changes in either the intervention or control groups.
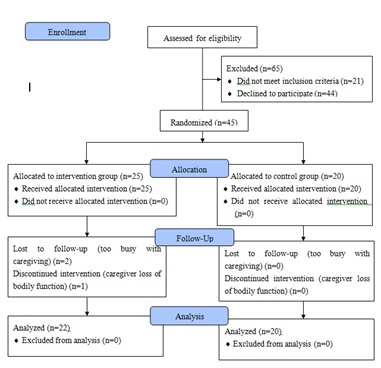 Figure 1: Study flow chart.
Figure 1: Study flow chart.
|
Intervention (n=22) |
Control (n=20) |
||||
|
Variable |
Median |
IQR |
Median |
IQR |
P value |
|
Caregivers |
|||||
|
Age, y |
80 |
73.5-81.5 |
79.0 |
75.5-82.0 |
0.880 |
|
Sex (M/F), n/% |
7/15 |
31.8/68.2 |
May-15 |
25/75 |
0.629 |
|
Adiponectin μg/mL (≥4.0) |
12.75 |
8.28-17.90 |
9.55 |
7.30-24.90 |
0.791 |
|
hs-CRP mg/dL (no ref value) |
0.039 |
0.022-0.108 |
0.047 |
0.021-0.123 |
0.930 |
|
Homocysteine nmol/mL (3.7-13.5) |
12.5 |
11.28-16.33 |
11.95 |
10.80-16.25 |
0.659 |
|
BMI |
22.31 |
19.6-25.0 |
20.8 |
19.3-23.7 |
0.290 |
|
ZBI sense of burden-total |
18.5 |
11-33 |
25.0 |
17.3-40.8 |
0.203 |
|
GDS |
4.5 |
2-7 |
7.0 |
4.0-10.5 |
0.051 |
|
Total physical activity (HS+SS+LS) |
2.13 |
1.75-2.66 |
1.92 |
2.22-2.56 |
0.641 |
|
Housework score (HS) |
2.00 |
1.67-2.14 |
1.67 |
2.06-2.33 |
0.510 |
|
Sports score (SS) |
0.00 |
0.00-0.41 |
0.00 |
0.00-0.41 |
0.740 |
|
Leisure score (LS) |
0.00 |
0.00-0.00 |
0.00 |
0.00-0.05 |
0.461 |
|
Dementia Patients |
|||||
|
Age, y |
80.0 |
77.0-83.5 |
82.0 |
78.0-85.0 |
0.677 |
|
MMSE |
21 |
16-25.3 |
18.0 |
14.3-22.8 |
0.124 |
Table 1: Baseline characteristics.
∗p < 0.05; ∗∗p < 0.01 by the Mann-Whitney U test.
Data are presented as median; IQR, Interquartile Range; hs-CRP, High Sensitivity C-Reactive Protein; BMI, Body Mass Index; ZBI, Zarit Burden Interview; GDS, Geriatric Depression Scale; MMSE, Mini-Mental State Examination
|
|
Intervention (n=22) |
Control (n=20) |
||
|
Variable |
Median (?) |
P value |
Median (?) |
P value |
|
Caregivers |
||||
|
Adiponectin µg/mL (≥4.0) |
0.200** |
0.000 |
1.250** |
0.001 |
|
hs-CRP mg/dL (no ref value) |
0.008 |
0.661 |
-0.005 |
0.575 |
|
Homocysteine nmol/mL (3.7-13.5) |
- 1.550** |
0.000 |
-2.150** |
0.008 |
|
ZBI |
0.5 |
0.736 |
4.5* |
0.031 |
|
Total physical activity (HS+SS+LS) |
0.235** |
0.003 |
-0.005 |
0.296 |
|
Housework score (HS) |
0.110 * |
0.019 |
-0.111 |
0.322 |
|
Sports score (SS) |
0.038** |
0.000 |
0.000 |
0.889 |
|
Leisure score (LS) |
0.000 |
0.285 |
0.000 |
0.273 |
|
GDS |
-1.5* |
0.03 |
-1.0 |
0.759 |
|
BMI |
0.5 |
0.263 |
0.005 |
0.760 |
|
Dementia Patients |
||||
|
MMSE |
-1.0 |
0.777 |
2.0 |
0.977 |
Table 2: Changes in outcomes after intervention.
Change after intervention (?) = post-intervention value - baseline value
*p<0.05; **p
DISCUSSION
In the present study, we succeeded in increasing the amount of total physical activity performed at home by caregivers who live with dementia patients, but did not observe an effect of intervention on the profiles of atherosclerosis-promoting factors since both groups showed some improvements in these factors. Given previous reports showing that reduced levels of adiponectin and severity of depression are related, changes observed in the control group despite the lack of increased physical activity may suggest a psychological basis. Rhythmically repeating muscle flexion and relaxation during music/exercise therapy is likely to prevent the formation of vascular lesions that result from the progression of atherosclerosis through an increase in cardiovascular function by acting on the circulatory system, and thus improving cardiac and vascular systems.
In the present study, adiponectin and homocysteine levels, but not hs-CRP levels, significantly improved in both intervention and control groups. Adiponectin functions directly on the vascular wall and has an anti-arteriosclerotic effect [22]. A low level of adiponectin is considered a risk factor for atherosclerosis [23,24] and adiponectin levels improve with exercise [25,26]. This suggests that improved levels in the intervention group can potentially be explained by increased physical activity. The mechanism underlying the increased secretion of adiponectin may involve its activation in liver/muscle following exercise, which leads to the stimulation of adipocytes and subsequent improvement in circulation.
On the other hand, in high-risk coronary artery disease patients, plasma adiponectin levels above 6.38 µg/ml are reportedly associated with a paradoxical higher risk of cardiovascular death. Indeed, patients with high-plasma adiponectin levels have a higher cardiovascular death rate than low-plasma adiponectin patients [27]. In the present study, the cardiovascular status of our participants was satisfactory, with baseline adiponectin levels ≥4.0 (reference value) in both control and intervention groups. After the intervention, the change in adiponectin levels in the intervention group was 1.57%, and since the median baseline adiponectin level in the intervention group was satisfactory at 12.75, it may have been difficult to further improve adiponectin levels. In the control group, however, the change in adiponectin levels was 13.09% and the median baseline adiponectin level was 9.55. While this value is within the reference range, it was low compared to that of the intervention group. Thus, although no intervention was performed, it is possible that the psychological impact from participating in the study itself improved adiponectin levels in the control group.
According to one study, increased physical activity slightly reduced homocysteine levels in young people [28]. However, in the control group, which engaged only in routine caregiving, both adiponectin and homocysteine levels improved despite the lack of increase in total physical activity. We speculate that improvements in adiponectin and homocysteine levels in the control group had a psychological underpinning, in which participation in the study gave caregivers a sense that people were interested in them. Reduction in adiponectin levels is reportedly associated with the severity of depression, with higher severity being associated with lower adiponectin levels [29]. One study found that adiponectin levels recovered following treatment for depression [30]. Moreover, acute psychological stress can significantly and rapidly induce total plasma homocysteine levels in adult women [31]. High levels of homocysteine are correlated with depressive symptoms in community-dwelling middle-aged people [32] and animal models suggest that depression is associated with high homocysteine levels [33]. In the present study, compared to the intervention group, caregivers in the control group had a higher GDS score.
While blood hs-CRP is an important marker for predicting cardiovascular events, hs-CRP and BMI did not significantly change in either the control or intervention group in this study. Physical rehabilitation has been reported to significantly reduce waist circumference and fat weight, leading to a significant reduction in hs-CRP levels [34]. However, neither BMI nor hs-CRP significantly changed in either group of this study. Since physical activity was set at a level that was relatively easy for older caregivers to continue, BMI (reflecting visceral fat) and cytokines (involving hs-CRP) secreted from visceral fat may not have changed.
While the ZBI score did not change in the intervention group, it significantly worsened in the control group. In a study that found that leisure activity can improve ZBI scores, the type of leisure activity was chosen by caregivers themselves and thus was easy to continue [35]. Caregivers in the intervention group of the present study did not experience substantial changes in their subjective sense of burden, suggesting that incorporating music/exercise therapy into their daily lives may have had a pleasant stimulating effect or may have allowed them to free themselves temporarily from caregiving and switch gears, thereby suppressing the sense of burden. This suggests that the increase in sense of burden during the natural progression of the few months of observation was prevented, and that the intervention group had a low depressive tendency at baseline and likely was more resilient to sense of burden than the control group. However, since the contents of the present program were preset, caregivers’ taste may have had an impact; given the relatively low level of activity and short intervention period and duration of activities, this result could be attributed to the limited amount of physical activity. In the control group, we speculate that the lack of activity (in the form of music/exercise therapy) led to a greater sense of caregiver burden.
MMSE scores of dementia patients did not significantly change in either group over the observation period. Music therapy has been shown to effectively improve the QOL of caregivers, reduce depression, and maintain the cognitive function of dementia patients [36]. However, given that MMSE scores did not improve in the intervention group, the study duration may have been too short to observe changes in MMSE scores. This study has some limitations worth noting. First, the study was conducted at a single facility, and thus the ability to generalize the conclusions is limited. Second, given the small sample size, the statistical power may not have been sufficient to detect differences. Our findings also suggest the need to develop a program that can be performed on a continuous basis even for busy caregivers. Finally, given the possibility that the severity of neuropsychiatric symptoms of dementia patients may have a greater impact on caregiver burden than MMSE scores, the psychiatric symptoms of dementia patients will need to be considered in future studies.
In conclusion, a program should be developed that maintains the amount of physical activity in caregivers, suppresses the progression or onset of atherosclerosis through exercise, and maintains the health of caregivers and reduces their sense of burden. If the program also has a beneficial effect on the cognitive function of dementia patients, this would also help to reduce the burden of caregivers and have important social and medical implications.
AUTHOR ROLES
Akemi Hirano and Hiroyuki Umegaki conceived the idea and designed this study. Akemi Hirano carried out data analysis and interpretation. Akemi Hirano wrote the first draft and Yusuke Suzuki, Hiroyuki Umegaki and Koichiro Ina critically discussed all versions of the manuscript. Yusuke Suzuki, Hiroyuki Umegaki, Koichiro Ina, Toshio Hayashi, and Takahisa Hirose recruited the participants, and Hiroyuki Umegaki contributed to the overall supervision of the present study.
ACKNOWLEDGEMENT
We thank those involved in this study, including patients and their families, for their assistance and participation. This study was supported by a Grant-in-Aid for Scientific Research (Scientific Research Grant).
REFERENCES
- Onishi J, Suzuki Y, Umegaki H, Nakamura A, Endo H, et al. (2005) Influence of Behavioral and Psychological Symptoms of Dementia (BPSD) and Environment of Care on Caregivers' Burden. Arch Gerontol Geriatr 41: 159-168.
- Muraki I, Yamagishi K, Ito Y, Fujieda T, Ishikawa Y, et al. (2008) Caregiver Burden for Impaired Elderly Japanese With Prevalent Stroke and Dementia Under Long-Term Care Insurance System. Cerebrovasc Dis 25: 234-240.
- Shaw WS, Patterson TL, Ziegler MG, Dimsdale JE, Semple SJ, et al. (1999) Accelerated risk of hypertensive blood pressure recordings among alzheimer caregivers. Journal of psychosomatic research 46: 215-227.
- Mausbach BT, Patterson TL, Rabinowitz YG, Grant I, Schulz R (2007) Depression and Distress Predict Time to Cardiovascular Disease in Dementia Caregivers. Health Psychol 26: 539-544.
- Mills PJ, Adler KA, Dimsdale JE, Perez CJ, Ziegler MG, et al. (2004) Vulnerable Caregivers of Alzheimer Disease Patients Have a Deficit in Beta 2-adrenergic Receptor Sensitivity and Density. Am J Geriatr Psychiatry 12: 281-286.
- Schulz R, Beach SR (1999) Caregiving as a Risk Factor for Mortality: The Caregiver Health Effects Study. JAMA 282: 2215-2219.
- von Kanel R, Dimsdale JE, Adler KA, Patterson TL, Mills PJ, et al. (2005) Exaggerated plasma fibrin formation (D-Dimer) in elderly Alzheimer caregivers as compared to noncaregiving controls. Gerontology 51: 7-13.
- Hirano A, Suzuki Y, Kuzuya M, Onishi J, Hasegawa J, et al. (2011) Association Between the Caregiver's Burden and Physical Activity in Community-Dwelling Caregivers of Dementia Patients. Arch Gerontol Geriatr 52: 295-298.
- Burgio L, Stevens A, Guy D, Roth DL, Haley WE (2003) Impact of Two Psychosocial Interventions on White and African American Family Caregivers of Individuals With Dementia. Gerontologist 43: 568-579.
- Bedini LA, Phoenix TL (1999) Addressing leisure barriers for caregivers of older adults: a model leisure wellness program. Therapeutic Recreation Journal 33: 222-240.
- Wilz G, Fink-Heitz M (2008) Assisted Vacations for Men With Dementia and Their Caregiving Spouses: Evaluation of Health-Related Effects. Gerontologist 48: 115-120.
- Carbonneau H, Caron CD, Desrosiers J (2011) Effects of an Adapted Leisure Education Program as a Means of Support for Caregivers of People With Dementia. Arch Gerontol Geriatr 53: 31-39.
- Ministry of Health, Labour and Welfare (2016) Ministry of Health, Labour and Welfare. MHLW White Paper. Tokyo, Japan.
- Verrusio W, Andreozzi P, Marigliano B, Renzi A, Gianturco V, et al. (2014) Exercise Training and Music Therapy in Elderly With Depressive Syndrome: A Pilot Study. Complement Ther Med 22: 614-620.
- Feys P, Moumdjian L, Van Halewyck F, Wens I, Eijnde BO, Van Wijmeersch B, et al. (2019) Effects of an Individual 12-week Community-Located "Start-To-Run" Program on Physical Capacity, Walking, Fatigue, Cognitive Function, Brain Volumes, and Structures in Persons With Multiple Sclerosis. Mult Scler 25: 92-103.
- Hirano A, Suzuki Y, Kuzuya M, Onishi J, Ban N, et al. (2011) Influence of Regular Exercise on Subjective Sense of Burden and Physical Symptoms in Community-Dwelling Caregivers of Dementia Patients: A Randomized Controlled Trial. Arch Gerontol Geriatr 53: 158-163.
- Hill K, Smith R, Fearn M, Rydberg M, Oliphant R (2007) Physical and Psychological Outcomes of a Supported Physical Activity Program for Older Carers. J Aging Phys Act 15: 257-271.
- Zarit SH, Reever KE, Bach-Peterson J (1980) Relatives of the Impaired Elderly: Correlates of Feelings of Burden. Gerontologist 20: 649-655.
- Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, et al. (1982-1983) Development and Validation of a Geriatric Depression Screening Scale: A Preliminary Report. J Psychiatr Res 17: 37-49.
- Voorrips LE, Ravelli AC, Dongelmans PC, Deurenberg P, Van Staveren WA (1991) A Physical Activity Questionnaire for the Elderly. Med Sci Sports Exerc 23: 974-979.
- Folstein MF, Folstein SE, McHugh PR (1975) "Mini-mental State". A Practical Method for Grading the Cognitive State of Patients for the Clinician. J Psychiatr Res 12: 189-198.
- Goldstein BJ, Scalia R (2004) Adiponectin: A Novel Adipokine Linking Adipocytes and Vascular Function. J Clin Endocrinol Metab 89: 2563-2568.
- Zoccali C, Mallamaci F, Tripepi G, Benedetto FA, Cutrupi S, et al. (2002) Adiponectin, Metabolic Risk Factors, and Cardiovascular Events Among Patients With End-Stage Renal Disease. J Am Soc Nephrol 13: 134-141.
- Kumada M, Kihara S, Sumitsuji S, Kawamoto T, Matsumoto S, et al. (2003) Association of Hypoadiponectinemia With Coronary Artery Disease in Men. Arterioscler Thromb Vasc Biol 23: 85-89.
- Kondo T, Kobayashi I, Murakami M (2006) Effect of Exercise on Circulating Adipokine Levels in Obese Young Women. Endocr J 53: 189-195.
- Blüher M, Bullen JW Jr, Lee JH, Kralisch S, Fasshauer M, et al. (2006) Circulating Adiponectin and Expression of Adiponectin Receptors in Human Skeletal Muscle: Associations With Metabolic Parameters and Insulin Resistance and Regulation by Physical Training. J Clin Endocrinol Metab 91: 2310-2316.
- Maiolino G, Cesari M, Sticchi D, Zanchetta M, Pedon L, et al. (2008) Plasma Adiponectin for Prediction of Cardiovascular Events and Mortality in High-Risk Patients. J Clin Endocrinol Metab 93: 3333-3340.
- Benser J, Valtueña J, Ruiz JR, Mielgo-Ayuso J, Breidenassel C, et al. (2015) Impact of Physical Activity and Cardiovascular Fitness on Total Homocysteine Concentrations in European Adolescents: The HELENA Study. J Nutr Sci Vitaminol (Tokyo) 61: 45-54.
- Leo R, Di Lorenzo G, Tesauro M, Cola C, Fortuna E, et al. (2006) Decreased Plasma Adiponectin Concentration in Major Depression. Neurosci Lett 407: 211-213.
- Narita K, Murata T, Takahashi T, Kosaka H, Omata N, et al. (2006) Plasma Levels of Adiponectin and Tumor Necrosis Factor-Alpha in Patients With Remitted Major Depression Receiving Long-Term Maintenance Antidepressant Therapy. Prog Neuropsychopharmacol Biol Psychiatry 30: 1159-1162.
- Stoney CM (1999) Plasma Homocysteine Levels Increase in Women During Psychological Stress. Life Sci 64: 2359-2365.
- Sachdev PS, Parslow RA, Lux O, Salonikas C, Wen W, et al. (2005) Relationship of Homocysteine, Folic Acid and Vitamin B12 With Depression in a Middle-Aged Community Sample. Psychol Med 35: 529-538.
- Chengfeng S, Wei L, Xinxing W, Lei W, Rui Z, et al. (2014) Hyperhomocysteinemia Is a Result, Rather than a Cause, of Depression under Chronic Stress. PLoS one 9: 106625.
- Onishi T, Shimada K, Sunayama S, Ohmura H, Sumide T, et al. (2009) Effects of Cardiac Rehabilitation in Patients With Metabolic Syndrome After Coronary Artery Bypass Grafting. J Cardiol 53: 381-387.
- Hirano A, Umegaki H, Suzuki Y, Hayashi T, Kuzuya M (2016) Effects of Leisure Activities at Home on Perceived Care Burden and the Endocrine System of Caregivers of Dementia Patients: A Randomized Controlled Study. Int Psychogeriatr 28: 261-268.
- Kim HJ, Yang Y, Oh JG, Oh S, Choi H, et al. (2016) Effectiveness of a Community-Based Multidomain Cognitive Intervention Program in Patients With Alzheimer's Disease. Geriatr Gerontol Int 16: 191-199.
Citation: Hirano A, Suzuki Y, Hayashi T, Ina K, Hirose T, et al. (2020) Influence of Music/Exercise Therapy at Home on Levels of Adiponectin and Homocysteine in Caregivers of Patients with Dementia in Japan: A Randomized Controlled Study. J Gerontol Geriatr Med 6: 056.
Copyright: © 2020 Akemi Hirano, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

