
Influence of Tobacco and Pericoronitis in the Production of Post-Exodoncia Alveolitis of the Third Molar, Statistical Analysis in SPSS
*Corresponding Author(s):
Alfredo Reinoso SantiagoAndalusian Health Service, Aljarafe Sanitary District Sevilla-Norte, Seville, Spain
Email:alresa001@yahoo.es
Abstract
Descriptive observational study, development of statistical parameter dumps from Excel to SPSS program. Collection of consultation data High-Resolution of Primary Care Dentistry, Aljarafe Health District, Andalusian Health Service-Andalusia-Spain. Using dependent variables, the production of alveolitis after surgical exodomy of the third molar, independent variables the personal history of the patient, the previous pericoronitis, treated, the Koerner index and smoker/non-smoker, and as age and sex confusing variables.
In our study we observed the great influence of tobacco and previous infection, the treated pericoronitis. The difficulty of the intervention does not influence, taking the belief that, with greater difficulty index, the greater possibility of the existence of alveolitis, given in the study the incidence of alveolitis in low or average Koerner scale.
Preamble
How does a different factor influence the production of post molar alveolitis of the third molar?
In most studies, tobacco is related to the appearance of post-exodontic alveolitis, our study wants to assess the importance of tobacco and a previous infectious process, pericoronitis. Interpreting as hypothesis that previous infections are also, together with tobacco influencing the appearance of alveolitis.
INTRODUCTION
The exodontics of the third molar today is being performed on a daily basis, including prophylactics. And they are the most frequent included teeth [1], in relation to morphology, number of roots, as well as the relationship with neighboring structures are very variable, causing different pathologies [2], making it the most frequent surgical intervention in the stomatognathic apparatus [3].
The third molar presents its eruption at an average age of 19.5 to 20.5 years [4], it is therefore the last tooth in eruption, so it can easily be impacted or suffer displacements, if there is not enough space in the dental arch [2], they do not evolve towards a correct situation, being able to generate pathology.
Injury produced by third molars
It is the anatomical and embryological characteristics that determine the retention or degree of eruption of the third molar. The included lower third molars can remain asymptomatic throughout life, but sometimes they can develop different clinical-pathological accidents or complications that we can classify as: infectious, tumor, mechanical and nervous processes. The pathogenesis or mode of appearance of these processes tries to be explained by a series of theories: Most theory, Mechanical theory, Capdepont theory and neurological theory [2].
Infectious processes
The most frequent and are centered by pericoronitis. In one study it was found that 64% of third molars with pathology presented this infectious complication, particularly those that presented in an angular and mesioangular position [5]. The term “pericoronitis” designates an acute infectious process that affects the soft tissues surrounding the crown of a partially erupted tooth, mainly of the third molars, is observed in young patients [5] (between the second and third decade of life) and equally in both sexes [2].
The forms of clinical manifestation vary widely depending on local and general factors and the balance between the organic defense system and bacterial activity. So when the infection affects the gingival flap that covers it, it is called operculitis [2].
The etiology of pericoronitis is a function of two factors:
- Active bacterial growth in an ideal environment, which is the soft tissue space that covers the crown of the molar.
- Traumatic irritation of the mucosa that covers the lower molar.
It is believed that among the states that predispose to pericoronitis are upper respiratory infections, emotional stress and pregnancy (in the second trimester) [2-6].
Oral infectious agents develop in the pericoronary space, in one of its recesses, the adjacent mucosa opposes the infection its usual defense reactions, when the defensive process is not able to control the aggression, pericoronitis is exacerbated, presenting itself in different ways:
Congestive or serous acute pericoronitis
It is characterized by marked chewing pains, which can radiate to the pharynx or ascending branch of the jaw, the mucosa behind the molar is erythematous and covers a part of the crown of the molar, sometimes leading to cusp pressure of the molar antagonist. Palpation of the region is painful and may bleed at the least pressure, a simple adenopathy can be palpated in the submandibular lymph node chain, which is located below the mandibular angle in the erupting third molars.
Its evolution is variable; spontaneously or under the effect of a treatment is attenuated. Recurrences can happen until the crown is completely released, but at all times the lesions can pass to the stage of suppurated acute pericoronitis [7].
Pericoronitis suppurated
More intense pains are manifested that radiate to the tonsils and ear. The retromolar region is turgid; the erythema extends to the pharynx and the anterior pillar of the palate veil. Trismus of low intensity, dysphagia appears, palpation is more painful and the pressure on the mucous cap of the tooth causes a small amount of pus to escape. There is presence of adenopathy in the submandibular lymph node chain painful on palpation.
The evolution is similar to that of the congestive or serous form, it may still return, although it is more rare; recurrences are separated by varying periods of pain reduction, and the transition to chronic form is frequent; Although pericoronitis has the danger, above all, of being the starting point of a more serious infectious complication: cell, mucosa, ganglion or bone [7].
- Complications due to bucofacial cellulitis: bucinate-maxillary abscess; supra or inframilohyoid abscess; masseter abscess; diffuse peritonsillar abscesses.
- Mucous complications: odontiatic stomatitis; Vincent’s angina; retromolar mucosal ulceration; broad, torpid and little painful ulceration located in the cap and in the mucosa behind the tailpiece.
- Ganglionic complications: simple or congestive adenitis; suppurative adenitis; adenoflemón.
- Bone complications: osteitis; osteoflemones; ostomyelitis; acute diffuse cortical osteitis.
- Finally, the literature cites the possibility of the appearance of distant complications such as intra and extracranial thrombophlebitis [6], uveitis, mediastinitis, nephritis and endocarditis [2].
Chronic pericoronitis
The symptoms are more attenuated, intermittent retromolar pains. Sometimes it is accompanied by trismus or limitation to the light and temporary opening of the mouth, can occur with absolute absence of symptoms or can be these little manifest, such as marked halitosis, recurrent pharyngitis, torpid gingivitis, chronic adenopathy or unilateral periamigdalin abscesses [2-7].
The tooth is covered with a pressure-sensitive erythematous and edematous mucosa that sometimes releases one or two drops of purulent serosity under the cap. A very typical sign of chronic pericoronitis is unilateral, intermittent and recurrent pharyngitis [7].
The basic pillars to consider in the treatment of these infectious accidents are the use of antimicrobials and surgical treatment, in order to restore the patient's health and avoid the occurrence of sequelae and complications.
They may also develop tumor lesions, cystic formation being the most frequent and usually associated with the inclusion of the third molar [8-9].
Tumor processes
Quiste radicular
They occupy sixty-five percent of the casuistry, and are thought to be formed from the epithelial remains of Malassez, in response to inflammation. Almost all develop from pre-existing periapical granulomas [10].
Clinically, large cysts may involve a complete quadrant with some teeth occasionally with mobility and some without vitality. Root resorption can be found. The cyst is asymptomatic when it is sterile and painful when it is infected [10]. Microscopically, the cyst is described as a wall of connective tissue, which can vary in thickness, a stratified squamous epithelium membrane and a focus of inflammatory cells [10].
The indicated treatment is its exeresis while we extract the responsible tooth [11].
Quiste folicular or dentigerous cust
The dentigerous cyst is one that develops from the enamel organ, wraps the coronary portion of a non-erupted tooth. Dentigerous cysts are the second most frequent odontogenic cysts after root cysts, constituting approximately twenty-four percent of all mandibular cysts [9]. The cyst is formed from the separation of the crown follicle from a non-erupted tooth, and although it may involve a tooth, the lower third molars are the most affected [12]. The incidence by age groups has been different according to the data of various authors, but its occurrence is more frequent in men than in women [13].
Often they are casual findings, clinically the dentigerous cyst is asymptomatic (except in case of secondary infection), but can cause bone cortical expansion and consequently local deformity in some cases [12].
The final diagnosis can only be confirmed histologically after its exeresis [14]. Its treatment logically passes through the cyst removal and in the same act extract the third molar [11]. It is not recommended in these cases to perform marsupialization techniques of the cyst [2].
Queratoquiste
Queratoquiste is a single or multilocular tumor, more frequent, of odontogenic origin, covered by a characteristic parakeratinized stratified epithelium, with an aggressive biological behavior similar to that of a benign neoplasm.
It can appear theoretically in any location of the jaws, although in most cases they occur in the jaw, mainly in the back of the body and in the ascending limb, developing occasionally around the crown of the non-erupted third molar, of the In the same way as a true dentigerous cyst, so it has been postulated that the keratocyst when it appears in this way has undergone a fusion with a preexisting dentigerous cyst [15].
Sometimes we find it within Gorlin-Gortz Syndrome, an autosomal dominant disease, with dermatological and dental alterations, as well as neurological.
Granuloma marginal
It is usually a radiological finding, with a crescent-shaped image, usually located behind the lower third molar, between it and the ascending branch of the jaw [11]. Also at a higher level between molar and tuberosity, although it can be located at any level of the molar crown [11].
Sometimes symptoms of pericoronitis appear which the indication of its exodontics is.
Quiste latero-radicular
They are inflammatory cysts that form along the distal or buccal root surface of the partially impacted mandibular third molars [10]. It usually occurs between one and four percent, according to authors.
Ameloblastoma
It is the most frequent odontogenic tumor. It is a benign, but locally invasive neoplasm derived from the odontogenic epithelium. It can form in the membrane of a follicular cyst but most often it appears independently of the impacted tooth [10]. The lesion is indistinguishable from an odontogenic cyst, so it is mandatory to submit the excised tissue for histopathological examination for diagnostic purposes and to rule out neoplasms [16]. It can be unilocular or multilocular (soap bubble image), so it can be confused with other tumors, hence the importance of the pathological study, it is essential to make differential diagnosis with keratocyst, ameloblastic fibroma, giant cell granuloma, odontogenic myxoma.
Mechanics: space and position problems
One of the controversies, even today, gives rise to prophylactic surgical exodontics after radiographic studies. There are many interventions made on the third molar by identifying a lack of space and alteration in the position of the molar, without having another cause that justifies it [17].
Friedman estimates that, of the ten million third molars extracted annually in the United States, seventy to eighty percent are prophylactic extractions [18]. Of these molars, only twelve percent of them would be impacted during their development, would be associated with pathological conditions and fifty percent of the upper third molars would evolve [19-20].
The British National Institute of Clinical Evidence and the Scottish Intercollegiate Guidelines Network, are unequivocal in their recommendations adopted by the National Health System: “the prophylactic extraction of impacted third molars free of pathology should be discontinued ... There is no scientific evidence to support the benefits of prophylactic extraction of impacted third molars free of pathology ” [21].
The American Public Health Association recommends that the third molar orthodontics be the same indication for another tooth. Not endorsing the prophylactic exodontics of these third molars, giving importance to the risks inherent in the intervention. Being of great importance, informing the patient of the risks of the intervention [22].
Positioning of third molars
There are a large number of classifications, but the most important and most used are Pell and Gregory and the winter classification.
In the different classifications it is important to have a radiographic analysis, since it provides detailed information both of the piece to be extracted and of the anatomy of the region to be evaluated. Panoramic radiography can accurately provide us with such information.
Pell Y Gregory
This classification is based on the relationship of the tailpiece with the second molar and with the ascending limb of the jaw, and with the relative depth of the third molar in the bone.
Relationship of the tailpiece with respect to the ascending limb of the jaw and the second molar
Class I - There is sufficient space between the ascending limb of the jaw and the distal part of the second molar to house the entire mesiodistal diameter of the crown of the third molar.
Class II - The space between the ascending limb of the jaw and the distal part of the second molar is smaller than the mesiodistal diameter of the crown of the third molar.
Class III - All or almost the entire third molar is inside the branch of the jaw.
Relative depth of the third molar in the bone:
Position A - The highest point of the tooth is level, or above the occlusal surface of the second molar.
Position B - The highest point of the tooth is below the occlusal line, but above the cervical line of the second molar.
Position C - The highest point of the tooth is at or below the cervical line of the second molar [23].
Winter classification
Winter proposed another classification assessing the position of the third molar in relation to the longitudinal axis of the second molar. Mesioangular when the axes form an anterior superior vertex angle close to 45°. Horizontal - when both axes are perpendicular. Vertical - when the two axes are parallel. Distoangular - when the axes form an angle of anterior inferior vertex of 45°. Invested - when the crown takes the place of the root and vice versa with a 180° turn. According to the coronal plane they are classified in vestibuloversion if the crown deviates to the vestibule and in linguoversion if it deviates towards lingual [23].
In the upper jaw we can apply the same criteria for the Winter Classification as for Pell and Gregory:
- Relationship of the tooth with respect to the tuberosity of the maxilla and the second molar.
- Relative depth of the third molar in the bone.
- Position of the tooth in relation to the longitudinal axis of the second molar.
Clasification of menedez and garia perla
First Grade: The molar is not covered by its occlusal face or bone or mucosa.
Second Grade: Tailpiece partially covered by mucosa, not bone.
Third Grade: Tailpiece completely covered by mucosa, not bone.
Four Grade: Tailpiece covered by mucosa, partially by bone.
Fifth Grade: Tailpiece completely covered by mucosa and bone
Difficulty index: Koerner
|
Space Relationship |
Value |
|
Mesioangular |
1 |
|
Horizontal/transverse |
2 |
|
Vertical |
3 |
|
Distoangular |
4 |
|
Depth |
|
|
Nivel A |
1 |
|
Nivel B |
2 |
|
Nivel C |
3 |
|
Relationship with the mandibular branch/space available |
|
|
Clase I |
1 |
|
Clase II |
2 |
|
Clase III |
3 |
|
Difficulty index |
|
|
Very difficult |
8-10 |
|
Modernly difficult |
5-7 |
|
Little hard |
3-4 |
Root relationship with maxillary sinus
Roots in relation to the breast: There is no bone or there is only a thin layer of bone between the upper third molar and the maxillary sinus. The extraction of this piece can cause buco-sinus communication.
Relationship with the lower dentary nerve
The situation of the vascular-nervous bundle in relation to the roots of the third molar is very variable, and therefore it is very important to interrelate the radiological image and the chordal relations with the inferior dental nerve. Most frequent positions of the root canal:
-Longual position.
-Contact between the roots of the third molar and the canal on the lingual side.
-Lower tooth in contact with the apex.
-The apexes of the tailpiece are insinuated into the duct.
-Vestibular position.
-Dental duct between the roots of the third molar.
- Lower dental conduit encompassed by the distal roots and in intimate contact with the mesial root.
Wound Healing Post-Exodoncia
Alveolitis is described in most books, as an inflammation of the socket. It has been described as the most frequent manifestation after the exodontics of the third molar in relation to any other exodontics, in many studies we find very high percentages of post-exodontic alveolitis, reaching up to fifty-six percent. But in the most contrasted studies, being in particular between three to four percent [24].
Since the etiology of the condition is not known, the main therapeutic weapon we have is prevention. Epidemiological studies have detected different risk factors in the development of post-extraction alveolitis: the difficulty of extraction, the surgeon's inexperience, the use of oral contraceptives, inadequate intraoperative irrigation, advanced age, female sex, smoking, immunosuppression, and surgical trauma [25]. Many risk factors could actually be a combination of several independent variables, which should instead be aimed at more complete designs [26].
Influence of tobacco on post-exodoncia alveolitis
In the healing of any lesion, a clot must first form. The healing or healing of wounds is a physiological process of great complexity that has the purpose of restoring the integrity of the skin and mucous membranes, thus, any anomaly in its barrier function, which is essential to maintain homeostasis and the general well-being of any individual [27].
The first healing phase confers the inflammatory phase, with the formation of a clot and the cessation of bleeding. This constitutes a dynamic and viable matrix of proteins and cells that contributes not only to hemostasis but also to the arrival of inflammatory cells, fibroblasts and growth factors that are essential for the healing process to take place [27].
In numerous studies, smoking is related as a cause of alveolitis production. Authors such as Blum quantify the increase in the rate of alveolitis in a smoking patient by twenty percent to the patient who smokes a daily package, and increases this probability up to forty percent if the patient smokes on the day of the intervention or immediately to the intervention [28]. Toxic numbers present in tobacco, as well as the effect of suction are the main intermediaries in producing dry socket in smoking patients.
Other influencing factors in alveolitis
- Trauma produced by the surgeon or dentist, little experience in the management of tailpiece surgery, due to thrombosis of the vessels and less resistance of the tissues to infectious processes [29].
- The female sex and especially the use of hormonal contraceptives. Estrogens and other drugs would activate the fibrinolytic system in an indirect way, contributing to the lysis of the clot and the development of alveolitis.
- Intraligamentous anaesthesia, anesthetic deposit very close to the socket and related to the anesthetic being cold, is also influential in the appearance of alveolitis [30].
- Diabetic patients, especially poorly controlled, with high glycated hemoglobins, and in immunosuppressed patients, have a greater tendency to develop post-exodontic alveolitis [31].
OBJECTIVE
Main objective
Influence of factors, before the surgical intervention of the third molar in the production of alveolitis after exodontics.
MATERIAL AND METHOD
Type of study
Descriptive observational study.
Scope of the study
Development of statistical parameters dumps from Excel to SPSS program. Collection of consultation data “High-Resolution of Primary Care Dentistry, Aljarafe Sanitary District, SAS”. High-Resolution Consultation Aljarafe Dentistry.
The main objective of the creation of the High-Resolution consultation in Dentistry is the promotion of Primary Care. With this we contribute to the approach of specialized medicine to our patients, carrying out cooperation programs between Hospital Units and Primary Care Units (a.p.).
This query was born for this purpose. In this area, and in the creation of an improvement area, the collaboration between the Maxilo-facial Surgery Unit of the Virgen del Rocío Hospital with its director D. José Luis Rodríguez Gutiérrez and the Unit of the Dental Support Device Sevilla Norte Aljarafe begins, with its Director D. Alfonso García Palma. In this way, we guarantee the best patient care, where they will be evaluated by a team formed by dentists and maxillofacial surgeons, in a dental practice of a.p.
As a secondary, an increase in competencies will be developed by dentists in the District Sevilla Norte-Aljarafe in the field of surgical pathology of the stomatognathic apparatus, participating in surgical techniques that strengthen and train them in the field of action of the ap, planning dentists rotations for this consultation. Decrease in the demand for appointment for maxillofacial surgery of the Hospital and decrease in emergency care, causing shortening in the appointment schedules of the patient in specialized appointment. Importance to the cancer patient, shortening their study appointments and assessment for the intervention and/or procedures.
The High-Resolution consultation is developed as a center in the dental office of Tomares, given its geographic centrality in the dispersion of Aljarafe patients. A dentist participates in it as a consultant, - Dr. Alfredo Reinoso - who has a consultation every Tuesday of each month, in the morning and a maxillofacial surgeon of the Surgery Unit of the Virgen del Rocío-Dr Hospital. Rodrigo Lozano, who goes on a Tuesday a month, for joint assessment of patients. The patients will be intervened, depending on the pathology, in this cabinet and the patients who need hospital surgical care through the fellow surgeon and its Director D. José Luis Gutiérrez Pérez, will be assigned an appointment.
For the appointment in the consultation, a clinical demand agenda and an agenda of programmed actions are enabled. The dentists of the Aljarafe District can assign patients to this consultation from their cabinet, both on the days of the dentist’s performance and in the joint operation with surgery. Having information on the actions that are performed on their patients, as well as direct communication with the dentist who manages the consultation. For requests for complementary tests, mainly diagnostic imaging tests, they are requested from Primary Care through the computer program.
After agreement in the Dentistry Unit and the Surgery Unit, the inclusions of the referrals to this consultation are determined, which are?
Included are patients for oral surgery:
- Inclusions of root remains.
- Inclusions of cordal.
- Inclusions of canines.
- Dental inclusions.
- Deciduous dentition anquilosis.
- Treatments of odontogenic cysts.
- Cystctomies Apiceptomy.
- Exeresis of benign lesions of the oral mucosa and gum
Fibroids Granulomas Mucoceles…….
- Biopsies for diagnosis: leukoplasias, lichen.
- Biopsy for suspected diagnosis: Ca.
- Biopsy of minor salivary glands for diagnosis of Sjogren.
- Abscess drainage and drainage placement.
- Special patients: committed patients, either because of their medical or pharmacological background.
Exclusion criteria, patients:
- Temporomandibular joint dysfunctions.
- Xerostomía.
- “Síndrome Boca ardiente”.
- TADA patient, with dentistry report enabled, hospital referral demanded.
Study period
First year of the High-Resolution Dentistry consultation of the Aljarafe District, from October 1, two thousand seventeen to June twenty six of the year two thousand eighteen.
Analysis unit
Statistical analysis in SPSS program.
Variables included in the study
Dependent variable
Production of alveolitis after surgical exodontics of the third molar.
Independent variables
Personal history.
Previous pericoronitis, treated.
Koerner index: classified as: index less than or equal to 4, index between 5 and 7, and indexes greater than 8.
Smoker/non smoker.
Confusing variables
Age
Sex
Measure instrument
Statistical analysis in SPSS, after Excel data dumps.
Information sources
Data collected in Diraya
Diraya is the system used in the Public Health System of Andalusia to support electronic medical records. It integrates all the health information of each one of the people attended in the health centers, so that it is available in the place and moment in which it is necessary to assist you, and also serves for the management of the health system.
Analysis plan
Statistical analysis methods used.
Analytical study in SPSS system, analysis of factors according to age, sex, smoker, history of pericoraritis, and Koerner index. Comparison of variables, multiple correlation and logistics.
Justification for the use of these statistical techniques.
RESULTS
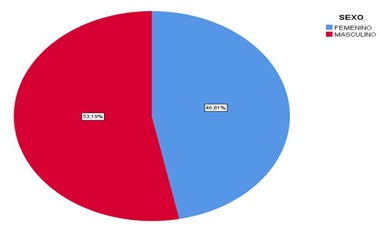
Graph 1: Intervention analysis by sex.
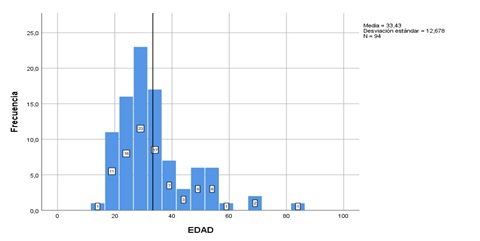 Graph 2: Analysis by age: Average age: 33 years.
Graph 2: Analysis by age: Average age: 33 years.
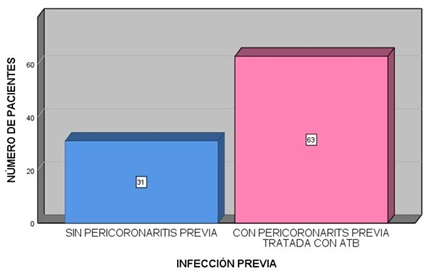 Graph 3: Patient who had previous infections, pericoronitis, before surgery, and as a cause of their intervention, compared to those who have not had pericoronitis.
Graph 3: Patient who had previous infections, pericoronitis, before surgery, and as a cause of their intervention, compared to those who have not had pericoronitis.
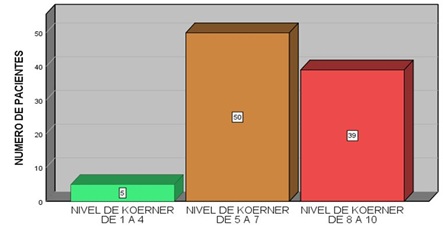 Graph 4: Number of patients according to level of difficulty, Koerner.
Graph 4: Number of patients according to level of difficulty, Koerner.
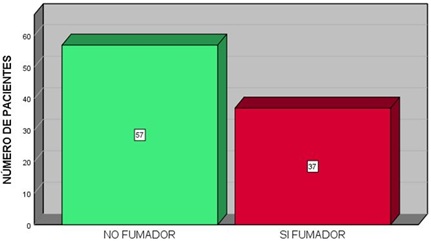 Graph 5: Smoking patients, versus non-smokers.
Graph 5: Smoking patients, versus non-smokers.
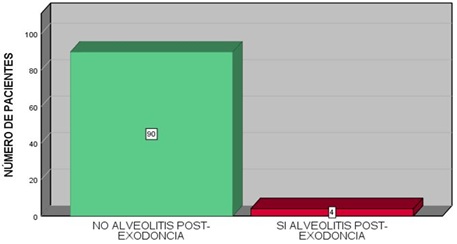 Graph 6: Patients who present with alveolitis after the weekly review.
Graph 6: Patients who present with alveolitis after the weekly review.
Patient being a smoker, after the surgical intervention presents post-exodontic alveolitis. The four patients who presented alveolitis were smokers, so in our study 100% smoked.
|
Correlations |
E.S.I |
Smoker |
|
|
Pearson correlation |
1 |
0.262* |
|
|
E.S.I |
Sig. (bilateral) |
|
0.011 |
|
|
N |
94 |
94 |
|
Pearson correlation |
0.262* |
1 |
|
|
Smoker |
Sig. (bilateral) |
0.011 |
|
|
|
N |
94 |
94 |
*The correlation is significant at the 0.05 level (bilateral).
The four patients who presented alveolitis were smokers, so in our study 100% smoked.
Patient who having presented pericoronitis prior to the intervention that justifies the exodontics, presents alveolitis after the intervention:
|
Correlations |
E.S.I |
INFC.PREV |
|
|
E.S.I |
Pearson correlation |
1 |
0.148 |
|
Sig. (bilateral) |
|
0.155 |
|
|
N |
94 |
94 |
|
|
INFC.PREV |
Pearson correlation |
0.148 |
1 |
|
Sig. (bilateral) |
0.155 |
|
|
|
N |
94 |
94 |
|
The four patients who presented alveolitis, had pericoronitis treated with antibiotic, that is, 100% of the patients who had alveolitis, had pericoronitis prior to the intervention.
The production of alveolitis, taking care of the independent variables previous infections and being a smoker.
|
Correlation |
E.S.I |
INFC.PREV |
Smoker |
|
|
E.S.I |
Pearson correlation |
1 |
0.148 |
0.262* |
|
Sig. (bilateral) |
|
0.155 |
0.011 |
|
|
N |
94 |
94 |
94 |
|
|
INFC.PREV |
Pearson correlation |
0.148 |
1 |
0.009 |
|
Sig. (bilateral) |
0.155 |
0.929 |
||
|
N |
94 |
94 |
94 |
|
|
Smoker |
Pearson correlation |
0.262* |
0.009 |
1 |
|
Sig. (bilateral) |
0.011 |
0.929 |
|
|
|
N |
94 |
94 |
94 |
|
*The correlation is significant at the 0.05 level (bilateral)
For multiple linear regressions, with dependent variable, the production of alveolitis, and independent variables: smoker/non-smoker, previous infection/no previous infection.
|
ANOVAa |
|
|
|
|
|
|
|
Model |
Sum of squares |
gl |
Quadratic mean |
F |
Sig. |
|
|
1 |
Regression |
0.343 |
2 |
0.172 |
4.479 |
0.014b |
|
|
Residue |
3.487 |
91 |
0.038 |
|
|
|
|
Total |
3.83 |
93 |
|
|
|
aVariable dependiente: E.S.I
bPredictores: (Constante), INFC.PREV, Smoker
For logistic regression, with dependent variable, the production of alveolitis, and independent variables: smoker/non-smoker, previous infection/no previous infection and Koerner index (dummy).
|
Codifications of categorical variables |
||||||||||
|
|
Frequency |
Parameter coding |
|
|||||||
|
(1) |
(2) |
|
|
|
||||||
|
ko |
Koerner level from 1 to 4 |
5 |
1.000 |
0.000 |
|
|
||||
|
Koerner level from 5 to 7 |
50 |
0.000 |
1.000 |
|
|
|||||
|
Koerner level from 8 to 10 |
39 |
0.000 |
0.000 |
|
|
|
||||
|
Variables in the equation |
||||||||||
|
|
|
B |
Standard error |
Wald |
gl |
Sig. |
Exp(B) |
|||
|
Paso 1a |
Smoker |
19.108 |
4913.276 |
0.000 |
1 |
0.997 |
198869920.824 |
|||
|
INFC.PREV |
18.353 |
6218.390 |
0.000 |
1 |
0.998 |
93448568.892 |
||||
|
ko |
|
1.424 |
2 |
0.491 |
|
|||||
|
Ko (1) |
1.792 |
1.607 |
1.243 |
1 |
0.265 |
6.000 |
||||
|
Ko (2) |
1.232 |
1.314 |
0.879 |
1 |
0.348 |
3.429 |
||||
|
Constant |
-39.946 |
7925.191 |
0.000 |
1 |
0.996 |
0.000 |
||||
aVariables specified in step 1: Smoker, INFC.PREV, ko.
Being a smoker and having previous infection correlates with a high percentage of being able to suffer alveolitis.
DISCUSSION
The control of the factors that predispose to alveolitis is fundamental, being possible the explanation and the information to the patient, who must stop smoking, both before the intervention and after the intervention, at least after the healing period. Other factors are very controllable such as sex, age, the difficulty of the intervention or the difficulty index due to the position of the tooth included. Given the difference in percentages in studies of post-extraction alveolitis, further study would be necessary, which contrasts the hypothesis that the prevalence factor should be between 3-4% of the disease. Assuming a factor of 3-4%, the number of patients to include, and according to Peduzzi would be much higher, for the realization of a logistic correlation.
CONCLUSION
In the different studies reviewed, they point to tobacco as the main factor in the production of post-exodontic alveolitis, other factors such as previous infections, surgeon's inexperience, the use of oral contraceptives, inadequate intraoperative irrigation, advanced age, being secondary. Female sex, smoking, immunosuppression, and surgical trauma. In our study, we observed the great influence of tobacco and previous infection, treated pericoronitis. The difficulty of the intervention does not influence, having the belief that, with higher difficulty index, greater possibility of alveolitis, given in the study the index of alveolitis in low or medium Koerner scale.
The age of choice the surgical treatment has on average 20-25 years, it is observed that the referral of these patients, in the Public Health Services, is being at a later age, being the age of 33 years the average in the interventions.
REFERENCES
- Archer WH (1975) Oral and maxillofacial surgery (5th edn). Philadelphia, Pennsylvania, USA.
- Gay C, Berini L (1999) Cirugía Bucal (1st edn). Ediciones Ergon SA, Madrid, Spain.
- Mercier P, Precious D (1992) Risks and benefits of removal of impacted third molars. A critical review of the literature. Int J Oral Maxillofac Surg 21: 17-27.
- Rantanen A (1967) The age of eruption of the third molar teeth. Acta Odontol Scand 25: 1-86.
- Knutsson K, Brehmer B, Lysell L, Rohlin M (1996) Pathoses associated with mandibular third molars subjected to removal. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 82: 10-17.
- Gracia A, Ángel M (2002) Valoración clínico-microbiológica de la terapéutica antibiótica en la extracción quirúrgica del tercer molar inferior retenido. Tesis Doctoral, Universidad Complutense de Madrid, Madrid, Spain.
- Rodri?guez MD (1998) Cirugi?a bucal : Patologi?a y te?cnica (2nd edn). Barcelona, Masson, Spain.
- Berge TI (1996) Incidence of large third-molar-associated cystic lesions requiring hospitalization. Acta Odontol Scand 54: 327-331.
- Daley TD, Wysocki GP, Pringle GA (1994) Relative incidence of odontogenic tumors and oral and jaw cysts in a Canadian population. Oral Surg Oral Med Oral Pathol 77: 276-280.
- Underbrink M, Pou A, Quinn FB, Ryan MW (2002) Odontogenic cysts and tumors. Grand Rounds Presentation, Department of Otolaryngology, UTMB, USA.
- Pérez G, Luis J, Ruiz R, Mª M, Lagares T, et al. (2001) El Tercer Molar Incluido. Madrid: Intigraf.
- Ko KS, Dover DG, Jordan RC (1999) Bilateral dentigerous cysts--report of an unusual case and review of the literature. J Can Dent Assoc 65: 49-51.
- Gorod SC, Gerlach KL, Krueger G (1993) Cysts associated with long-standing impacted third molars. Int J Oral Maxillofac Surg 22: 110-112.
- Shah N, Thuau H, Beale I (2002) Spontaneous regression of bilateral dentigerous cysts associated with impacted mandibular third molars. Br Dent J 192: 75-76.
- Saap JP (2005) Patología Oral y Maxilofacial contemporánea. Elsevier España, Pg no: 450.
- Sarmiento ME (1998) Lesiones quísticas asociadas a terceros molares retenidos que requirieron hospitalización. Rev Cubana Estomatol 35: 97-101.
- Torres MAF, Albiol JG, Aytés LB, Gay-Escoda C (2008) Evaluación de la indicación de la extracción quirúrgica de los terceros molares según el cirujano bucal y el odontólogo de atención primaria experiencia en el Máster de Cirugía Bucal e Implantología Bucal de la Universidad de Barcelona. Med Oral Patol Oral Cir Bucal Nov 13: 299-305.
- Friedman JW (2007) The prophylactic extraction of third molars: a public health hazard. Am J Public Health 97: 1554-1559.
- Stanley HR, Alattar M, Collett WK, Stringfellow HR, Spiegel EH (1988) Pathological sequelae of “neglected” impacted third molars. J Oral Pathol 17: 113-117.
- Leonard MS (1992) Removing third molars: a review for the general practitioner. J Am Dent Assoc 123: 77-78.
- NICE (2000) Guidance on the extraction of wisdom teeth. National Institute for Clinical Excellence, London, UK.
- APHA (1997) Evidence-based dental care. American Public Health Association, Washington, DC, USA.
- Escoda CG, Aytés LB (2004) Tratado de cirugía bucal tomo 1. 12: 356-385.
- Jaafar N, Nor GM (2000) The prevalence of post-extraction complications in an outpatient dental clinic in Kuala Lumpur Malaysia--a retrospective survey. Singapore Dent J 23: 24-28.
- Lagares DT, Figallo MAS, Ruíz MMR, Cossío PI, Calderón MG, et al. (2004) Alveolitis seca. Actualización de conceptos. Med Oral Patol Oral Cir Bucal 10: 77-85.
- Rakhshan V (2018) Factores de riesgo comunes de la alveolitis seca después de la extracción dental: una breve revisión narrativa. J Stomatol Oral Maxillofac Surg 18: 30100-30109.
- Marsol IB (2006) Proceso de cicatrización de las heridas. Piel 21: 207-212.
- Blum IR (2002) Contemporary views on dry socket (alveolar osteitis): A clinical appraisal of standardization, aetiopathogenesis and management: A critical review. Int J Oral Maxillofac Surg 31: 309-317.
- Larsen PE (1992) Alveolar osteitis after surgical removal of impacted mandibular third molars. Identification of the patient at risk. Oral Surg Oral Med Oral Pathol 73: 393-397.
- Alexander RE (2000) Dental extraction wound management: A case against medicating postextraction sockets. J Oral Maxillofac Surg 58: 538-551.
- García MJ, Peñarrocha M (1994) Alveolitis seca: Revisión de la literatura y meta-análi Rev Act Odontoestomatol Esp 44: 25-34.
Citation: Santiago AR (2019) Influence of Tobacco and Pericoronitis in the Production of Post-Exodoncia Alveolitis of the Third Molar, Statistical Analysis in SPSS. J Community Med Public Health Care 6: 051.
Copyright: © 2019 Alfredo Reinoso Santiago, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

