
Infrainguinal Revascularization in Patients with Critical Limb Ischemia on End-Stage Renal Disease Patients (ESRD) and Comparison Results with Non-ESRD Population
*Corresponding Author(s):
Javier Rodríguez-PadillaDepartment Of Angiology Vascular And Endovascular Surgery, Hospital Universitario Severo Ochoa, Madrid, Spain
Email:javierrodriguezpadilla@gmail.com
Abstract
Infrainguinal revascularization in end-stage renal disease patients is controversial, despite of patency and limb salvage rates observed in several studies. This study provides more favourable overall survival and amputation free-survival rates than the contemporary study of the same characteristics. The revascularization of patients with ESRD is frequently conditioned by poor survival. With the data we provide, approximately half of the patients were alived and their limbs were salvaged at 3 years, and this is encouraging. Thus, we can be more aggressive in daily practice and offer revascularization in ESRD patients.
Objective: This study analyzed outcomes of Infrainguinal Revascularization (IR) both Open Surgery (OS) and Endovascular Revascularization (ER) with Critical Limb Ischemia (CLI) in patients with and without ESRD.
Patients and Methods: A total of 1188 patients were prospectively collected and analyzed retrospectively. We included 108 (9.1%) patients with ESRD (55 OS and 53 ER) and of them 70 patients (64.8%) receiving hemodialysis. 1080 patients were included in Non-ESRD group (793 OS and 287 ER).
Results: We followed 1188 patients (Mean age 70.2±11.2, 74.5% males). The secondary patency was similar in ESRD vs non-ESRD group at 1 and 3 years (87.6% and 85.3% vs. 82.9% and 81.6%). The limb salvage rates at 1 and 3 years. (83.5%-83.2% vs. 66.0%-77.6% (p=0.194). Overall survival rate was at 1 year 79.6% vs. 91.8% and at 3 years 57.9% vs. 79.1%, p<0.001). Amputation Free Survival (AFS) rate was at 1 year 68.2% vs. 78.8% and at 3 years 45.7% vs. 64.6%, p<0.001). Cox regression analysis showed that hemodialysis was an independent predictor of all causes mortality and AFS (HR=2.38, 95% CI 1.54 - 3.68, p<0.001). Octogenarian patients and coronary disease were independent predictor of all causes mortality (HR=3.05, 95% CI 2.3-4.01, p<0.001) and (HR=1.49, 95% CI 1.14-1.95, p=0.03).
Conclusion: The long-term patency and limb salvage rates in patients who underwent IR with CLI and ESRD was comparable with non-ESRD patients. No significant differences were found in the term of limb salvage or survival when we compared OP and ER. Despite, the overall survival and amputation free-survival rates was poorer in ESRD patients, we advocated for aggressive revascularization in ESRD patients but we must individualize treatment decision and should be offered revascularization for patients with acceptable life expectancy.
Keywords
Critical limb ischemia; Dialysis; End stage renal disease; Infrainguinal revascularization; Vascular surgery
INTRODUCTION
Critical Limb Ischemia (CLI) defines a sub-group of patients with Peripheral Arterial Disease (PAD), who present ischemic pain at rest and/or ulcers and gangrene [1]. Patients with End-Stage Renal Disease (ESRD) have a high incidence and prevalence of PAD. Some studies suggests a prevalence of 27.5-38% in the United States with about 13% having a diagnosis of CLI [2,3], which is more prevalent in dialysis patients compared to non-dialysis kidney failure patients [4]. The most patients with ESRD have multiple systemic comorbidities (diabetes, hypertension, history of smoking, hyperlipidemia) and their arteries are affected by severe calcification and multiple distal occlusions [5,6].
Infrainguinal Revascularization (IR), OS and ER, in patients with ESRD can be challenging and its management remains unclear [5-8]. In the 80-90’s some authors defended primary amputation after observing high rates of amputations with an important associated morbimortality [9,10]. Some authors have advocated the aggressive management of critical limb ischaemia in ESRD patients, based on the observation that patients who undergo amputation are at high risk of subsequent death [11-15].
The aim of our study is to assess the short and long-term outcomes of IR (OS and ER) in term of patency, limb salvage and survival for CLI in ESRD patients.
PATIENTS AND METHODS
A total of 1188 procedures we were done to CLI at the Department of Vascular Surgery, Getafe University Hospital (Madrid-Spain). This research was approved by our Ethical Committee. Epidemiological data, demographics characteristics, operative data and postoperative outcomes were prospectively collected and analyzed retrospectively. The study included patients who underwent OS with infrainguinal bypass with autologous graft and ER (25.4% angioplasty alone 55.8% angioplasty and stenting, 28.8% drug eluted balloon). All patients presented objective clinical criteria that describe patients with typical chronic ischemic rest pain (Fontaine III or Rutherford 4) or patients with ischemic skin lesions, ulcers or gangrene and/or hemodynamic criteria for CLI [1] by the Ankle-Brachial Index (ABI) or toe systolic pressure. Ischemic rest pain most commonly occurs below an ankle pressure of 50 mmHg or a toe pressure less than 30 mmHg. All cases were reviewer and discussed for decision making and daily vascular meetings in our Department. All patients signed informed consent.
The demographic and procedure data in the study (overall series) are shown in table 1. The average patients age was 70.6±8.1 vs. 70.1±11.2 (p=0.701). ESRD group had most patients a history of smoking, DM, hypertension and coronary disease. Ulcer or gangrene was the indication of revascularization in 74.5% (n=886) of the overall cohort (ESRD: 88.0% vs. non-ESRD: 73.2%). The level of revascularization was similar in both groups. Types of revascularization were OS (50.9% vs. 73.4%) and ER (49.1% vs. 26.6%) respectively (Table 2).
|
Patient’s characteristics |
Number of patients (%) |
|
Age (years) Octogenarian |
70.2 ± 11.2 246 (20.7) |
|
Male (gender) |
885 (74.5) |
|
Diabetes Mellitus |
769 (64.7) |
|
Hypertension |
782 (65.8) |
|
Coronary artery disease |
293 (24.6) |
|
Pulmonary disease |
203 (17.1) |
|
Hyperlipidaemia Cerebrovascular disease |
334 (28.1) 164 (13.8) |
|
Smoking |
692 (58.2) |
|
Indication of revascularization |
|
|
Rest pain |
302 (25.4) |
|
Ulcer/gangrene |
886 (74.5) |
|
Level of revascularization |
|
|
Femoropopliteal Below the knee vessels (BTK) |
578 (48.6) 610 (51.3) |
|
Type or revascularization |
|
|
Open surgery Endovascular revascularization ESRD on hemodialysis |
848 (71.4) 340 (28.6) 70 (5.9) |
Table 1: Baseline characteristics and operative data who underwent infrainguinal revascularization for critical limb ischemia.
|
Patient's characteristics |
Overall Series |
||
|
ESRSD |
No ESRD |
p-value |
|
|
Age (years) Octogenarian |
70.61±8.1 70.19±11.2 0.701 14 (13) 232 (21.5) 0.032 |
||
|
Male (gender) |
73 (67.6) |
812 (75.2) |
0.084 |
|
Diabetes Mellitus (DM) |
89 (82.4) |
680 (63.0) |
<0.001 |
|
Hypertension |
90 (83.3) |
692 (64.1) |
<0.001 |
|
Coronary artery disease |
49 (45.4) |
224 (22.6) |
<0.001 |
|
Pulmonary disease |
13 (12.0) |
190 (17.6) |
0.001 |
|
Hyperlipidaemia Cerebrovascular disease |
40 (30.0) 16 (14.8) |
295 (27.3) 148 (13.7) |
<0.032 <0.001 |
|
Smoking |
51 (47.2) |
642 (59.4) |
0.014 |
|
Indication of revascularization |
|||
|
Rest pain |
13 (12.0) |
289 (26.8) |
|
|
Ulcer/gangrene |
95 (88.0) |
791 (73.2) |
|
|
Level of revascularization |
|||
|
Femoropopliteal Below the knee vessels (BTK) |
52 (41.8) 56 (51.9) |
526 (48.7) 554 (51.3) |
|
|
Type or revascularization |
|||
|
Open surgery Endovascular revascularization ESRD on hemodialysis |
55 (50.9) 53 (49.1) 70 (64.8) |
793 (73.4) 287 (26.6) - |
|
Table 2: Baseline characteristics and operative data on patients with and without end-stage renal disease who underwent infrainguinal revascularization for critical limb ischemia in the overall population.
After procedures patients received low molecular weight heparin during their postoperative hospital stay and were treated with 100 mg aspirin once day indefinitely. The patients who placed stent were treated with 75 mg clopidogrel orally for at least one month. Routine follow-up included clinical examination, ankle-brachial index and Doppler ultrasound at 1, 3, 6 and 12 months, and then every year.
Glomerular Filtration (GF) is the best rate to assess renal function. Serum creatinine and GF levels of patients were determined 24 hours before the procedure. Different equations can be used to calculate the GF. We used the MDRD equation: [186 x serum creatinine x patient’s age in years x 1.210 (if black race) x 0.742 (if female)]. Patients were classified according to their GF, into the stages of Chronic Kidney Disease (CKD) defined by the KDOQI guidelines [16].
- GF: >90 ml/min/m2 → CKD class 1
- GF: 60-89 ml/min/m2 → CKD class 2
- GF: 30-59 ml/min/m2 → CKD class 3
- GF: 15-29 ml/min/m2 → CKD class 4
- GF: < 15 ml/min/m2 → CKD class 5
ESRD was defined as those patients with GF <30ml/min/m2, CKD class 4 and 5.
Short-term outcomes (30-day): were analyzed amputation and mortality rates, Major Adverse Limb Event (MALE), Major Adverse Cardiovascular Event defined to coronary artery disease or cerebrovascular disease (MACE). Male included any ipsilateral amputation or vascular re-intervention o the target vessel revascularization.
Long-term outcomes were analyzed primary and secondary patency, limb salvage, overall survival, Amputation Free-Survival (AFS) and freedom from MALE at 1 and 3 years. AFS required the abscense of either amputation or death.
MALE, MACE and freedom from MALE were defined according to the Objective Performance Goals (OPGs) [17]. The patients that underwent procedures with non-autologous graft (only below the knee arteries), as well as emergency procedures for acute embolic limb ischemia and patients with acute renal failure were excluded. In the present study, the CLI treatment outcomes of patients with and without ESRD were compared.
STATISTICAL ANALYSIS
Statistical analysis was performed using SPSS statistical software (SPSS v. 16.0.Inc, Chicago, Ill., USA). For comparison of the demographics and epidemiological data between two groups, a Chi-squared test for categorical variables and the T-student test for continuous variables were used. Difference were considered significant when the P-value was <0.05. Patency, limb salvage, overall survival and amputation free-survival rates were estimated by Kaplan- Meier Methods. The differences in survival rates between both groups were evaluated by Log-Rank Test and the Cox regression methods. Only variables with a p<0.10 in univariate analysis were included in the Cox regression model.
RESULTS
The mean length of the follow-up was 31.5±30.6 months. We included 108 (9.1%) ESRD patients (64.8% on hemodialysis) and 1080 non-ESRD patients. Compared ESRD patients, the non-ESRD group had lower mortality rate at 30-day (5.6% vs. 1.8% (6 vs. 19 patients) (p=0.009). The amputation and MALE rates were 2.8% vs. 5.4% (3 vs. 58 patients) (p=0.24) and 5.6% vs. 12.8% (6 vs. 138 patients) (p=0.028). At 30-day peri-operative MACE rates was 8.3% vs. 4.0% (9 vs. 43 patients) (p=0.035) (Table 3).
|
|
ESRD (%) |
Non-ESRD (%) |
P value |
|
Mortality Amputation MALE (reinterv and amputations) MACE |
5.6 2.8 5.6 8.3 |
1.8 5.4 12.8 4.0 |
0.009 0.24 0.28 0.035 |
Table 3: Early outcomes rates (at-30 days).
Primary and secondary patency rates are illustrated in table 4. Primary and secondary patency rates at 1 and 3 years were 73.8% and 62.5% vs. 68.9% and 59.8%, 87.6% and 85.3% vs. 82.9% and 81.6%, respectively. The limb salvage, overall survival and AFS rates can be observed in table 5. The limb salvage rates at 1 and 3 years was similar (83.5% and 83.2% vs. 66.0% and 77.6% (p=0.194). ESRD patients had significantly lower overall survival (at 1 year 79.6% vs. 91.8% and at 3 years 57.9% vs. 79.1%, p<0.001), and AFS (at 1 year 68.2% vs. 78.8% and at 3 years 45.7% vs. 64.6%, p<0,001) than non-ESRD patients. Freedom MALE was 50.2% vs. 42.4% and 37.9% vs. 28.5% (p=0.18) at 1 and 3 years, respectively (Figure 1).
|
|
Primary patency (%) |
Secondary patency (%) |
||
|
|
1 year |
3 years |
1 year |
3 years |
|
ESRD No ESRD P value |
73.8 68.9 >0.05 |
62.5 59.8 >0.05 |
87.6 82.9 >0.05 |
85.3 81.6 >0.05 |
Table 4: Primary and secondary patency at 1 and 3 years.
|
Limb salvage (%) |
Amputation free survival |
Overall survival |
||||
|
HR (95%CI) |
P value |
HR (95%CI) |
P value |
HR (95%CI) |
P value |
|
|
Octogenarian |
- |
- |
1.65(1.36-2.01) |
0.001 |
3.05(2.3-4.01) |
85.3 |
|
History of smoking |
- |
59.8 |
1.28(0.89-1.48) |
0.036 |
- |
- |
|
Hypertension |
- |
>0.05 |
- |
>0.05 |
- |
>0.05 |
|
Hemodialysis |
- |
- |
- |
- |
2.14(1.42-3.24) |
|
|
Ulcer/gangrene |
2.19 (1.54-3.12) |
0.001 |
1.54(0.97-1.35) |
0.075 |
- |
- |
|
BTK TVR |
1.48 (0.95- 1.96) |
0.001 |
- |
- |
1.51(0.97-2.34) |
0.064 |
|
Coronary disease |
- |
- |
- |
- |
1.49(1.14-1.95) |
0.03 |
|
Hyperlipedaemia |
- |
- |
- |
- |
- |
- |
Table 5: Limb salvage, Amputation free survival and overall survival according to Cox regression analysis.
BTK (Below the Knee Vessel); TVR (Target vessel revascularizated)
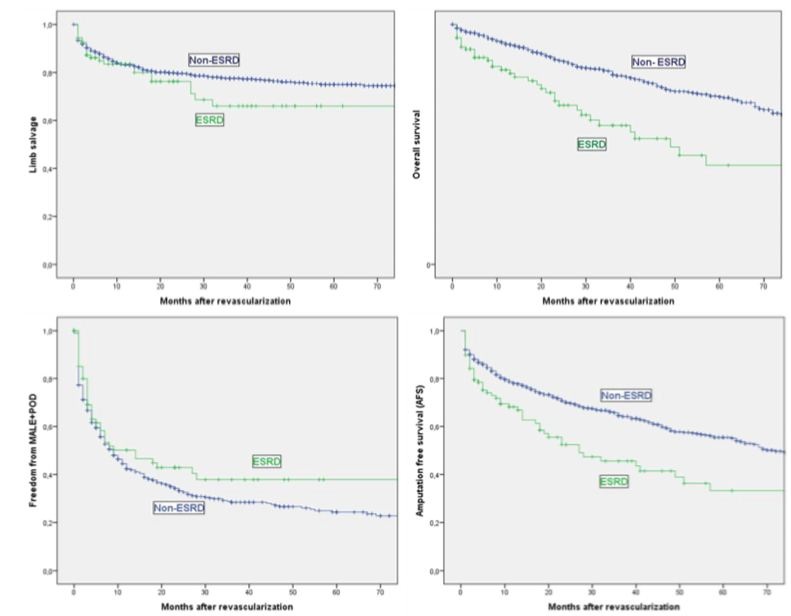
Figure 1: Limb salvage, Overall survival, Freedom from MALE and Amputation free-survival to Kaplan-Meier Methods in ESRD and non- ESRD patients.
Comparing outcomes after OS versus ER within 30 days of the lower extremity revascularization procedure, mortality and major amputation rates were similar. The mortality rate at 30 days in ESRD patients was 5.8 % OS vs 5.1 % ER (p=0.301). Major amputation was 1.9% OS vs 2.9% (p =0.1).
When we compared the outcome in ESRD group between OS and ER, it was found similar result at 1 and 3 years in term of secondary patency (91% and 83.6% OS vs 98.6% and 92.2% ER, p=0.07), overall survival (91.2% and 75.6% OS vs 78.6% and 54.7% ER, p=0.305), limb salvage (80.8% and 58.9% OS vs 86.7% and 73.7% ER, p=0.17), and amputation free survival (63.2% and 58.1% OS vs 78.2% and 56.3% ER, p=0.103).
Independent predictor of limb salvage, overall survival and AFS rates are shown in table 5. Cox regression analysis identified octogenarian patients and coronary disease were associated with significantly higher risk of all causes mortality (HR=3.05, 95% CI 2.3-4.01, p<0.001) and (HR=1.49, 95% CI 1.14-1.95, p=0.03). The patients on hemodialysis was an independent predictor and was associated a higher risk of all causes mortality survival and AFS (HR=2.38, 95% CI 1.54-3.68, p<0.001). The patients underwent infrainguinal revascularization due ulcer or gangrene were a higher risk of amputation (HR=2.19, 95% CI 1.54-3.12, p<0.001).
DISCUSSION
ESRD is a huge problem that is growing. According to the US Department of Health and Human Services, ESRD has increased by 600% over the past three decades [18], approximately 20% of the ESRD patients may need a vascular consultation. For this reason, CLI management of this population can be a challenging and we have to make the effort to find tools that allow us to offer each patient individually the best treatments. Patients with ESRD have higher rates of limb loss and mortality compared with patients with normal renal function [2,19]. In this series, ESRD patients had poorer outcomes with higher mortality and lower limb salvages rates.
The appropriate treatment of CLI in ESRD patients is unclear. Some studies advocated an aggressive approach that achieves good limb salvage rates, although all these studies agree on the poor overall survival rates of long-term [13,20]. A Metanalysis, Albers at al recommend that bypass grafting should not be offered patients with amount of tissue loss or extensive infection [5].
Compared with non-ESRD patients, multiple studies evaluated lower limb revascularization have previously shown ESRD population experience decreased patency, limb salvage, and lower survival rates [4,11]. In despite, several studies and conventional wisdom have historically supported early vascular surgery referral and potential revascularization among ESRD patients.
The present findings differed in certains respects; it was found promising results of long-term overall survival rates in this population against previously reviewed studies. The 30-day peri-operative mortality rates found after IR on ESRD patients (5.6%) was on par with those reported in another studies [2,11,18,21,22]. We suggested that probably, the higher mortality rates on ESRD patients can be explained due the higher MACE rate (8.3%, 9/108 patients). A meta-analysis evaluated the impact of kidney function on the outcome after surgery indicated that relative risk of 30-day mortality according to the decrease of the glomerular filtration. The relative risk was 3.57 (CI 95%) in CKD class 5, particularly after lower limb revascularization [22]. While there was a similar risk of 30-day amputation rate between both groups, the MALE was significantly higher on non-ESRD patients, due higher minor amputation rate in this group. The peri-operative mortality rates found after OS and ER were lower (5.8 % OS vs 5.1 % ER, p=0.301) with those reported in another recent observational database [2].
Some reports have reported different patency rates. It was found an excellent secondary patency in both groups at 1 and 3 years (85.3% vs. 81.6%). This outcomes demonstrate similar patency between ESRD cohort to controls with mild or no renal impairment (p<0.05), according previous studies [23,24]. These data would be suggest the patients might in fact be dying with a patent graft or target vessel revascularizated. Patency rates were markedly superior than data have been previously published in other studies [8,9,11,23].
Despite the excellent results of patency and limb salvage, clinically, independent ambulation and the quality of life are more relevant than these parameters. Some studies reported independent ambulation rates of 10-61% at one year [25-27]. Measures of quality of life in Non-ESRD patients underwent IR is higher to primary amputation, but this is certain in ESRD population [28].
The poor long-term survival, which is a consistent finding in all studies reviewed. In our study, limb salvage rate outcomes were no better than survival rates. Limb salvage, AFS and overall survival at 1 and 3 years were 83.5% and 83.2% vs. 66.0% and 77.6% (p=0.0194), 68.2% vs. 78.8% and 45.7% vs. 64.6%, (p<0.001), 79.6% vs. 91.8% and at 3 years 57.9% vs. 79.1% (p<0.001). These results were indicated excellent limb salvage, improving the overall survival in the ESRD population, although the overall survival rate is still poorer than non-ESRD group. Shroff GR et al., [29] reported a mortality rate at 3 years ESRD patients who underwent coronary revascularization was 42%. This findings support that the severe arteries calcification is determinant of a worse survival in ESRD patients. As aspected, the patients with ulcer or gangrene have a higher risk of amputation (HR= 2.19, 95% CI 1.54 - 3.12, p<0.001).
Patients on hemodialysis was an independent predictor and was associated a higher risk of all causes mortality and AFS (Table 5). Octogenarian patients were independent predictor of all causes mortality. Further, increasing age, increasing time on dialysis, and were also associated with worse outcomes, as in previous studies of ESRD patients; survival rates in this cohort also appear to be worse than the overall ESRD.
Despite the differences in the different approaches in terms of invasiveness, the findings obtained in ESRD patients do not differ between OS and ER. The data from this study not demonstrate that OS was associated with significantly increased risk of both perioperative and long-term survival rate, compared with ER. Furthermore, we observed equivalent long-term outcome of limb salvage. Similar results were seen with amputation free survival. In term of patency rates, there was no difference in both techniques at 1 and 3 years. Fallon et al., with more than 20,000 patients, not reported a difference in overall survival and AFS, however, they reported only stadistically significant difference between the ER and OS groups was improved patency in the endovascular revascularization group. The difference with present study could be part be related to the larger sample size afforded. These findings could call into question the "endovascular first" axiom, although, as the BASIL trial [30], suggested that ER be offered to patients whose life expectancy is less than 2 years, given the peri-operative morbidity and higher first year resource expenditures associated with open surgery.
Consensus regarding the optimal management of CLI in this population has not yet emerged. Nowadays, majority authors have recommended reserving revascularization for patients with favourable survival potential and offering palliative options or primary amputation to the remainder. The decision to employ OS or ER varies among departments. This is probably related to the availability of great saphenous vein for conduit and training of the clinician, the surgical and endovascular skills of the remainder.
Risk stratification should be performed to improve both the safety and the efficacy of IR. Analyzing freedom from MALE half of the patients were amputated al 1 year (50.2% vs. 42.4%) and around a quarter of the patients at 3 years (37.9% vs. 28.5%) (p=0.18). If we analyzed the events of AFS, we observed that the most of them were caused by deaths (70.8%). These data highlight the important mortality associated with ESRD population and importance of identifying patients who can benefit from a more conservative approach.
There are a few studies that analyzed the cost/effectiveness of lower limb revascularization in ESRD patients. To support the decision to proceed revascularization, Barshes NR et al., [31] showed that the ER appears to be a cost-effective compared with a local wound care and primary amputation. In a previous study [32], they found surgical by pass to be a most cost-effective alternative to local wound care based a CLI population similar to PREVENT III trial [33-35], where the incidence of ESRD was 12%. More studies are needed to confirm the cost-effective of limb revascularization in ESRD patients and compared them with healthy population or initial class of CKD.
CONCLUSION
Limb loss is clearly associated loss of independence and quality of life, and the need for institutional care, therefore, an agressive limb salvage effort in ESRD patients can be justified whenever feasible. Despite the poorer mortality and overall survival rates in patients with ESRD in previous cohorts, in this study we observed encouraging long-term results. In addition, the patency and limb salvage rates were comparable with the non-ESRD group. The complete preoperative evaluation emphasizing of age and myocardial ischemia may be beneficial to select the patients who benefit of revascularization. Thus, despite we advocated for revascularization in ESRD patients, we must individualize treatment decision and should not be offered revascularization for patients with deep tissue loss or extensive infection.
FUNDING
The author(s) not received any specific grant form funding agencies in the public, commercial, or not-fit-profit sectors.
CONFLICT OF INTEREST STATEMENT
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
REFERENCES
- Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, et al. (2007) Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). Eur J Vasc Endovasc Surg 33: 1-75.
- Rao A, Baldwin M, Cornwall J, Marin M, Faries P, et al. (2017) Contemporary outcomes of surgical revascularization of the lower extremity in patients on dialysis. J Vasc Surg 66: 167-177.
- Yuo TH, Wallace JR, Fish L, Avgerinos ED, Leers SA, et al. (2019) Editor's Choice - Comparison of Outcomes After Open Surgical and Endovascular Lower Extremity Revascularization Among End Stage Renal Disease Patients on Dialysis. Eur J Vasc Endovasc Surg 57: 248-257.
- Owens CD, Ho KJ, Kim S, Schanzer A, Lin J, et al. (2007) Refinement of survival prediction in patients undergoing lower extremity bypass surgery: stratification by chronic kidney disease classification. J Vasc Surg 45: 944-952.
- Albers M, Romiti M, De Luccia N, Brochado-Neto FC, Nishimoto I, et al. (2007) An updated meta-analysis of infrainguinal arterial reconstruction in patients with end-stage renal disease. J Vasc Surg 45: 536-542.
- Yamamoto S, Hosaka A, Okamoto H, Shigematsu K, Miyata T, et al. (2014) Efficacy of revascularization for critical limb ischemia in patients with end-stage renal disease. Eur J Vasc Endovasc Surg 48: 316-324.
- Lumsden AB, Besman A, Jaffe M, MacDonald MJ, Allen RC (1994) Infrainguinal revascularization in end-stage renal disease. Ann Vasc Surg 8: 107-112.
- Leers SA, Reifsnyder T, Delmonte R, Caron M (1998) Realistic expectations for pedal bypass grafts in patients with end-stage renal disease. J Vasc Surg 28: 976-980.
- Edwards JM, Taylor LM Jr, Porter JM (1988) Limb salvage in end-stage renal disease (ESRD). Comparison of modern results in patients with and without ESRD. Arch Surg 123: 1164-1168.
- Johnson BL, Glickman MH, Bandyk DF, Esses GE (1995) Failure of foot salvage in patients with end-stage renal disease after surgical revascularization. J Vasc Surg 22: 280-286.
- Ramdev P, Rayan SS, Sheahan M, Hamdan AD, Logerfo FW, et al. (2002) A decade experience with infrainguinal revascularization in a dialysis-dependent patient population. J Vasc Surg 36: 969-974.
- Townley WA, Carrell TW, Jenkins MP, Wolfe JH, Cheshire NJ (2006) Critical limb ischemia in the dialysis-dependent patient: infrainguinal vein bypass is justified. Vasc Endovascular Surg 40: 362-366.
- Biancari F, Arvela E, Korhonen M, Söderström M, Halmesmäki K, et al. (2012) End-stage renal disease and critical limb ischemia: a deadly combination? Scand J Surg 101: 138-143.
- Eggers PW, Gohdes D, Pugh J (1999) Nontraumatic lower extremity amputations in the Medicare end-stage renal disease population. Kidney Int 56: 1524-1533.
- Meyerson SL, Skelly CL, Curi MA, Desai TR, Katz D, et al. (2001) Long-term results justify autogenous infrainguinal bypass grafting in patients with end-stage renal failure. J Vasc Surg 34: 27-33.
- Kopple JD (2001) The National Kidney Foundation K/DOQI clinical practice guidelines for dietary protein intake for chronic dialysis patients. Am J Kidney Dis 38: 68-73.
- Conte MS, Geraghty PJ, Bradbury AW, Hevelone ND, Lipsitz SR, et al. (2009) Suggested objective performance goals and clinical trial design for evaluating catheter-based treatment of critical limb ischemia. J Vasc Surg 50: 1462-1473.
- Fallon JM, Goodney PP, Stone DH, Patel VI, Nolan BW, et al. (2015) Outcomes of lower extremity revascularization among the hemodialysis-dependent. J Vasc Surg 62: 1183-1191.
- O’Hare AM, Sidawy AN, Feinglass J, Merine KM, Daley J, et al. (2004) Influence of renal insufficiency on limb loss and mortality after initial lower extremity surgical revascularization. J Vasc Surg 39: 709-716.
- Kodama A, Sugimoto M, Kuma S, Okazaki J, Mii S, et al. (2014) Clinical outcomes after infrainguinal bypass grafting for critical limb ischaemia in patients with dialysis-dependent end-stage renal failure. Eur J Vasc Endovasc Surg 48: 695-702.
- Brosi P, Baumgartner I, Silvestro A, Do DD, Mahler F, et al. (2005) Below-the-knee angioplasty in patients with end-stage renal disease. J Endovasc Ther 12: 704-713.
- Sigala F, Georgopoulos S, Langer S, Baunach C, Papalambros E, et al. (2006) Outcome of infrainguinal revascularization for critical limb ischemia in diabetics with end stage renal disease. Vasa 35: 15-20.
- Harrington EB, Harrington ME, Schanzer H, Haimov M (1990) End-stage renal disease--is infrainguinal limb revascularization justified? J Vasc Surg 12: 691-696.
- Lantis JC 2nd, Conte MS, Belkin M, Whittemore AD, Mannick JA, et al. (2001) Infrainguinal bypass grafting in patients with end-stage renal disease: improving outcomes? J Vasc Surg 33: 1171-1178.
- Korn P, Hoenig SJ, Skillman JJ, Kent IC (2000) Is lower extremity revascularization worthwhile in patients with end-stage renal disease? Surgery 128: 472-479.
- Nicholas GG, Bozorgnia M, Nastasee SA, Reed JF (2000) Infrainguinal Bypass in Patients with End-stage Renal Disease: Survival and Ambulation. Vasc Surg 34: 147-156.
- Harpavat M, Gahtan V, Ierardi R, Kerstein MD, Roberts AB (1998) Does renal failure influence infrainguinal bypass graft outcome? Am Surg 64: 155-159.
- Albers M, Fratezi AC, De Luccia N (1992) Assessment of quality of life of patients with severe ischemia as a result of infrainguinal arterial occlusive disease. J Vasc Surg 16: 54-59.
- Shroff GR, Li S, Herzog CA (2010) Survival of patients on dialysis having off-pump versus on-pump coronary artery bypass surgery in the United States. J Thorac Cardiovasc Surg 139: 1333-1338.
- Adam DJ, Beard JD, Cleveland T, Bell J, Bradbury AW, et al. (2005) Bypass versus angioplasty in severe ischaemia of the leg (BASIL): multicentre, randomised controlled trial. Lancet 366: 1925-1934.
- Barshes NR, Kougias P, Ozaki CK, Goodney PP, Belkin M (2014) Cost-effectiveness of revascularization for limb preservation in patients with end-stage renal disease. J Vasc Surg 60: 369-374.
- Barshes NR, Belkin M (2011) A framework for the evaluation of “value” and cost-effectiveness in the management of critical limb ischemia. J Am Coll Surg 213: 552-566.
- Conte MS, Bandyk DF, Clowes AW, Moneta GL, Seely L, et al. (2006) Results of PREVENT III: a multicenter, randomized trial of edifoligide for the prevention of vein graft failure in lower extremity bypass surgery. J Vasc Surg 43: 742-751.
- Mooney JF, Ranasinghe I, Chow CK, Perkovic V, Barzi F, et al. (2013) Preoperative estimates of glomerular filtration rate as predictors of outcome after surgery: a systematic review and meta-analysis. Anesthesiology 118: 809-824.
- Kimura H, Miyata T, Sato O, Furuya T, Iyori K, et al. (2003) Infrainguinal arterial reconstruction for limb salvage in patients with end-stage renal disease. Eur J Vasc Endovasc Surg 25: 29-34.
Citation: Rodríguez-Padilla J, Varela C, Carrascosa T, March JR (2020) Infrainguinal Revascularization in Patients with Critical Limb Ischemia on End-Stage Renal Disease Patients (ESRD) and Comparison Results with Non-ESRD Population. J Angiol Vasc Surg 5: 036.
Copyright: © 2020 Javier Rodríguez-Padilla, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

