
Is it worth to Operate Patients with a Metastatic Pancreas Carcinoma? Case Report of a Long-Term Survivor after Liver and Lung Metastases Resection
*Corresponding Author(s):
Jolanta WilczynskaDepartment Of Psychiatry, St. Gallen Nord, Zürcherstrasse 30, 9500 Wil SG, Switzerland
Email:jolanta.wilczynska@hin.ch
Urs Huber
Department Of Oncology, Center Zürich AG, Seestrasse 259, 8038 Zürich, Switzerland
Email:urs.huber@ozh.ch
Abstract
Background: We present a case report of a successful and unexpected 9 years long survival (the patient is still alive without tumor recurrence) of a pancreas adenosquamous carcinoma with liver and lung metastasis after distal pancreatic resection with lymphadenectomy, splenectomy, with surgical and radiotherapeutical treatment of metastasis and additional chemotherapy (Remove yellow part). The standard five-year survival for such cases is normally very poor and at rates of 0-9%.
Case presentation: A case report of a 74-year-old man now with an unexpected long 9 year survival of metastatic adenosqamous pancreatic carcinoma who received first palliative neoadjuvant chemotherapy with mFOLFIRINOX in May 2014. After a good response pancreatic tail resection with lymphadenectomy and splenectomy, was performed in March 2015 and local resection (R0) was achieved. Two liver metastases were treated with radiofrequency ablation in separate settings in April 2015. After two years, metachronous metastases were found in the lower lobe of the left lung and they were treated with radiofrequency ablation. Later due to local recurrence subsequent left lower lobe resection in October 2017 was done. Radiotherapy of the chest and an adjuvant chemotherapy with gemcitabine and capecitabine were also performed from November 2017 until April 2018 and followed by GEM and capecitabine from October 2018 until January 2019. Regular follow-up with tumor marker CA 19-9 showed a significant increase in January 2022 (form 31.4kU/l up 167 kU/l in a year period of time). In MRI check-up, a suspicious tumor was found at the lower lobe resection margin. Biopsy was performed in February 2022. The histopathology showed a fibrosis without metastasis. At present, the patient takes part in regular follow-up, survival is 9 years and he is currently recurrence free with 4 years after last tumor occurrence.
Conclusion: We conclude that multimodal treatment with tumor resection incl. treatment of metastasis can be a promising alternative for much selected patients with metastatic pancreatic carcinoma.
Keywords
Chemotherapy of metastatic pancreas carcinoma; Distal pancreatectomy; Metastatic pancreas carcinoma; Pancreas carcinoma; Survival of metastatic pancreas carcinoma
Background
The standard five-year survival for cases with metastatatic pancreatic carcinoma is very poor and ranges between 0-9% [1]. We would like to present our own multidisciplinary experience on a case with a very good long-term outcome.
Case Presentation
At the age of 66 the patient was diagnosed with a 4 cm pancreas tail tumor with synchronous liver metastasis in Positron-Emissions-Tomographie/Computer Tomographie (PET/CT) in 2014 (Figure 1A&1B). Initial CA 19-9 was 181 kU/l (Figure 2) in June 2014. The patient was oligosymptomatic, he had spine pain, fatigue and no significant weight loss. At the age of 65, he had some kind of belly pain and received a CT of the abdomen in 2013, however his pancreas and other organs were clean. In retrospective the cancer was already seen on that CT without liver metastasis (Figure 3). His risk factor for pancreas carcinoma were smoking, regular alcohol consumption and a positive family history for cancer. He was a smoker (30 pack-years (PY)) and quit in 1982. Despite the presence of liver metastasis the patient wished to be operated on. Preoperative the patient received pseudo-neoadjuvant chemotherapy mFOLFIRINOX (15 cycles) from May 2014 until January 2015. After chemotherapy a regression of the tumor, liver metastasis (Figure 4) and CA 19-9 (Figure 2) was observed. However a new 19 mm metastasis of liver occurred. Despite that fact a successful pancreas tail resection with lymphadenectomy and splenectomy was performed on in April 2015. Based on the histopatology the tumor staging was pT3, G3, L0, V1, Pn1, R0. The morphology of the tumor was poorly differentiated adenosquamous carcinoma and tumor size was 2.5 cm diameter. Radiofrequency Ablation (RFA) of liver metastasis were done in April 2015. One year postoperatively diabetes mellitus type 2 was diagnosed and insulin therapy was started in March 2015.
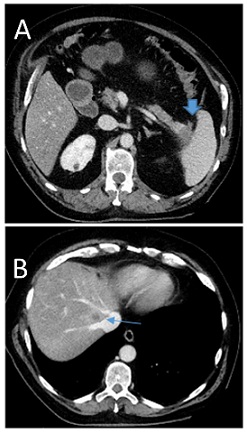 Figure 1: Axial image from a pre-operativ contrast-enchanced CT scan of the abdomen in our patient with pancreastic tail tumor in (A) and 13 mm liver metastasis close next to draining point of liver veins into vena cava inferior (Segment VII) in (B).
Figure 1: Axial image from a pre-operativ contrast-enchanced CT scan of the abdomen in our patient with pancreastic tail tumor in (A) and 13 mm liver metastasis close next to draining point of liver veins into vena cava inferior (Segment VII) in (B).
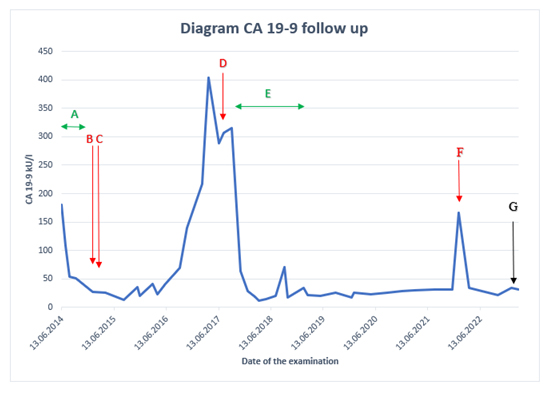 Figure 2: Evaluation of CA 19-9 level follow up 2014-2023. A. The chemotherapy of FOLFIRINOX (15 cycles) from May 2014 until January 2015. B. The first operation pancreas tail resection with lymphadenectomy and splenectomy in April 2015. C. RFA of liver metastases in Segment VI and VII in April 2015. D. RFA and wedge resection of left lung metastasis in October 2017. E. Chemotherapy with gemcitabine and capecitabine (6 cycles) from November 2017 until April 2018, followed by and radiotherapy of 50 Gy (25 fractions a 2 Gy) in 2018 and GEM and capecitabine (4 cycles) from October 2018 until Januar 2019. F. Biopsy of a scar from a lower lobe of the left lung in February 2022. G. CA 19-9 was 27 kU/l in October 2023.
Figure 2: Evaluation of CA 19-9 level follow up 2014-2023. A. The chemotherapy of FOLFIRINOX (15 cycles) from May 2014 until January 2015. B. The first operation pancreas tail resection with lymphadenectomy and splenectomy in April 2015. C. RFA of liver metastases in Segment VI and VII in April 2015. D. RFA and wedge resection of left lung metastasis in October 2017. E. Chemotherapy with gemcitabine and capecitabine (6 cycles) from November 2017 until April 2018, followed by and radiotherapy of 50 Gy (25 fractions a 2 Gy) in 2018 and GEM and capecitabine (4 cycles) from October 2018 until Januar 2019. F. Biopsy of a scar from a lower lobe of the left lung in February 2022. G. CA 19-9 was 27 kU/l in October 2023.
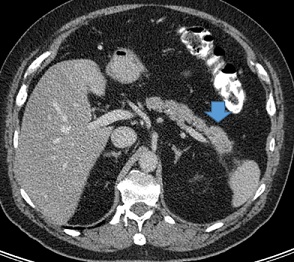 Figure 3: Axial image from a contrast-enchanced CT scan of the abdomen in our patient with 4cm pancreas tail cancer showing a very early stage.
Figure 3: Axial image from a contrast-enchanced CT scan of the abdomen in our patient with 4cm pancreas tail cancer showing a very early stage.
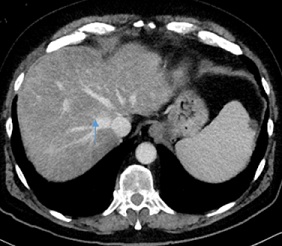 Figure 4: Axial images from a contrast-enchanced CT scan of the abdomen after neo-adjuvant chemiotherapy in our patient with metastatic pancreas tail carcinom showing a regression of liver metastasis.
Figure 4: Axial images from a contrast-enchanced CT scan of the abdomen after neo-adjuvant chemiotherapy in our patient with metastatic pancreas tail carcinom showing a regression of liver metastasis.
In 2017, in the lower lobe of the left lung metastasis was found, the biggest one was about 11 mm in diameter (Figure 5). CA 19-9 was 404 kU/l (Figure 2). The combination a wedge resection and RFA was choosen as treatment and performed in October 2017. KRAS p. Gly12Arg and TP53 p.Arg306Ter tumor mutations were found after retrospective molecular diagnostics. 50 Gy (25 fractions a 2 Gy) radiotherapy of the thorax was also performed in 2018 as well as addivive chemotherapy with gemcitabine and capecitabine (6 cycles) from November 2017 until April 2018 and followed by GEM and capecitabine (4 cycles) from October 2018 until January 2019. Regular follow-up with tumor marker CA 19-9 showed once more a significant increase in January 2022 (form 31.4 kU/l up 167 kU/l in a year period of time) (Figure 2). In MR check up, a suspicious solid component was found in the lower lobe of the left lung (Figure 6), a biopsy was performed in Februar 2022. The histopatology showed fibrotic tissue without metastasis. At present the patient is doing well and is recurrence free. In his life the patient had some additional surgeries such as a radical prostatovesiculectomy due to adenocarcinoma Gleason-Score 6 (1998), epididymectomy (2014), osteoma resection frontal (1990, 2006), a benign tumor resection from left shoulder (2004), osteonecrosis resection right knee (1995) and lipomectomy on the neck (2016).
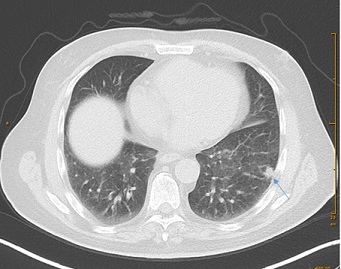 Figure 5: Axial images from a contrast-enchanced CT scans of thorax showing metastasis of a left lung.
Figure 5: Axial images from a contrast-enchanced CT scans of thorax showing metastasis of a left lung.
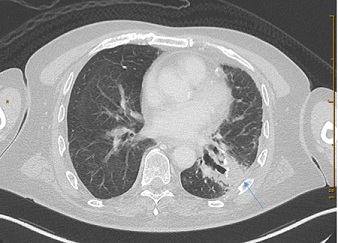 Figure 6: Axial image from a contrast-enchanced CT scan of thorax showing a new suspected scar in a left lung after primary operation.
Figure 6: Axial image from a contrast-enchanced CT scan of thorax showing a new suspected scar in a left lung after primary operation.
Discussion
Pancreatic cancer is a malignant tumor with 500000 deaths each year worldwide and it is placed as 7th highest cause of cancer mortality in the world [1]. A higher incidence rate is observed in well developed countries and for male gender [1]. Pancreatic cancer is late diagnosed because of an asymptomatic beginning, very high aggression and early metastasis [2,3]. About 80% of cases at diagnostic point are advanced and unresectable [1]. The typical metastasis of a pancreatic carcinoma are located in liver (90%), lymph nodes (25%) and lungs (20%) [3]. Patients with liver metastasis have a significantly poorer prognosis than lung or other distant metastasis [3]. Thus the survival for adencocarcinoma of pancreas is very poor and its five-year-survival rate is usually about 0-9% [1]. The presented case patient is currently recurrence free 9 years after diagnosis.
Despite the generally poor prognosis of patients with synchronous liver metastases an individual approach seems indicated. A first line treatment for metastatic pancreatic cancer after symptom control such as management of jaundice, palliative chemotherapy using mFOLFIRONOX is the treatment of choice [3-9]. FOLFIRINOX is a combination of 5-FU, irinotecan, leucovorin and oxaliplatin. The median survival after a chemotherapy is better and has a superior survival based on prognosis analysis, but is generally less than 12 months and in those with liver metastasis less than 6 months [2,3,9]. The combination of chemotherapy and surgery shows an optimal chance of longer survival and quality of life for some patient [5,6,7]. However, in some the disease has developed into unresesectable disease during the course of their chemotherapy treatment [6]. Surgical resection of a pancreatic ductal adenocarcinoma can be curative in about 10-20% [5]. Radical surgery for pancreatic cancer carries a perioperative mortality rate about 3.8% to 10.6% [10]. The combination of chemotherapy and surgery should be evaluated in selective individual cases such as we did.
The study of He from China from 2020 shows that chemotherapy benefited patients with metastases while surgery and radiotherapy could only prolong survival in patients with liver and peritoneum metastases [5]. Our patient at early diagnosis point had a resectable pancreas tail carcinoma with three liver metastasis. He strongly wished a radical surgery despite having a poor survival perspective. His health condition was well enough for surgical treatment. We repected his wishes and decided to start with preoperative pseudo-neoadjuvant therapy with mFOLFIRINOX for other biological selections. The next step was distal pancreatectomy with lymphadenectomy and splenectomy. A successful local R0 resection was achieved. Liver and lungs metastasis can be treated with both classic surgery or RFA. We decided to go for both of them in separate settings. In our case after treatment of late lung metastasis with RFA and after local recurrence with lung resection, radiotherapy and adjuvant gemcitabine and capecitabine chemotherapy was performed as pseudo adjuvant treatment.
Careful follow-up is strongly required for detection of local recurrence or new metastasis, the best combination is tumor marker CA19-9 [8], radiologic imaging with CT or MR and with tumor marker measurement as well as regular discussion in Tumor board meetings [8]. However because of a low positive predictive value of CA 19-9 it has no role in mass screening of asymptomatic patients, but is a first choice marker of monitoring of treatment, recurrence and metastasis.
Conclusion
To our knowledge this is the first case of pancreatic carcinoma with simultaneous liver and even metachronic lung metastases that has survived for 9 years and is as of this publication recurrence free. The patient remains free of recurrence for about 6 years from the last lung metastasis resection. Multimodal treatment with tumor resection and treatment of all metastases in the oligofocal setting can represent a promising alternative for much selected patients with metastatic pancreas carcinoma. Regular follow up with tumor marker CA 19-9 and radiologic images such as CT or MR can help to detect late metastasis or local recurrence. This multidisciplinary individualized therapy can in some cases such as ours achieve longterm survival and quality of life for some patients.
Acknowledgements
Not applicable
Funding
There was no funding for this study.
Role of the Funding Source
There was no funding for this study.
Conflict of Interest
There is no conflict of interest.
Data Availability
Not applicable.
Ethics Approval
Not applicable.
Informed Consent
There is informed consent.
Declaration of Generative AI and AI-assisted Technologies in the Writing Process
Not applicable.
References
- McGuigan A, Kelly P, Turkington R, Jones C, Coleman H, et al. (2018) Pancreatic cancer : A review of clinical diagnosis, epidemiology, treatment and outcomes. World J Gastroenterol 24: 4846-4861.
- Hogendorf P, Durczynski A, Strzelczyk J (2018) Metastatic Pancreatic Cancer. Journal of Investigative Surgery 31: 151-152.
- Cao B-Y, Tong F, Zhang L-T, Kang Y-X, Wu C-C, et al. (2023) Risk factors, prognostic predictors, and nomograms for pancreatic cancer patients with initially diagnosed synchrnous liver metastasis. World J Gastrointest Oncol 15: 128-142.
- Ettrich T, Seufferlein T (2021) Systemic Therapy for Metastatic Pancreas Cancer. Curr. Treat. Options in Onkol 22: 106.
- He C, Huang X, Zhang Y, Lin X, Li S (2021) The impact of different metastatic patterns on survival in patients with pancreatic cancer. Pancreatology 21: 556-563.
- Christians K, Heimler J, George B, Ritch P, Erickson B, et al (2016) Survival of patients with resectable pancreatic cancer who received neoadjuvant therapy. 2016 Elsevier 159: 893-900.
- Uson P, France M, Rodriques H, Macedo A, Goldenberg A, et al. (2015) Higher overall survival in metastatic pancreatic cancer : the impact of where and how treatment is delivered. Einstein 13: 347-351.
- Fogel E, Shahda S, Sendrasegaran K, DeWitt J, Jeffrey E, et al. (2017) A Multidisciplinary Approach to Pancreas Cancer in 2016: A Review. Am J Gastroenterol 112: 537-554.
- Park W, Chawla A, O`Reilly EM (2021) Pancreatic Cancer: A Review. JAMA 326: 851-862.
- Balzano G, Capretti G, Callea G, Cantu E, Carle F, et a. (2016) Overuse of surgery in patients with pancreatic cancer. A nationwide analysis in Italy. HPB (Oxford) 18: 470-478.
Citation: Wilczynska J, Huber U, Helbling D, Siebert S, Winder T, et al. (2023) Is it worth to Operate Patients with a Metastatic Pancreas Carcinoma ? Case Report of a Long-Term Survivor after Liver and Lung Metastases Resection. J Angiol Vasc Surg 8: 113.
Copyright: © 2023 Jolanta Wilczynska, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

