Issues of the Evaluation of Endocervical Cells of the Uterine Cervix on Cytological Smears
*Corresponding Author(s):
Jaroslav HoracekDepartment Of Pathology, University Of Ostrava, Ostrava, Czech Republic
Tel:+420 597372318,
Fax:+420 597375052
Email:jaroslav.horacek@fno.cz
Anton Pelikán
Department Of Surgical Disciplines, University Of Ostrava, Ostrava, Czech Republic
Tel:+420 597375153, +420 602774546
Fax:+420 597375052
Email:anton.pelikan@fno.cz
Hana Hronzová
Department Of Pathology, University Of Ostrava, Ostrava, Czech Republic
Tel:+420 597091766,
Fax:+420 597375052
Email:hana.hronzova@osu.cz
Abstract
The study of cytological and histological changes in the glandular and squamous epithelium of the uterine cervix is important in diagnosis of cervical cancer with the communication between gynecologists and cytopathologists about a definition of suspected neoplastic changes with transitions to adenocarcinoma. The Papanicolaou test (Pap) is a method of cervical screening used to detect these changes for pre-cancerous and cancerous processes in the cervix. A certain diagnostic insecurity in the evaluation of cytological smears arises in the area of abnormalities of the endocervical epithelium from the applied Pap test. Important criteria indicating malignancy are cell palisades, rosettes, feathered cell edges of cell clumps and large cellular cluster. Authors deal in the article with criteria being significant when evaluating cytological endocervical findings. In addition, Human Papilloma Virus (HPV) test may be performed either as indicated for abnormal Pap results.
Keywords
INTRODUCTION
The basic method of cervical cancer screening is cervicovaginal cytology smear and evaluation of fixed and stained cell population from the surface of the cervix and the smear from cervix by light microscopy. Cytological preparations are dyed according Papanicolaou test (Pap test) and findings are expressed in Bethesda System 2001 (The Bethesda System - TBS). In each cytological preparation it is necessary to assess cells cocktail about 50,000-3,00,000 cells. Pap screen testing should begin at age 21. Routine screening is recommended every three years for women 21-65 years old. For women 30 to 65 years who have a normal Pap test with a negative HPV test, screening every five years is considered adequate.
Normal glandular cells are found in the cervical canal of the uterus. It is necessary to carry out proper sampling and then cells retain their shape in the form of strips or remind honeycombs. Their cytoplasm is light-colored, finely granulated in places, often with one or more vacuoles. The cell nucleus is spherical or oval-shaped and is located at the base of the cells and chromatin is fine. They appear in regular groups on cytological smears. The size of the nucleus is approximately 54 μm (Figure 1).
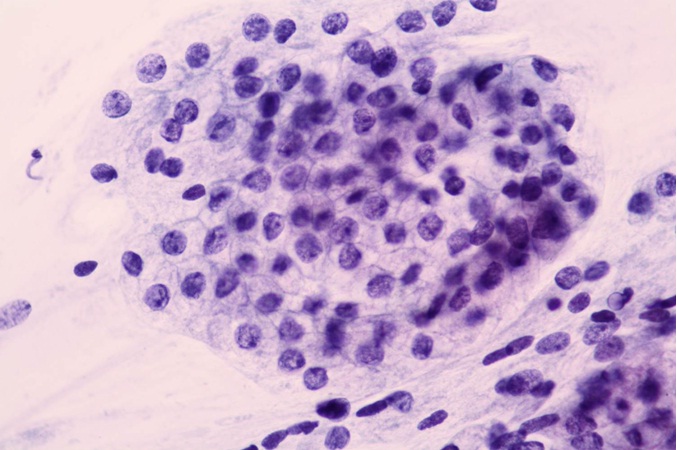 Figure 1: Endocervical cells. Flat sheet of normal endocervical cells in honeycombed pattern, Pap.
Figure 1: Endocervical cells. Flat sheet of normal endocervical cells in honeycombed pattern, Pap.
Endocervical cells may have glandular, cylindrical shape with or without cilia. There are found very often reactive changes in these elements, associated with changing the shape of nuclei with the presence of protruding nucleolus (Figure 2). The presence of endocervical cells in the smear is a condition required quality sampling (Bethesda 2001) [1]. There is a certain diagnostic insecurity in the evaluation of cytological smears arises in the area of abnormalities of the endocervical epithelium from the applied Pap test [2,3].
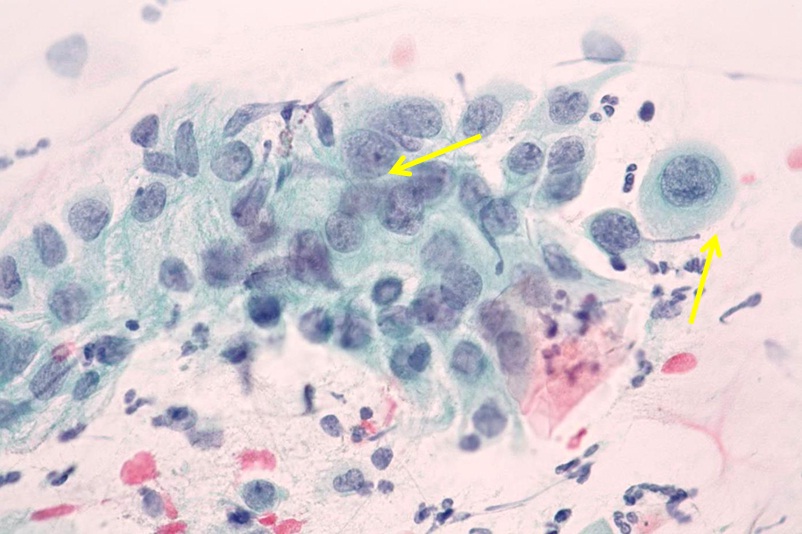 Figure 2: Reactive endocervical cells. Columnar endocervical cells with prominent nucleoli. Slight degree of variation in nuclear size, Pap.
Figure 2: Reactive endocervical cells. Columnar endocervical cells with prominent nucleoli. Slight degree of variation in nuclear size, Pap.
A national cervical carcinoma screening program like in other countries was declared also for Czech Republic in 2007 and was finally anchored in the Bulletin of the Ministry of Health 07/2007. Since that time women with abnormal findings in cervical cytology are invited for further examinations at defined time intervals [4].
ABNORMITIES OF THE ENDOCERVICAL EPITHELIUM
Abnormalities of the endocervical epithelium mentioned by a number of authors [5-7] are not quite suitable material with respect to the evaluation in the form of a PAP test. The sampling origin is the transformation (transitional) zone where is located glandular and squamous epithelium. The endocervical glandular epithelium abnormalities are characterized by loss of nuclear polarity, their overlap, nuclear shape irregularities, loss of cell cohesion, vacuolization of the karyoplasms and cytoplasm (Figure 3).
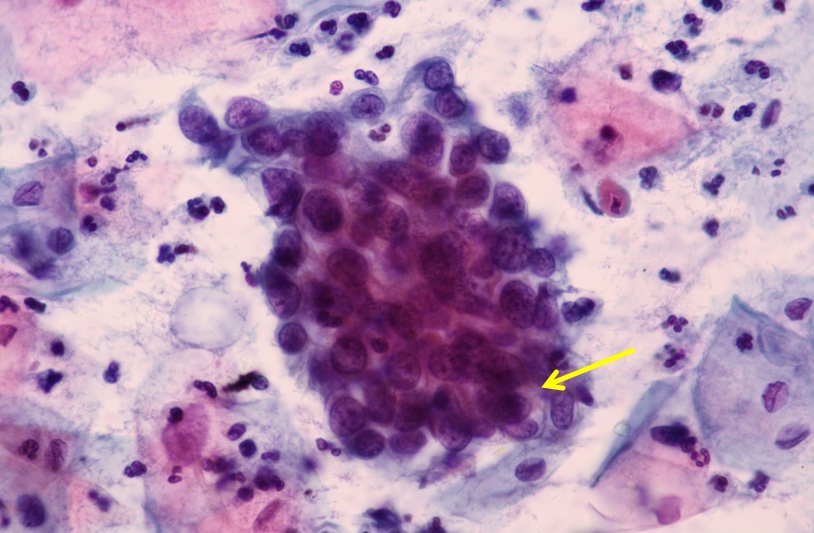 Figure 3: Atypical endocervical cells, probably neoplastic. Three-dimensional cluster of atypical cells. These cells show thickened nuclear membranes and hyperchromasia, Pap.
Figure 3: Atypical endocervical cells, probably neoplastic. Three-dimensional cluster of atypical cells. These cells show thickened nuclear membranes and hyperchromasia, Pap.
Other criteria associated with nuclear hyperchromia, changes in the nuclear membrane and in the chromatin pattern with the prominence of micro nucleoli and with the presence of changes in nucleoplasmatical disparity in favor of the nucleus have been gradually added to these criteria (Figure 4).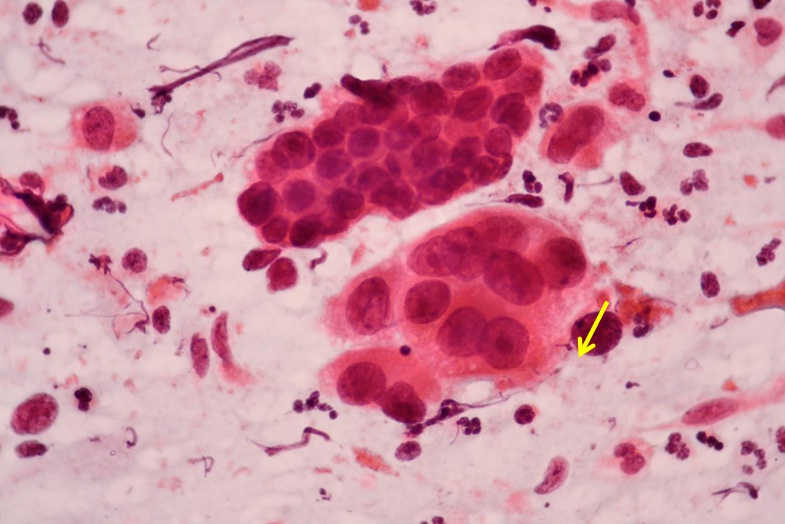 Figure 4: Atypical endocervical cells arranged in rosett-like formation, hyperchromasia, pleomorphism, irregular nuclear contours, Pap.
Figure 4: Atypical endocervical cells arranged in rosett-like formation, hyperchromasia, pleomorphism, irregular nuclear contours, Pap.
Important criteria indicating malignancy are cell palisades, rosettes, feathered cell edges of cell clumps and large cellular clusters (Figure 5). These changes are also characteristic for the adenocarcinoma pattern.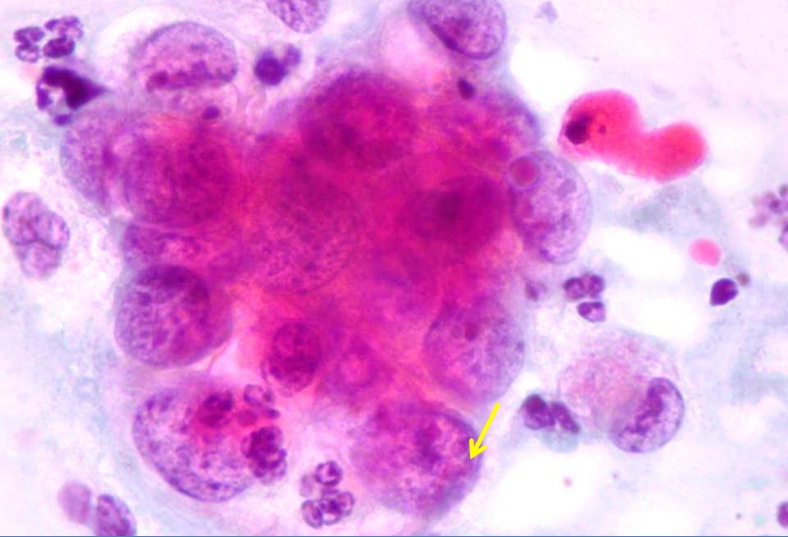 Figure 5: Endocervical adenocarcinoma. Round nuclei, eosinophilic macronucleoli with extensive parachromatin clearing, Pap.
Figure 5: Endocervical adenocarcinoma. Round nuclei, eosinophilic macronucleoli with extensive parachromatin clearing, Pap.
As part of the evaluation of cytological findings of the glandular epithelium according to the Bethesda system for cervical cytology (2004), diagnostic problems cause changes designated as Atypical Glandular Cells (AGC), Not Otherwise Specified cells (NOS) and atypical endocervical cells suspicious for cancer (NEO). With regard to these evaluations, the frequency of AGC-NOS in larger statistical sets is 0.26% and in AGC-NEO 0.03%.
The histological examination as the “golden standard” is found in these cases in the biopsy squamous metaplasia, hyperplasia of reserve cells, reactive epithelial changes, endocervical polyps, endometriosis, tubal metaplasia and the presence of mesonephric ducts. Another significant step towards a proper diagnosis is cytohistological correlation and the examination of demanding preparations under 400-1000x magnification [7-9].
MATERIAL AND METHODS
Our study consisted of a set of 175,000 patients in the age range 16-93 years and had a character of qualitative analysis. From the whole number of patients at 1490 patients were identified atypical glandular cells by cytology (0.85%). Of the 1490 patients were diagnosed AGC-NOS in 1,137 (0.76%) cases and the diagnosis AGC-NEO in 353 (0.23%) cases.
The series 175000 samples were obtained in five cytology departments Moravian-Silesian region - Czech Republic from women who participated regular cervical screening test during year 2013. Cytological material was processed by standard cytological papanicolaou staining method. By verifying the statistical data of these five selected regional workplaces, the percentage difference was in the evaluation range of AGC-NOS from 0.03% to 2% and AGC-NEO from 0% to 1%.
DISCUSSION
Many authors have already studied cytological and histological changes in the glandular and squamous epithelium of the uterine cervix in recent years [10-13]. An important step towards the evaluation of the findings of epithelium abnormalities was in 2001 the Bethesda system which supported the communication between gynecologists and cytopathologists [14,15]. They defined changes in glandular cells with a focus on their atypical shape and a definition of suspect neoplastic changes with transitions to adenocarcinoma in more details. It was crucial to characterize the normal glandular structure of the endocervical epithelium and the changes of beginning, minimal and developed neoplasia. This includes nuclear and cytoplasmic variability.
Significant nuclear changes with the expression of chromatin pattern, the number of nucleoli and participation of macro-nucleoli, nuclear shape with overlap, mitosis, participation of apoptotic bodies and the presence of mucin in cytoplasm. Furthermore there is important to distinguish of tumor changes from pseudoneoplastic lesions define reactive and reparative glandular atypia, intestinal and oxyphilic metaplasia and other [16]. Oncological cytology is a highly specific method about 97%, but is little sensitive about 60%. The sampling of cytological material should cover the whole transformation zone. However, these tests need to be complemented by immunohistochemical methods and in future also take advantage of the possibilities of molecular biology. The role of colposcopy and HPV testing is irreplaceable too [17,18]. Atypical glandular cells of PAP smear should quickly raise the suspicion of malignancy and merits thorough evaluation and close follow up, especially among high-risk women aged more than 50 years [19].
The aim of our study was to draw attention to the changes within the glandular atypia and changes already diagnostic for glandular atypia-atypical glandular cells and cells that already express the transition into the endocervical cancer. These lesions of the glandular endocervical type can in many cases occur concurrently with changes in squamous epithelium which suggests the effect of the virus on both types of epithelia. The coincidence of two epithelial lesions can result in an image adenosquamous carcinoma.
These changes we will continue to monitor and be subject to wider notice in our subsequent publication. For these lesions in their initial phase occurs positivity of HPV infection, which is a sign of incipient viral carcinogenesis caused by a viral effect and there is desirable to repeat a colposcopy with cytological sampling swab with immunohistochemistry using an antibody Ki67 and p16. Atypical Glandular Epithelium (AGC) in the cytological findings are usually up to 39% but in reality they are lesions HSIL (High-grade Intraepithelial Lesion).
CONCLUSION
Regarding the evaluation of cytological endocervical findings we consider the following criteria to be significant:
- Careful evaluation of cell complexes
- Nuclear chromatin pattern
- Chromocenters, micro and macronucleoli
- Thickening of the nuclear membrane
- Nucleoplasmatic disproportion
- Overlapping of nuclei
- Pseudo-eosinophilia
- Nuclear vacuolation and cytoplasm
The most important risk factor for developing cervical cancer is infection with Human Papillomavirus (HPV). There is possible to test for the types of HPV (high-risk or carcinogenic types) that are most likely to cause cervical cancer by looking for pieces of their DNA in cervical cells. Tests for the presence of human papilloma virus are based on the recognition that one of the types of HPV is in the early pathogenesis of cervical cancer. The test HVP DNA is considered in Europe as an adjuvant examination indicated in women over 30 years and is done similarly to the Pap test. According to the American Society for colposcopy and cervical pathology it was stated that Pap smear test is the most successful in history. Experience shows that for women over 30 years of combined carry HPV test with a Pap test. For women with HPV positive test but with negative cytology finding is recommended to test for HPV-16/HPV 18 or m-RNA oncogenes. For women with HPV positive but negative cytology finding is recommended to test for HPV-16/18 or m-RNA oncogenes.
For future is quite important the benefit of immunohistochemical methods in diagnosis and prevention of cervical dysplastic changes including determinations of protein p161ink4a and Ki67, whereby cytoplasmic and nuclear expression could more precisely to clarify cytological diagnosis.
REFERENCES
- Solomon D, Davey D, Kurman R, Moriarty A, O‘Connor D, et al. (2002) The 2001 Bethesda System: terminology for reporting results of cervical cytology. JAMA 287: 2114-2119.
- Dušková J (2010) Falešn? Negativní Pap test? Cytopatolog v Roli Clena Skupiny Znalc? P?i Pozdní Diagnóze Cervikálního Karcinomu. ?es-slov Patol 46: 62-64.
- Dušková J (2012) Co je nového v cytodiagnostice cervikálních prekanceróz? Cesko-slovenská patologie a Soudní lékarství 48-57: 22-29.
- Ondruš G, Dvo?ák V, Dušek L, Májek A (2013) Ambulantní gynekologie. In: Screening karcinomu deložního hrdla. Maxdorf, Czech Republic. Pg: 1-80.
- Kobilková J (2006) Abnormální zmeny bunek žlázového epitelu. In: Gynekologická Cytodiagnostika (2ndedn). Galén, Czech Republic.
- Marquardt K, Griesser H (2014) Die neue Münchener Nomenklatur III: Anwendung in der Praxis. Gyn Praktische Gynäkologie C42058.
- Awatif Al-Nafussi (2006) Histopathological challenges in assessing invasion in squamous, glandular neoplasia of the cervix. Current Diagnostic Pathology 12: 364-393.
- Geisinger KR (2004) Atypical glandular cells of undetermined significance. In: Geisinger KR (ed.). Modern cytopathology. Churchill Livingstone, Philadelphia. Pg: 147-165.
- Horácek J, Kobilková J (2013) Atlas cytohistologických korelací. In: Gynekologická Cytodiagnostika. Maxdorf, Czech Republic. Pg: 136.
- Gloor E, Ruzicka J (1982) Morphology of adenocarcinoma in situ of the uterine cervix: a study of 14 cases. Cancer 49: 294-302.
- Shiozawa T, Shiohara S, Kanai M, Konishi I, Fujii S, et al. (2001) Expression of the cell cycle regulator p27 (Kip1) in normal squamous epithelium, cervical intraepithelial neoplasia, and invasive squamous cell carcinoma of the uterine cervix. Cancer 92: 3005-3011.
- Boon ME, van Ravenswaay Claasen HH, van Westering RP, Kok LP (2003) Urbanization and the incidence of abnormalities of squamous and glandular epithelium of the cervix. Cancer 99: 4-8.
- Ridder R, Wentzensen N, von Knebel Doeberitz M (2003) Biomarker in der Differenzialdiagnostik von HPV-assoziierten Läsionen. Der Gynäkologe 36: 323-330.
- Verma I, Jain V, Kaur T (2014) Application of bethesda system for cervical cytology in unhealthy cervix. J Clin Diagn Res 8: 26-30.
- Mariani R, Grace C, Hughes K, Dietrich RM, Cabay RJ, et al. (2014) Can we improve the positive predictive value of atypical glandular cells not otherwise specified? Diagn Cytopathol 42: 200-204.
- Loureiro J, Oliva E (2014) The spectrum of cervical glandular neoplasia and issues in differential diagnosis. Arch Pathol Lab Med 138: 453-483.
- Dušková J, Beková A, Dvo?ák V, Májek O, Dušek L (2014) [Results of the Czech National Cervical Cancer screening programme]. Klin Onkol 2: 79-86.
- Dvo?ák V, Pilka R (2014) [Role of prebioptic and bioptic methodsin the screening and diagnosis of cervical cancer]. Ceska Gynekol 79: 88-97.
- Carroll R, Goldstein SR (2015) It‘s time to rethink atypical glandular cells on Pap smear. Contemporary OB/GYN.
Citation: Horá?ek J, Pelikán A, Hronzová H (2015) Issues of the Evaluation of Endocervical Cells of the Uterine Cervix on Cytological Smears. J Cytol Tissue Biol 1: 008.
Copyright: © 2015 Jaroslav Horacek, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.