
It’s not a Lung Abscess but it’s a Tumor! A Case of Coexistent Pulmonary Fibrosis and Adenocarcinoma
*Corresponding Author(s):
Rebeca E Vazquez NievesDepartment Of Pulmonary Medicine, Mayaguez Medical Center, Puerto Rico, United States
Tel:+1 7876529200 ; +1 7879410125,
Email:rebecavaz@gmail.com
Abstract
Pulmonary fibrosis is a form of interstitial lung disease that can be secondary to a known source but also of unknown cause. In the case of unknown source, it is called Idiopathic Pulmonary Fibrosis (IPF). Some risks factors for pulmonary fibrosis of known etiology are work related, like Hypersensitivity Pneumonitis, Collagen Vascular Diseases and smoking. It is very common in older adults and has been associated with increased risk for Non-Small Cell Lung Cancer (NSCLC). We present a case of occupational related pulmonary fibrosis and concomitant adenocarcinoma whose initial presentation was necrotizing pneumonia requiring hospitalization.
INTRODUCTION
Pulmonary Fibrosis is characterized by chronic, progressive fibrosing interstitial pneumonia and occurs primarily in older adults with and without smoking history. The patients may present with progressive dyspnea, clubbing, and lung “Velcro-like” sounds upon auscultation. It is characterized by a persistent severe hypoxia and hypoxemia more prominent on exertion. A significant number of patients with pulmonary fibrosis have risk factors, such as history of smoking, emphysema and environmental or occupational exposures. In the case of disease associated to exposures, the antigen is inhaled resulting in accelerated inflammatory response [1,2]. All these risks can predispose the patient to lung cancer [1]. This condition is characterized by a persistent inflammatory state. The patients have an increased incidence of Non-Small Cell Lung Cancer (NSCLC) due to chronic inflammation causing DNA damage [1]. The findings of High Resolution chest CT scan (HRCT) may show area of acute inflammation, fibrosis, honeycombing and/or overlapping features. Biopsy should be considered if the findings are not typical of pulmonary fibrosis or are suggestive of coexisting pathologies in order to direct therapy accordingly.
CASE REPORT
A 62-years-old smoker man was brought to the Emergency Room (ER) complaining of hemoptysis, weight loss, progressive cough, and dyspnea of four months of evolution associated to unquantified weight loss. Three days prior to his admission he started with worsening productive cough of green sputum, general malaise, fatigue and fever. The patient was the owner of a pizza truck and he used to cook burgers in the grill. He was exposed to the steam and flour without wearing any protective gear. One month before admission to our hospital he decided to visit a community pulmonologist because of progressive dyspnea and shortness of breath. A HRCT was recommended that showed findings characteristics of pulmonary fibrosis. A bronchoscopy was performed, but he did not return to the office for discussion of the results.
On evaluation at the emergency room the lung examination was significant for left inspiratory basilar dry crackles and absent right basilar breath sounds. There was no cyanosis or clubbing. He had an adequate oxygenation by pulse oximeter. The laboratories were remarkable for anemia, and increased erythrocyte cell rate 77 mm/hr and C-reactive protein 21.8 mg/dL. No leukocytosis neither bandemia were reported. The Chest x-ray showed increased bilateral interstitial markings and right lower lobe fluid filled cavitation (Figure 1). The Chest CT scan without contrast showed a right lower lobe thick cavity with associated parapneumonic effusion, bilateral interstitial markings, small blebs and paratracheal-hilar lymphadenopathy. In view of his clinical presentation the findings were suspicious for a lung abscess.
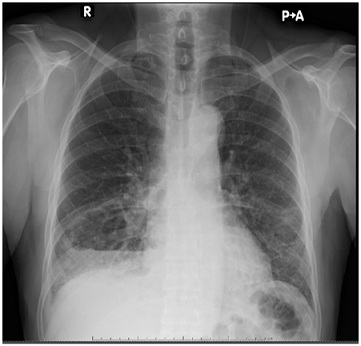
Figure 1: Right lower lobe cavitation and interstitial changes.
The patient was admitted to the Medicine Intensive Care Unit (MICU) due to severe cavitary pneumonia with high risk of complications and the possible need of a chest tube or surgery. During his stay at MICU he received empiric antibiotics. After 3 days of admission a Chest CT scan with IV contrast (Figure 2) reported similar findings suggestive of cavitary pneumonia and/or empyema, but now honeycombing changes were observed in the left lower lung. The IgE levels were normal; the titers for Mycoplasma pneumoniae and Aspergillus were negative as well as the influenza and galactomannan test. The case was consulted to the cardiothoracic surgeon. After the evaluation, the patient underwent right sided thoracotomy with lower lobectomy with mediastinal lymph node dissection and decortication. Intraoperatively a bronchoscopy with Bronchoalveolar Lavage (BAL) was performed. The BAL culture did not show growth of bacteria or fungi. He tolerated the procedure well without complications. The chest tube placed during the surgery was removed during the third post-operative day. The biopsy report (Figure 3) was consistent with invasive adenocarcinoma with acinar predominance with a size of 5.5 cm, no surgical margins involvement and was classified as T3N0M0. The tumor markers were negative for ALK and positive for PDL-1.
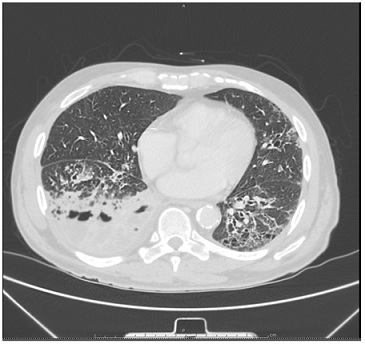 Figure 2: Right lower lobe cavitation and left honeycombing.
Figure 2: Right lower lobe cavitation and left honeycombing.
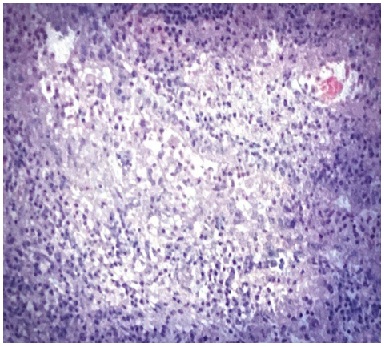 Figure 3: Right lower lung biopsy- Adenocarcinoma.
Figure 3: Right lower lung biopsy- Adenocarcinoma.
On six-minute walk test he was able to walk 300 m with evidence of oxygen desaturation less than 88% for 72% of the duration of the test for which he was started on therapy with oxygen at 3L/minute on exertion and while sleeping. The postoperative spirometry showed moderately severe restrictive ventilator impairment. Upon discharge, he was evaluated by the Oncologist, who recommends starting chemotherapy with Carboplatin and Permetrexed every 21 days for 4 cycles. He achieved remission after completion of four cycles of chemotherapy. His overall functional capacity has improved, now he is able to do his activities of daily living without assistance, including home chores. The oxygen therapy was discontinued. He continues with active surveillance for lung cancer and is pending to do a PET CT scan.
DISCUSSION
The patients with pulmonary fibrosis are at high risk to develop lung cancer. Since 1965 there has been a debate about whether lung cancer may precede pulmonary fibrosis and influence the development of fibrosis, but recent evidence supports the view that lung cancer may also occurs as a late complication of it [3-6]. Some studies have associated the involvement of epigenetics. The most common type of lung cancers is squamous cell carcinomas followed by adenocarcinomas [3].
This case illustrates that pulmonary fibrosis may coexist with NSCLC. Malignancy maybe associated to underlying occupational exposures, smoking or the fibrosis itself. Also, it could be secondary to genetic, molecular and cellular processes. It reminds us of the importance to take into consideration that both conditions may coexist. The Chest CT scan may reveal lobulated-nodular lesions with soft tissue attenuation or ground glass opacities in the absence of a mass or characteristics findings of neoplasm. Also, it is important to take into consideration the use of HRCT in cases of cavitary pneumonia and in the case of a suspicious of an interstitial lung disease. HRCT is able to demonstrate specific features of ILD. Some of these features include ground glass opacities; reticular infiltrates and honeycombing that enable the differential diagnosis to be narrowed [7]. It provides information that cannot be determined from clinical history and spirometry [8]. Therefore, HRCT has an impact in decreasing for surgical lung biopsy and improve management in clinical practice. Sometimes if HRCT is not available or diagnosis is uncertain the tissue biopsy should be considered to institute the adequate treatment. To diagnose lung cancer in the basis of cavitary pneumonia is very challenging. It is a baffling diagnosis and a coin flip to think in cancer when pneumonia is your first diagnosis.
This case shows us that not always what looks like a pneumonia is pneumonia but patient with a diagnosis of pulmonary fibrosis associated to smoking and occupational exposure can present with other pathology like lung cancer. Primary lung cancer cavitation is not uncommon but malignant diagnosis is very challenging because the nonmalignant lesions sometimes mimic malignant ones. The most common histological types are Squamous cell carcinoma and Adenocarcinoma, Lung cavitation related to cancer is secondary to rapid tumor growth that exceeds the blood supply causing necrosis [9]. Cavitation related to cancer is associated with poor prognosis. The relationship between pulmonary fibrosis and cancer was established since 1965 and there are involved multiple common genetic, molecular, and cellular processes [1,3,10-12]. Some of these are myofibroblast activation and uncontrolled proliferation, alterations of growth factors expression, and large genetic and epigenetic variations [1]. Thus, the diagnosis of lung cancer with atypical presentation in a patient with pulmonary fibrosis requires a high index of suspicion and should be considered in any patient presenting with this lung disease. The definitive diagnosis requires tissue biopsy to establish the correct diagnosis and to determine the early treatment to prevent cancer extension and improve survival.
There are some specific antifibrotic agents that are used for Idiopathic Pulmonary Fibrosis (IPF), but recently have been used for cancer related to IPF in combination with chemotherapy. Two of these therapies are Nintedanib and Pirfenidone [1]. Nintedanib is approved as a second line treatment in NSCLC, and Pirfenidone has shown anti-neoplastic effects in preclinical studies. The studies have observed a partial remission of the primary tumor and disseminations [13]. The Nintedanib as a monotherapy have showed to be very effective in patients with NSCLC who are unable to tolerate the cytotoxic effects of chemotherapy [13]. Regarding Pirferidone, it has showed a diminished tumor growth and tumor size in vivo, and to reactivate the local immune in conjunction with current immunotherapies [14]. IPF increases the risk for lung cancer but there are others factors involved to be considered like cellular process dysregulation, epigenetics and genetics. In conclusion, NSCLC should be considered in patients with pulmonary fibrosis. Its diagnosis is very challenging and tissue biopsy may be needed when HRCT is not available or the diagnosis is uncertain. Current approved IPF therapy may be very effective in treating the cancer and the IPF but still uncertain and is under research [1,2,14]. It is important to think in malignancy as a differential diagnosis when cavitation is present in a patient with pulmonary fibrosis. At the moment chemotherapy and immunotherapy are the only therapies that have been described for lung cancer related to non-IPF. The early diagnosis and treatment may prevent cancer extension.
REFERENCES
- Ballester B, Milara J, Cortijo J (2019) Idiopathic Pulmonary Fibrosis and Lung Cancer: Mechanisms and Molecular Targets. Int J Mol Sci 20: 593.
- Bargagli E, Bonti V, Ferrari K, Rosi E, Bindi A, et al. (2017) Lung Cancer in Patients with Severe Idiopathic Pulmonary Fibrosis: Critical Aspects. In Vivo 31: 773-777.
- Yoo H, Jeong BH, Chung MJ, Lee KS, Kwon OG, et al. (2019) Risk factors and clinical characteristics of lung cancer in idiopathic pulmonary fibrosis: a retrospective cohort study. BMC Pulmonary Medicine. BMC Pulm Med 19:149.
- Park J, Kim DS, Shim TS, Lim CM, Koh Y, et al. (2001) Lung cancer in patients with idiopathic pulmonary fibrosis. Eur Respir J 17: 1216-1219.
- Le Jeune I, Gribbin J, West J, Smith C, Cullinan P, et al. (2007) The incidence of cancer in patients with idiopathic pulmonary fibrosis and sarcoidosis in the UK. Respir Med 101: 2534-2540.
- Matsushita H, Tanaka S, Saiki Y, Hara M, Nakata K, et al. (1995) Lung cancer associated with usual interstitial pneumonia. Pathol Int 45: 925-932.
- Turner-Warwick M, Lebowitz M, Burrows B, Johnson A (1980) Cryptogenic fibrosing alveolitis and lung cancer. Thorax 35: 496-499.
- Daniels CE, Jett JR (2005) Does interstitial lung disease predispose to lung cancer? Curr Opin Pulm Med 11: 431-437.
- Mueller-Mang C, Grosse C, Schmid K, Stiebellehner L, Bankier AA (2007) What every radiologist should know about idiopathic interstitial pneumonias. Radiographics 27: 595-615.
- Elicker BM, Kallianos KG, Henry TS (2017) The Role of High-Resolution Computed Tomography in the Follow-Up of Diffuse Lung Disease: Number 2 in the Series "Radiology" Edited by Nicola Sverzellati and Sujal Desai. Eur Respir Rev 26: 170008.
- Shiratori T, Tanaka H, Tabe C, Tsuchiya J, Ishioka Y, et al. (2020) Effect of Nintedanib on Non-Small Cell Lung Cancer in a Patient With Idiopathic Pulmonary Fibrosis: A Case Report and Literature Review. Thorac Cancer 11: 1720-1723.
- Marwitz S, Turkowski K, Nitschkowski D, Weigert A, Brandenburg J, et al. (2020) The Multi-Modal Effect of the Anti-fibrotic Drug Pirfenidone on NSCLC. Front Oncol 9: 1550.
- Selman M, Pardo A, King Jr TE (2012) Hypersensitivity Pneumonitis: Insights in Diagnosis and Pathobiology. Am J Respir Crit Care Med 186: 314-324.
- Gill R, Matsusoka S, Hatabu H (2010) Cavities in the Lung in Oncology Patients: Imaging Overview and Differential Diagnoses. Appl Radiol 39: 10-21.
Citation: Nieves REV, Dionisi ME, Ramos DV (2020) It’s not a Lung Abscess but it’s a Tumor! A Case of Coexistent Pulmonary Fibrosis and Adenocarcinoma. J Angiol Vasc Surg 5: 042.
Copyright: © 2020 Rebeca E Vazquez Nieves, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

