
Laparoscopic-Assisted Transhiatal Esophagectomy in Squamous Carcinoma after Bipulmonary Transplant
*Corresponding Author(s):
Cristina Alegre TorradoGeneral And Digestive Surgery Department, Esophagogastric And Bariatric Surgery Unit, “12 De Octubre” University Hospital, Madrid, Spain
Tel:+34 913908386,
Email:cristina.alegre2006@gmail.com
Abstract
Background: Advances in immunosuppression have made possible to prolong survival of lung transplant patients. It is well known that immunosuppression treatment is associated with an increased risk to develop de novo tumors, being infrequent the appearance of esophageal malignancies.
Surgical treatment of esophageal cancer is associated with high morbidity and mortality, and usually requires a transthoracic approach.
Case Description: We report the case of a 58-year-old patient with squamous cell esophageal cancer after a bilateral lung transplant. Thoracotomy or thoracoscopy were ruled out due to pleural adhesions and high risk of respiratory complications. Laparoscopic-assisted transhiatal esophagectomy was performed, with gastric tubulization. Histopathological analyses showed ypT3N0 poorly differentiated Squamous Cell Esophageal Cancer (SCEC), with negative resection margins. The patient developed a cervical fistula on ninth postoperative day, being treated with a stent and antibiotic therapy with good outcome.
Conclusion: Bipulmonary transplant patients undergoing esophagectomy for cancer have an increased risk of postoperative complications. Multidisciplinary guidance is mandatory in order to propose the best surgical approach.
Keywords
Esophageal cancer; Laparoscopic esophagectomy; Lung transplant
Abbreviations
SCEC: Squamous Cell Esophageal Cancer
PET: CT-Positron Emission Tomography
Introduction
Esophageal cancer is one of the most common causes of cancer deaths worldwide. Although is not one of the most frequent tumor location in the United States, it has a high incidence in countries from the so called “esophageal cancer belt” (from Northern Iran through the central Asia to North-Central China) [1]. In 2018 about 572,034 new esophageal cancer cases were diagnosed worldwide with 508,585 deaths. That year in Spain there were 2,311 new patients diagnosed and 2,026 deaths [2]. In the United States, Squamous Cell Esophageal Cancer (SCEC) has decreased over the last 10 years, being squamous dysplasia the main risk for developing it [3]. There are many risk factors associated to SCEC like tobacco and alcohol abuse, diet poor in fruits and vegetable, with a predominance in males and African Americans [3].
Patients who underwent solid organ transplantation have a high risk for developing de novo tumors, different studies found three-to-five-fold increased risk of neoplasia. Higher incidence has been attributed to decreased immunosurveillance, activation of oncogenic viruses, chronic stimulation of the immune system and carcinogenic effects of immunosuppressants on pre-existing cancer risk factors. Cancer incidence differs according to the transplanted organ, being the higher incidence observed in lung transplant recipients (6-fold increased risk) [4,5].
Surgical treatment of SCEC is associated with a high morbidity and mortality, especially in patients with lung transplant with potential risk of pneumonia, respiratory failure and sepsis [6]. Lung transplantation has increased in the past decades, making it a challenge to perform esophageal surgery in this patients, not only because the added technical difficulty in surgical access, but also because of the importance of preventing lung damage or associated respiratory dysfunction.
We present the following case in accordance with the CARE reporting checklist.
Case Description
A 58-year-old male patient who underwent bilateral lung transplant due to pulmonary hypertension 6 years earlier, and a past personal history of type 2 diabetes, atrial flutter, sleep apnea syndrome and steatohepatitis, and immunosuppressive therapy with tacrolimus, mycophenolate and prednisone. The patient presented a 4-month history of dysphagia with mild weight loss. Endoscopy revealed an esophageal tumor in middle thoracic esophagus (Figure 1) with a histological diagnosis of SCEC, staged as TxN1M0 by CT-scan and CT-Positron Emission Tomography (PET) (Figure 2). After multidisciplinary team meeting, the patient received 4 weekly cycles of neoadjuvant chemotherapy with carboplatin AUC 2 and Paclitaxel 60mg/m2, without radiotherapy because of lung radiotoxicity risk. After finishing neoadjuvant treatment, a new PET was performed showing tumor progression but without tracheal or bronchial infiltration. The patient was proposed for surgery assuming high risk of medical and surgical complications. Laparoscopic-assisted transhiatal esophagectomy was performed, with a gastric tubulization using Akiyama method, hand-sew cervical anastomosis, and a jejunostomy tube was placed for enteral feeding. Thoracoscopic access was discarded because of bilateral lung transplant past history. No lymphadenectomy was performed for subcarinal or tracheobronchial nodes to avoid the risk of bronchial isquemia.
 Figure 1: Preoperative upper endoscopy.
Figure 1: Preoperative upper endoscopy.
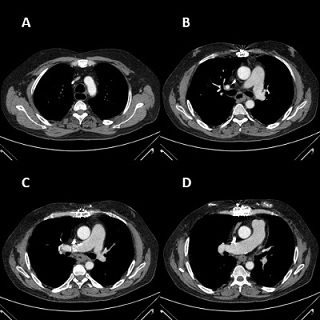 Figure 2: (A, B, C, D) Preoperative chest computed tomography.
Figure 2: (A, B, C, D) Preoperative chest computed tomography.
The patient was extubated on second postoperative day without incidences with initiation of immunosuppression with tacrolimus and mycophenolate through jejunostomy the first postoperative day and enteral nutrition the second postoperative day. The fourth postoperative day the patient developed a cervical hematoma with airway compromise, being necessary surgical revision. On ninth postoperative day the patient was diagnosed of cervical fistula, proceeding to esophageal stent insertion being needed stent repositioning due to migration. Posterior, patient evolution was satisfactory initiating oral clear liquids on 37th postoperative day and being discharged on 40th postoperative day. The stent was removed 2 months later without incidents. The patient had no postoperative respiratory or vascular complications.
The histopathological analyses showed ypT3N0 poorly differentiated SCEC with perineural invasion without lymphovascular invasion and negative resection margins. The patient remained with good oral intake and without impairment of respiratory function, but with mediastinal and retroperitoneal recurrence in CT-scan 1 year after surgery with disease progression, dying 4 months later.
Discussion
Patients on immunosuppressive treatment after lung transplantation are at high risk of developing de novo tumors having six-fold elevation in overall cancer risk. Even though gastrointestinal cancer is one of the most common, esophageal cancer are relatively rare [5,7].
Morbidity and mortality of patients who undergo esophagectomy is high. In patients with surgical antecedents of bilateral lung transplantation, the risk is not only surgical but also anesthetic/medical, being complications such as pneumonia, respiratory distress or sepsis higher [6]. Preserving graft function and avoiding rejection is paramount.
There are few articles published in the literature about patients undergoing esophagectomy after lung transplantation [5,6,8]. It is known that the introduction of minimally invasive approach through laparoscopy and thoracoscopy produces earlier recovery, with less blood loss and analgesia requirement and shorter hospital stays, but in our patient, due to past bilateral lung transplant, it was only possible to perform an assisted laparoscopic approach for a transhiatal esophagectomy, discarding the possibility of thoracoscopy because of expected dense adhesions and risk of lung damage. Transhiatal approach avoid, not only lung collapse and manipulation, but also increased immune response. Lung transplantation, promoting adhesions, makes thoracoscopic access more difficult and therefore the performance of a correct lymphadenectomy. In addition, donor bronchi are poorly irrigated, so it is important to avoid vascular injuries. Transhiatal approach could be consider a suboptimal surgery which may condition the overall and disease-free survival of the patient.
This patient, in addition to presenting a higher anesthetic risk and a poorly differentiated tumor, have a worse oncological prognosis given their immunosuppressive condition, so it is essential to have an adequate study of the case, and a multidisciplinary team treatment decision, as well as to fully inform the patient [8].
Conclusion
In conclusion, bipulmonary transplant patients undergoing esophagectomy for cancer have an increased risk of postoperative complications. Intense intrathoracic adhesions can promote high risk of pulmonary air leak and hinder lymphadenectomy which could be associated to pulmonary oedema and other complications.
Multidisciplinary guidance and management are mandatory in order to propose the best surgical approach.
It is important to assess, based on the preoperative histology findings, the associated risk and its prognosis and the balance of risk and benefits of surgical intervention in this patient.
Author’s Contribution
- Conception and design: Cristina Alegre Torrado
- Administrative support: Cristina Alegre Torrado and Elías Rodríguez Cuéllar
- Provision of study materials or patients: All authors
- Collection and assembly of data: Cristina Alegre Torrado
- Data analysis and interpretation: Cristina Alegre Torrado y Elías Rodríguez Cuéllar
- Manuscript writing: All authors
- Final approval of manuscript: All authors
Acknowledgment
I want to thank all the authors the implication for the performance of this article.
Funding
None
References
- Batra R, Malhotra GK, Singh S, Are C (2019) Managing squamous cell esophageal cancer. Surg Clin North Am 99: 529-541.
- Ferlay J, Colombet M, Soerjomataram I, Dyba T, Randi G, et al. (2018) Cancer incidence and mortality patterns in Europe: Estimates for 40 countries and 25 major cancers in 2018. Eur J Cancer 103: 356-387.
- Arnold M, Soerjomataram I, Ferlay J, Forman D (2015) Global incidence of oesophageal cancer by histological subtype in 2012. Gut 64: 381-387.
- Acuna SA (2018) Etiology of increased cancer incidence after solid organ transplantation. Transplant Rev (Orlando) 32: 218-224.
- Fukutomi T, Taniyama Y, Sato C, Okamoto H, Niikawa H, et al. (2022) A Case of Esophageal Cancer Treated by Thoracoscopic Esophagectomy after Bilateral Cadaveric Lung Transplantation. Ann Thorac Cardiovasc Surg 29: 200-205.
- Walsh SM, Maphango N, Egan JJ, Reynolds JV (2015) Successful surgical management of early esophageal cancer in a patient with cystic fibrosis post-bilateral lung transplantation. BMJ Case Rep 2015: 210342.
- Fink AK, Yanik EL, Marshall BC, Wilschanski M, Lynch CF, et al. (2017) Cancer risk among lung transplant recipients with cystic fibrosis. J Cyst Fibros 16: 91-97.
- Toyama H, Saito K, Takei Y, Saito K, Fujimine T, et al. (2016) Perioperative management of esophagectomy in a patient who previously underwent bilateral lung transplantation. JA Clin Rep 2: 15.
Citation: Torrado CA, Cuéllar ER, Zapata AP, García-Gallardo DH, Aguilar MO, et al. (2025) Laparoscopic-Assisted Transhiatal Esophagectomy in Squamous Carcinoma after Bipulmonary Transplant. J Surg Curr Trend Innov 9: 65.
Copyright: © 2025 Cristina Alegre Torrado, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

