
Laparoscopic Management of Assessory Gall Bladder & Tips for Surgeons
*Corresponding Author(s):
Dr. Monika GuptaHepatico Pancreaticobiliary And Minimal Access Surgery, Department Of Gastrointestinal, Manipal Hospital Jaipur, Rajasthan, India
Tel:+91 9571450766,
Email:guptamons1506@gmail.com
INTRODUCTION
Duplicated gall bladder occur one in 4000 cases, varying from diverticulum of gall bladder to a separate gall bladder with separate cystic duct. Awareness of this anomaly is essential while doing laparoscopic or open surgery in order to avoid inadvertent injury to biliary system. In fact it’s also imperative to know the anomaly preoperatively so that surgeon removes whole gall bladder tissue which may cause similar symptoms in later life and there are chances that surgeon may get sued just for a trivial cause, for leaving symptomatic gall bladder behind.
CASE REPORT
This a case of 26 yrs. old female presenting to Department of Gastrointestinal, Hepatopancreatico-biliary and Minimal access surgery with history of colicky pain right hypochondrium off and on for last 15 days, there was no history of pancreatitis or cholangitis. She was worked up with a sonography abdomen which showed presence of double gall bladder. Her LFT was normal, so in order to rule out anatomical ductal anomalies and to confirm findings of accessory gall bladder, MRCP was done. MRCP showed double gall bladder with pericholecystic collection and wall edema and stones in Gall bladders and cystic duct ,CBD was clear (Figure 1).
 Figure 1: MRCP showing separate gall bladder lumen and cystic ducts.
Figure 1: MRCP showing separate gall bladder lumen and cystic ducts.
Its protocol in our department to perform MRCP whenever LFT is deranged. Considering this as sufficient for workup of a patient presenting with duplicated gall bladder case was posted for laparoscopic cholecystectomy which was then performed successfully. Intraoperative findings were double gall bladder adherent to each other with separate cystic ducts entering the CBD at 1 cm distance. Both gall bladders had separate cystic ducts and arteries which were clipped separately. Both gall bladders had stones and were inflamed. Duration of surgery was 90 minutes, estimated blood loss was 50 cc, no drain was inserted and patient was discharged on day 2. Postoperatively patient followed up on day 8 for stitches removal, thereafter patient remained asymptomatic.
DISCUSSION
Most cases of gall bladder duplication are diagnosed incidentally .Presentation has been found in all age groups in literature. Asymptomatic cases should be followed up and symptomatic cases should undergo surgery. During preoperative workup awareness among surgeons and radiologists about its anatomy is of crucial importance for a successful outcome [1]. In this case patient presented at 26 years of age with stones in both of gall bladders and inflammation.
Duplication of the gallbladder is the result of a rare bifid embryonic diverticulum of the hepatic duct occurring during the fifth or early in the sixth embryonic week. It is a rare entity found in 0.03% of autopsy studies [2]. Symptomatic accessory gall bladder is further rare. The commonly used classifications are the Boyden, Gross and Harlaftis classifications.
According to Boyden’s classification, main types of duplication are:
- Vesica Fellea Divisa or bilobed GB and
- Vesica fellea duplex or true duplication with two different cystic ducts.
The true duplication is sub classified as:
(a) Y shaped type (two cystic ducts unite before entering the CBD). Usually the two GBs are adherent and occupy the same fossa.
(b) H shaped type (two separate GB & cystic ducts entering separately into the CBD [3-6].
Harlaftis et al classified double gallbladders into three categories. Type I was the split primordium group (septate V-shaped and Y-shaped), type II was the accessory gallbladder group (H-type or trabecular pattern) and type III included any anomaly that could not be classified into the above two groups (Figure 2) [2].
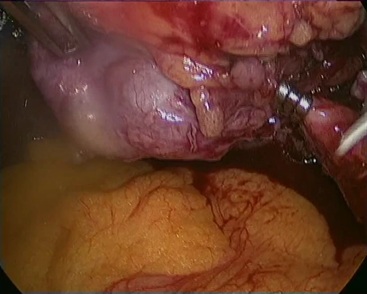 Figure 2: Intraoperative picture showing laparoscopic removal of second gall bladder and cystic duct.
Figure 2: Intraoperative picture showing laparoscopic removal of second gall bladder and cystic duct.
Caster and Flannery categorised cystic duct duplication into 3 types: (1)¨Y¨type, wherein 2 cystic ducts join to form a single cystic duct that then enters the CBD, (2)¨H¨type, in which each cystic duct independently joins the bile duct system at the CBD, right hepatic duct, left hepatic duct or common hepatic duct and (3) trabecular type, in which one cystic duct enters the CBD while the other directly enters the liver parenchyma [5]. According to these classifications, the case described would represent a type 2 H type double gallbladder [2,5].
According to G. Desolneux et al duplication should be considered when two cystic ducts are present on preoperative imaging [7]. Such anomaly may predispose to the development of gall stones due to impaired emptying of the gallbladder [4].
Duplication of the gall bladder may be associated with duplication of cystic duct, the anatomy should be precisely visualized during surgery to avoid injuries to other structures [4]. However, if one or both gallbladders cause symptoms, cholecystectomy should be done for both gallbladders [8].
The duplicated gall bladder may remain undiagnosed preoperatively and present as single gall bladder on laparoscopy [9,10]. That is the reason most cases of duplicated gall bladder are converted to open surgery due to lack of awareness about this variant [9].
Important points for safe cholecystectomy worth mentioning here -
PREOPERATIVE WORKUP
- Preoperative workup of gall bladder stone surgery should always include LFT & USG .In case of raised ALP, MRCP should be done which can delineate biliary anatomy, CBD stone or obstructing lesion. MRCP findings should be discussed with radiologist.
- Routine ERCP is not preferred for preoperative wore up for cholecystectomy unless it’s being done for therapeutic purpose.
- Always counsel patient about the anatomical variation which may need open conversion stating % rate at your centre so that in case of need surgeon doesn't feel the pressure of resisting open conversion of a difficult laparoscopic case.
INTRAOPERATIVE TIPS
- As soon as scope is inserted one should reconfirm preoperative findings of double gall bladder.
- Gall bladder rotation is difficult so posterior dissection cannot be done in first step, one should dissect calots from below or front and delineate single/double cystic duct according to MRCP findings (Figures 3,4).
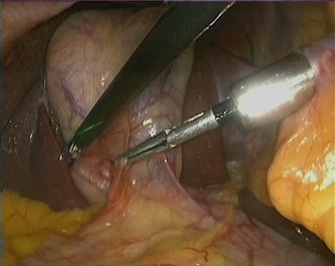 Figure 3: Intraoperative picture showing accessory gall bladders.
Figure 3: Intraoperative picture showing accessory gall bladders.
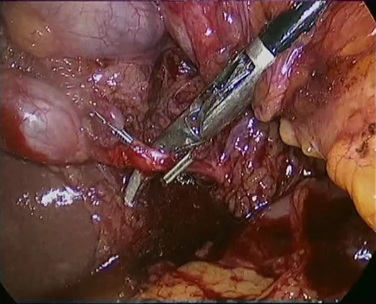 Figure 4: Intraoperative picture showing laparoscopic removal of first gall bladder and cystic duct.
Figure 4: Intraoperative picture showing laparoscopic removal of first gall bladder and cystic duct.
3. There may be separate vessels to both gall bladders which should be patiently dissected and clipped taking care not to take any big looking vessel.
4. Any of the cystic ducts (if separate), or common cystic duct may look wide and confuse the anatomy so one should reconfirm the cystic anatomy by transcystic cholangiogram. Never hesitate in open conversion.
5. The limited success of preoperative biliary tract imaging in demonstrating anatomic aberrancies prior to cholecystectomy clearly highlights the importance of maintaining constant vigilance for even the slightest anatomic abnormality at operation. Any uncertainty or concern for ductal injury mandates immediate operative cholangiogram with cannulation of all structures in question [6].
CONCLUSION
It is important for surgeons to be aware of this entity, so as to avoid leaving one or another part of gall bladder when it’s diagnosed incidentally. It is essential to delineate biliary system anomalies either pre or postoperatively so as to avoid postoperative complications and medicolegal suits in cases of insufficient surgery.
REFERENCES
- Kumar J, Yadav A (2017) Duplex gall bladder: bystander or culprit. BMJ Case Rep 221716.
- Hassan S, Young AL, Farooq M, Pai D, Gough M (2012) Accessory gallbladder: a new anatomical variation arising from both left and right hepatic ducts. Ann R Coll Surg Engl 94: e204-e205.
- Boyden EA (1926) The accessory gall-bladder. Am J Anat 38.
- Hassan Arif S, Hussein IS, Mohammed AA (2019) Duplicated gall bladder with gall bladder polyp presenting with cholecystitis: Case report with literature. Int J Surg Case Rep 60: 103-105.
- Munie S, Nasser H, Go PH, Rosso K, Woodward A (2019) Case report of a duplicated cystic duct: A unique challenge for the laparoscopic surgeon. Int J Surg Case Rep 56: 78-81.
- Muhd Yusairi K, Vasu Pillai L, Voon ML, Manisekar KS (2018) Surgical challenges of duplicated gallbladder during cholecystectomy. Med J Malaysia 73: 418-419.
- Desolneux G, Mucci S, Lebigot J, Arnaud JP, Hamy A (2009) Duplication of the Gallbladder. A Case Report. Gastroenterol Res Pract 2009: 1-3.
- Shiba H, Misawa T, Ito R, Ohki K, Igarashi T, et al. (2014) Duplicated Gall bladder. Int Surg 99: 77-78.
- Cozacov Y, Subhas G, Jacobs M, Parikh J (2015) Total laparoscopic removal of accessory gallbladder: A case report and review of literature. World J Gastrointest Surg 7: 398-402.
- Rajapandian S, Jankar SV, Nayak DS, Chittawadgi B, Sabnis SC, et al. (2017) Laparoscopic management of ‘Y?shaped’ gallbladder duplication with review of literature. J Min Access Surg 13: 231-233.
Citation: Gupta M, Goyal S (2020) Laparoscopic Management of Assessory Gall Bladder & Tips for Surgeons. J Gastroenterol Hepatology Res 5: 026.
Copyright: © 2020 Dr. Monika Gupta, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

