
Laparoscopic Sleeve Gastrectomy and Situs Inversus Totalis: Case Report and Literature Review
*Corresponding Author(s):
Fredy Romaña MosqueraResident Of General Surgery, Faculty Of Medicine, Department Of General Surgery, Cartagena University, Bolívar, Colombia
Tel:+57 3128794062,
Email:fredy.romamos@hotmail.com
Abstract
Situs Inversus Totalis (SIT) is a relatively uncommon condition, with anatomic anomaly in which an abdominal and/or thoracic organ is placed into a position similar to “a mirror reflection” in comparison to the normal position of the human organs seen from a sagittal plane. Obesity is a prevalent clinical disorder in the general population with increased risk for other diseases. Nowadays bariatric surgery has become an option for morbid obesity with great outcome. There are few report of bariatric surgery in patient with situs inversus,we present a case of a male 47 years old patient suffering from high blood pleasure, type 2 diabetes mellitus, obstructive sleep apnea, chronic sinusitis, osteoarthosis, his weight previous surgery was 121 kg and BMI: 40.9 kg/m2, his HbA1C was 8.6%, he was elected to have Laparoscopic sleeve gastrectomy and was discharge at day 2 after surgery and at 4th month follow up his BMI was 29, 7kg/m2 he has no taken any medication. As it shown in this case bariatric surgery is safely perform in situs inversus by an experienced surgeon team.
Keywords
Bariatric surgery; Laparoscopic sleeve gastrectomy ; Obesity; Situs inversus totalis
INTRODUCTION
Situs Inversus Totalis (SIT) is a recessive congenital autosomic anatomic anomaly in which an abdominal and/or thoracic organ is placed into a position similar to “a mirror reflection” in comparison to the normal position of the human organs seen from a sagittal plane. Fabricius was who firstly reported a SIT case in humans since them there are few cases reported. SIT is a relatively uncommon condition, it’s been said to be found approximately in 1 out of 5000 - 20000 individuals [1].
Obesity is a current highly prevalent clinical condition which is associated to several comorbidities such as diabetes mellitus, high blood pressure, ostheoarticular alterations, coronary heart disease, cerebrovascular disease, and so forth [2]. Thus, correcting obesity is a key point towards improving patient’s health. Bariatric surgery is nowadays the most effective intervention within the weight control field; plus, its outcomes are helpful when it comes to managing obesity-related diseases. In regards of bariatric surgery, the laparoscopic approach has been proved as the ideal one [3]. However, such approach have additional technical difficulties for the laparoscopic surgeon due to SIT’s. Based on the lack of worldwide reports of laparoscopically-approached weight control surgeries in SIT-presenting patients we are glad to provide a successfully performed laparoscopic gastric Sleeve procedure case.
CASE PRESENTATION
A male 47 years old patient suffering from high blood pleasure, type 2 diabetes mellitus, obstructive sleep apnea, chronic sinusitis, osteoarthosis, morbid obesity, and situs inversus totalis who was being treated by the internal medicine, endocrinological and nutritional services and who had been prescribed orlistat, glargine insulin, glulysine, fluoxetine, mometasonefuroate nasal spray, and gemfibrozil. This patient was also being treated with continuous positive airway pressure CPAP interventions and was under various nutritional and exercise schemes. Based on the patient’s poor response to such management, it was suggested that a bariatric surgery be performed to him. This patient was received to our bariatric surgery services with the following anthropometric data: height: 1.75m; weight: 121 kg; BMI: 40.9 kg/m2; HbA1C: 8.6%. The patient was also performed routine tests and some specialized tests whose results were: echocardiogram showing a conserved biventricular function and showing the presence of situs inversus; thoracic X-rays: cardiac silhouette located towards the right side; upper digestive endoscopy: no alteration found besides the presence of situs inversus; nasosinuscopy: chronic rinosinutisis associated to nasal polyps, left septal deviation and left nasal turbinate hypertrophy. (Figure 1)
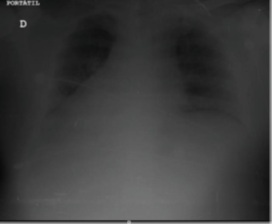 Figure 1: The apex of the heart on the patient’s right side shown in chest X-ray.
Figure 1: The apex of the heart on the patient’s right side shown in chest X-ray.
The patient was taken into the Operating Room (OR) on June 4th, 2019. The patient was operated under general anesthesia. The operating team placed into American position was composed of the head surgeon to the right, the second-in-charge surgeon to the right, the assistant surgeon and the surgical instrumental to the left. Local anesthesic was administrated through infiltration prior to the skin incision’s being made. (Figure 2)
 Figure 2:2Port Set Up.
Figure 2:2Port Set Up.
A 15mm optical trocar was introduced into the epigastrium to the right side of the medial line. A pneumoperitoneum was created and a set 30mm lenses was introduced. Under direct vision, a 15mm optical trocar was introduced into the mesogastrium, then back to the epigastrium, but closer to the left side of the medial line this time, and finally reaching the right flank. At this point, a 5mm subxyphoideal trocar was introduced and the exploration process was performed, this allowed the confirmation of the presence of SIT. The spleen was located into the right hypocondriac region, and so were the gastric fundus and its major curve under the II and III hepatic segments, located to the right of the falciform ligament. Towards the left side, into the hypochondriac region the gallbladder was found under the IV and V hepatic segments. It was also found a great hiatal hernia which contained the gastric fundus and epiplon. The patient’s stomach was noticed to be of great size and with a major curve pointing towards the right whereas the lesser curves pointed towards the left. The hiatal hernia got reduced. Gastrocolic ligament and short gastric vessel were dissected with a 37/5mm cm Maryland Jaw Laparoscopic device. A bougie was inserted to confirm a satisfactory gastric remnant size. Then methylene blue test was done without any sign of leak. (Figure 3 and Figure 4)
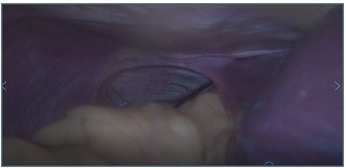 Figure 3: 3D Lafragmatic hernia at the left and the liver at the right side.
Figure 3: 3D Lafragmatic hernia at the left and the liver at the right side.
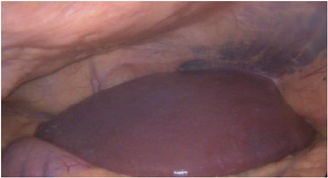 Figure 4: Liver at the right position.
Figure 4: Liver at the right position.
The patient was allowed to use his oral administration route the first postoperative day, and was given medical discharge on the second postoperative day. On the fifth postoperative day, the patient was taken back into the hospital due to upper gastrointestinal bleeding, he did not need blood transfusion either additional procedure. A month later after the procedure, the patient was seen as part of the postoperative routine appointments and his fasting glycemic levels were 110 mg/dl and his blood glucose levels after a glucose load test were 125 mg/dl. His HbA1C levels were of 6,18% without medication. His body weight was of 88 Kg and his Body Mass Index (BMI) was 29, 7kg/m2.
METHODS
PubMed, ResearchGate, and Google Scholar search revealed a total of 27 papers with 30 cases of bariatric surgeries performed on patients with Situs Inversus between 1998 and 2019. Using the following search terms: “obesity”, “morbid obesity”, “bariatric surgery” “obesity surgery” “situs inversus” “situs inversus totalis’. The following information was collected: first author of article; publication year; patient’s gender, BMI age and preoperative study, surgical technique and complications.
RESULTS
We Found 27 case reports with 30 patient who were into bariatric surgery, 18 (60%) patient were female, 8 (26.7%) were male, in 4 of them the author did not give any demographic information. The average age was 29 year, the younger patient was 19 year [4] and the older 59 year [5]. The average BMI was 44.72kg/m2, BMI range was between 76 kg/m2 and 35 kg/m2. There were 2 patients with Kartagenere Syndrome previously diagnostic [6,7]. Pauli et al, refer this imply an additional anesthetic risk and they managed with low neumoperitoneum pressure. The second patient did not show any inconvenient.
The average operating time was 112.83 min. The French position was performed in 9 (30%) patient and the mirror position in 15 (50%) patient, in 6cases the author did not give this information.
LRYGB: laparoscopic roux-y-gastric bypass was performed in 10 patients [4,5,7,8-13], LAGB: laparoscopic adjustable gastric banding in 5 patients [6,14-17], LSG: laparoscopic sleeve gastrectomy in 9patients [12,18-25]. SILSG: single incision laparoscopic sleeve gastrectomy in 1 patient [26]. LSG+DS: laparoscopic sleeve gastrectomy duodenal switch in 1 patient [27], SIPS: stomach intestine pylorus sparing surgery in 1 patient [28], RRYGB: robotic assisted roux-Y-gastric bypass in 1 Patient [20]. LOAGB: Laparoscopic One-Anastomosis Gastric Bypass in 2 patient [3,29].
Complications were reported in 3 patients. One patient with band erosion [6] and the other one with suture line leakage [19], the authors did not related it with the anatomy changes seen in situs inversus. In the last complication the author has to converse for technical difficulties as a result of anatomical changes noticed intraoperative [13]. (Table 1)
|
|
Age |
Gender |
Body mass index (BMI) before operation (kg/m2) |
Preoperative diagnostic Method |
The need for additional trocars |
Operation time |
Kartagner syndrome |
Surgical procedure |
Postoperative complications |
Position |
|
Wittgrove et al. (1998) |
38 |
female |
47.8 |
ECG/X- raychest |
No |
300 min |
No |
LRYGB |
No |
Mirror position |
|
Ersoy et al. (2005) |
33 |
female |
53 |
ECG/gastroscopy/ X-ray chest/USG |
No |
NA |
No |
LAGB |
No |
French position |
|
Catheline et al. (2006) |
19 |
male |
76 |
ECG/gastroscopy/ X-ray chest/USG |
Yes |
NA |
No |
LSG |
No |
French position |
|
Ahmed et al. (2006) |
47 |
female |
58.1 |
ECG/X- ray chest/CT scan |
No |
160 min |
No |
LRYGB |
No |
Mirror position |
|
Samaan et al. (2008) |
29 |
male |
56 |
ECG |
No |
NA |
No |
LAGB |
Band erosion |
French position |
|
Matar (2008) |
28 |
male |
51 |
ECG/Barium graphy/X-ray chest/USG |
No |
NA |
No |
LAGB |
No |
NA |
|
Pauli et al. (2008) |
47 |
female |
60 |
X-ray chest/chest and abdominal CT scan |
Yes |
105 min |
Yes |
LAGB |
No |
Mirror position |
|
Taskin et al. (2008) |
20 |
female |
44.9 |
ECG/X-ray chest/USG |
Yes |
90 min |
No |
LAGB + LC |
No |
Mirror position |
|
Barros et al. (2010) |
24 |
male |
40 |
Bariumgraphy/ Abdominal CT |
NA |
400 min |
No |
LRYGB |
No |
Mirror position |
|
Deutsch et al. (2012) |
39 |
female |
42 |
Abdominal CT |
No |
NA |
No |
LSG |
Suture line leakage |
NA |
|
Wall et al. (2014) |
58 |
male |
43.4 |
Abdominal CT |
yes |
NA |
No |
RRYGB |
No |
NA |
|
Stier et al. (2014) |
51 |
female |
54.2 |
USG/X-ray chest/gastroscopy/ ECG |
No |
61 min |
No |
LSG |
No |
French position |
|
Stier et al. (2014) |
39 |
male |
44 |
USG/X-ray chest/gastroscopy/ ECG |
No |
76 min |
No |
LRYGB |
No |
French position |
|
Tsepelidis et al. (2015) |
51 |
female |
43 |
NA |
No |
120 min |
No |
LRYGB |
No |
Mirror position |
|
Nelson et al. (2015) |
43 |
female |
45.3 |
USG/X-ray chest/Gastroscopy |
No |
NA |
No |
LRYGB |
No |
NA |
|
Genser et al. (2015) |
52 |
female |
49 |
ECG/X- ray chest/CT scan |
Yes |
52 min |
Yes |
Trans-umbilical SILSG |
No |
NA |
|
Yazar et al. (2015) |
21 |
female |
41.8 |
ECG/ gastroscopy/ X-ray ch |
No |
78 min |
No |
LSG |
No |
French position |
|
Augusto et al. (2015) |
49 |
NA |
38,9 |
Abdominal CT/Gastroscopic/ Echocardiogram |
No |
160 min |
No |
LRYGB |
No |
Mirror position |
|
Augusto et al. (2015) |
39 |
NA |
35 |
Abdominal CT/Gastroscopic/ Echocardiogram |
No |
160 min |
No |
LRYGB |
No |
Mirror position |
|
Augusto et al. (2015) |
49 |
NA |
39.2 |
Unknown |
No |
160 min |
No |
LRYGB |
Conversion |
Mirror position |
|
Watanabe et al. (2016) |
46 |
female |
40,3 |
ECG/Abdominal CT |
Yes |
202 |
No |
LSG/DS |
No |
Mirror position |
|
Surve et al. (2017) |
31 |
female |
52,5 |
NA |
No |
90 min |
No |
SIPS |
No |
Mirror position |
|
Aziret et al. (2017) |
54 |
female |
54 |
NA |
No |
105 min |
No |
LSG |
No |
French position |
|
Kassir et al. (2017) |
NA |
NA |
NA |
abdominal CT/Gastroscopic |
No |
50 min |
No |
LOAGB |
No |
French position |
|
Salerno et al. (2017) |
41 |
male |
46.4 |
NA |
No |
45 min |
No |
LSG |
No |
French position |
|
Atwez et al. (2018) |
43 |
female |
50 |
X-RAY CHEST/ECG/ ABDOMINAL CT |
No |
180 min |
No |
LRYGB |
No |
Mirror position |
|
Froylich et al. (2018) |
47 |
female |
51 |
x-RAY CHEST/Gastroscopic |
No |
62 min |
No |
LSG |
No |
NA |
|
Villalvazo et al. (2019) |
59 |
female |
38 |
ECG/Gastroscopic/ abcominalct/Xray |
No |
108 min |
No |
LSG |
No |
Mirror position |
|
Amini et al. (2018) |
36 |
male |
56.8 |
ECG/CHEST X-ray/abdominal US |
No |
90 min |
No |
LOAGB |
No |
Mirror position |
|
Burvil et al. (2019) |
25 |
female |
40 |
NA |
Yes |
35 min |
No |
LSG |
No |
Mirror position |
|
LRYGB: laparoscopic roux-y-gastric bypass, LAGB: laparoscopic adjustable gastric banding, LSG: laparoscopic sleeve gastrectomy, SILSG: single incision laparoscopic sleeve gastrectomy, LSG + DS: laparoscopic sleeve gastrectomy duodenal switch, SIPS: stomach intestine pylorus sparing surgery, RRYGB: robotic assisted roux-Y-gastric bypass. LOAGB: Laparoscopic One-Anastomosis Gastric Bypass. |
||||||||||
Table 1: Bariatric surgery In situs inversus: Literature review.
CONCLUSION
Situs inversus related with obesity is a rare condition, those patient have a similar high cardiovascular risk compared to the general population. Patient with situs inversus can have bariatric surgery safely but is very important to have the routine preoperative protocol to patient with obesity (EKG, Chest X-ray, abdominal Ultrasound, gastroscopy and abdominal CT if it needed). Most surgeons reported technical aspect as the hardest part because the mirror images in situs inversus and the need to use the right hand. Finally we think bariatric surgery is an option in patient with situs inversus and obesity.
In order to performance safely this procedure in patient with situs inversus the mirror image approach has demonstrated to be effective. As Wall et al. described Robotic surgery is an option to avoid the need to change position or instrument orientation by the surgeon, which have been reported in the literature as a principal technical problem.
REFERENCES
- Nursal TZ, Baykal A, Iret D, Aran O (2001) Laparoscopic cholecystectomy in a patient with situs inversus totalis. J Laparoendosc Adv Surg Tech A 11: 239-241.
- Maggard MA, Shugarman LR, Suttorp M, Maglione M, Sugerman HJ, et al. (2005) Meta-Analysis: Surgical Treatment of Obesity. Annals of Internal Medicine 142: 547-559.
- Kassir R, Mourthadhoi F, Tiffet O, Lointier P (2017) How do I do a laparoscopic one-anastomosis gastric bypass in a patient with situs inversus totalis. Obes Surg 27: 2218-2219.
- Wittgrove AC, Clark GW (1998) Laparoscopic gastric bypass for morbid obesity in a patient with situs inversus. J Laparoendosc Adv Surg Tech A 8: 53-55.
- Atwez A, Keilani Z (2018) Laparoscopic Roux-en-Y gastric bypass in a patient with situs inversus totalis: Case report, technical tips and review of the literature. Int J Surg Case Rep 45: 56-62.
- Samaan M, Ratnasingham A, Pittathankal A, Hashemi M (2008) Laparoscopic adjustable gastric banding for morbid obesity in a patient with situs inversus totalis. Obes Surg 18: 898-901.
- Tsepelidis D, Loi P, Katsanos G, Closset J (2015) Gastric Bypass for Morbid Obesity in a Patient with Situs Inversus Totalis. Acta Chirurgica Belgica 115: 81-82.
- Ahmed AR, Malley WO (2006) Laparoscopic Roux-en-Y gastric bypass in a patient with situs inversus. Obes Surg 16: 1392-1394.
- de Barros CJ, Rapoport A, de Andrade Sobrinho J, Dedivitis RA, Grill EH (2010) The gastric bypass banding for morbid obesity in a patient with situs inversus. Rev Col Bras Cir 37: 157-158.
- Stier C, El-Sayes I, Theodoridou S (2014) Are laparoscopic bariatric procedures feasible in morbidly obese patients with situs inversus? A report of 2 cases and a brief review. Surg Obes Relat Dis 6: e53-e56.
- Nelson L, Teixeira AF, Jawad MA (2016) Laparoscopic Roux-en-Y gastric bypass in a patient with situs inversus. Surg Obes Relat Dis 12: 711-713.
- Yazar FM, Emre A, Akbulut S, Urfal?o?lu A, Cengiz E, et al. (2016) Laparoscopic sleeve gastrectomy in situs inversus totalis: a case report and comprehensive literature review. Indian J Surg 78: 130-135.
- Tinoco A, Bussad A, Tinoco R, Luciana ElK (2015) Situs Inversus during Bariatric Surgery: A Retrospective Analyze. Surgical Science 6: 454-458.
- Ersoy E, Koksal H, Ege B (2005) Laparoscopic gastric banding for morbid obesity in a patient with situs inversus totalis. Obes Surg 15: 1344-1346.
- Matar ZS (2008) Laparoscopic adjustable gastric banding in a morbidly obese patient with situs inversus totalis. Obes Surg 18: 1632-1635.
- Pauli EM, Wadiwala II, Rogers AM (2008) Laparoscopic placement of an adjustable gastric band in a super–super obese patient with situs inversus. Surg Obes Relat Dis 4: 768-769.
- Taskin M, Zengin K, Ozben V (2009) Concomitant laparoscopic adjustable gastric banding and laparoscopic cholecystectomy in a super-obese patient with situs inversus totalis who previously underwent intragastric balloon placement. Obes Surg 19: 1724-1726.
- Catheline JM, Rosales C, Cohen R, Bihan H, Fournier JL, et al. (2006) Laparoscopic sleeve gastrectomy for a super-super-obese patient with situs inversus totalis. Obes Surg 16: 1092-1095.
- Deutsch GB, Gunabushanam V, Mishra N, Sathyanarayana SA, Kamath V, et al. (2012) Laparoscopic vertical sleeve gastrectomy after open gastric banding in a patient with situs inversus totalis. J Minim Access Surg 8: 93-96.
- Wall A, Feng Z, Melvin W (2014) Robotic-assisted Roux-en-Y gastric bypass in a patient with situs inversus. J Robotic Surg 8: 169-171.
- Aziret M, Karaman K, Ercan M, Bostanc? EB, Ako?lu M (2017) Laparoscopic sleeve gastrectomy on a morbidly obese patient with situs inversus totalis: a case study and systematic review of the literature. Obes Res Clin Pract 11: 144-151.
- Salerno A, Trotta M, Sarra G, D'Alessandro G, Marinari GM (2017) Laparoscopic sleeve gastrectomy in a patient with situs viscerum inversus totalis: is the life easy upside-down? Surg Endosc 32: 516.
- Froylich D, Segal-Abramovich T, Pascal G, Hazzan D (2018) Laparoscopic Sleeve Gastrectomy in Patients with Situs Inversus. Obes Surg 28: 2987.
- Villalvazo Y, Jensen CM (2018) A Backwards Approach to Bariatric Surgery: The Perioperative Approach Used in a Woman with Situs Inversus Totalis Undergoing a Laparoscopic Sleeve Gastrectomy. Cureus 10: e3464.
- Burvill A BR, Hamdorf J (2019) Laparoscopic sleeve gastrectomy in a patient with situs inversus totalis and Kartagener syndrome: an unusual surgical conundrum. BMJ Case Rep 24 12: e229550.
- Genser L, Tayar C, Eddine IK. Trans-umbilical single ?ncision laparoscopic sleeve gastrectomy in a patient with situs ?nversus totalis and kartagener syndrome: video report. Obes Surg 25: 1985-1986.
- Watanabe A, Seki Y, Kasama K (2016) Laparoscopic sleeve gastrectomy with duodeno-jejunal bypass for morbid obesity in a patient with situs inversus totalis. Asian J Endosc Surg 9: 218-221.
- Surve A, Zaveri H, Cottam D, Richards C, Medlin W, et al. (2017) Laparoscopic stomach intestinal pylorus sparing surgery in a patient with morbid obesity and situs inversus: first video case report. Surg Obes Relat Dis 13: 122-124.
- Amini M, Dehghani R, Zare A (2019) Laparoscopic One-Anastomosis Gastric Bypass in a Patient with Morbid Obesity and Situs Inversus Totalis: a Case Report. Obes Surg 29: 632-635.
Citation: Mosquera FR, Hernandez A, Salazar D, Patron LI (2020) Laparoscopic Sleeve Gastrectomy and Situs Inversus Totalis: Case Report and Literature Review. Archiv Surg S Educ 2: 007.
Copyright: © 2020 Fredy Romaña Mosquera, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

