
Learning Health System in a Senior Retirement Community: A Platform to Promote Implementation Research
*Corresponding Author(s):
Shingo FukumaHuman Health Sciences. Kyoto University Graduate School Of Medicine, Kyoto, Japan
Tel:+81 753667675,
Email:fukuma.shingo.3m@kyoto-u.ac.jp
Abstract
Introduction: In an effort to develop a Learning Health System (LHS) for a healthy ageing society, this study launched an Internet of Things (IoT) platform in a senior residential community to continuously generate behavior logs.
Methods: Considering that older adults experience difficulties in technology adaptation and declined information processing abilities, senior residents only needed to carry around a card sized beacon which was the tracking device. Participant recruitment took place in a continuing care retirement community. Individual feedback was obtained quarterly.
Results: During the first 16 months, 111 residents, aged 67 to 97 years, joined the program, and nearly 90% of them were consistently monitored in their everyday lives. Participants’ average daily walking distance was slightly less than 1 km. The average time spent socializing was between 1 to 1.5 hours per day.
Conclusion: The IoT platform offers the possibility of extending the target population and scope of data, as well as incorporating experimental study designs. It is expected that factors affecting older people’s everyday lives and their consequences on health outcomes are continuously studied, learned from and improved.
Keywords
Communication design; Healthy aging; IoT; Learning health system; Technology adaptation
INTRODUCTION
A Learning Health System (LHS) entails a cyclical process of data generation from daily practice, analysis of the data to evolve knowledge, and application of the knowledge to the practice [1,2]. The model was originally meant to improve values in healthcare through the effective implementation of research findings using electronic health records [3]; however, the concept of LHS can be expanded to other areas, such as to improve quality of life among older adults. In that sense, continuously recording older people’s daily life and combining that information with health-related data would generate knowledge about the factors determining older people’s everyday life activities and how they relate to their longitudinal health outcomes and long-term care needs. This knowledge generated by research is then expected to be put into practice at multiple levels: the whole system level (when planning public health and social care programs), team and organizational levels (when revising work/care practice), and individual user’s level (when monitoring oneself) [4].
Designing a platform for ordinary older people to input data on their everyday life is, however, challenging. Barriers include issues with data privacy and technology adaptation. Novel information technology, such as smartphone applications and wearable devices that can track independent individuals in space and time may enable the generation of such data [5]; however, adaptation to new technology is deeply affected by age-specific factors, such as cognitive aging [6]. Although technology can facilitate older people’s lives and they are increasingly incorporating it into their routines, the elderly typically experience more difficulties in learning to use and operate technology than younger adults [7]. As for overcoming the data privacy issues, voluntary consensus are preferred [8]; therefore, older people need to understand the importance of and agree to provide data using electronic devices [9].
Regarding the above-mentioned issues associated with the development of a LHS for a healthy ageing society, we aimed to launch an Internet of Things (IoT) platform to track the location of older people living independently. A Continuing Care Retirement Community (CCRC) was the selected site as it offers the potential to expand the scope of data collection beyond the behavior logs. The idea was introduced as an attractive activity program in which the CCRC residents could participate voluntarily. This short article describes its implementation over 16 months and the corresponding findings.
RESEARCH INTERESTS
The authors’ main research interest focused on whether it was possible to continuously track behavior logs of functionally independent older people using an IoT platform.
METHODS
Setting
This study took place in a CCRC built over 11 hectares on a hill in an isolated area of Kyoto, Japan. The community has a total of 361 units (335 apartment units and 26 assisted living units) and 51 nursing care units, offering 24-hour health care at an onsite clinic, security services with built-in door and room sensors, and social and recreational activities. The residents typically start their life in the CCRC in their seventies and spend 10-15 years until death. Because of its location, it is not unusual for many residents to spend their day within the area of the CCRC; thus, it is a nearly closed community where their everyday life takes place from the time of retirement all the way to the end-of-life.
Technical artifact adopted in the activity program
Given the possibility that older people would not accept technology, we adopted a beacon technology for tracking the residents. Beacons are small, wireless transmitters that use low-energy Bluetooth technology to send signals [10]. The senior residents were only asked to carry a 16 g card-sized beacon as they went around with their normal routines without requiring any extra operation. In total, 30 beacon receivers were utilized throughout the CCRC to detect information from the surrounding beacons that broadcasted packets of data at regular intervals and forward the data to the server. With this IoT system, exact times to enter and exit from a radius of 10 to 30 m from the 30 locations were accumulated in a chronological order for each resident. The locations of the receivers were carefully determined through a process of trial and error, so that the approximate distances the residents moved in and around the CCRC and the approximate time spent around the receivers for social interaction could be estimated. The distance was calculated based on latitude and longitudes where 30 beacon receivers were located using a haversine formula, a method which was validated through a study with 10 CCRC employees using pedometers at the same time (appendix).
Recruitment to the activity program
Because carrying the beacon card was completely at the discretion of residents, we intentionally recruited participants by holding a large event in September 2018 and remained open so that new residents could also participate. For the recruitment purpose, important information was conceptualized as an illustration, since visual images communicate information better than text [11,12]. The aim of the activity was showed in a circle linkage between “knowing” (one’s life), “changing” (one’s behavior to a healthier one), “feeling” (what is happening in one’s life), and “connecting” (with people), which we believed would be the learning component of LHS from the user’s point of view (Figure 1a). Additionally, an overview of the project was illustrated, emphasizing ease of use, which is a known factor to facilitate technology adaptation among seniors [13,14] (Figure 1b). To attract participants, a project logo was designed to show an image of seniors walking actively (Figure 1c) and a starter kit with the project logo, including a card holder that fit a beacon card and could be attached to their key chains as well as a binder notebook for collection of individual feedback sheets were provided. In addition, stamp spots with the project logo were situated at six sites across the CCRC to attract participants’ attention [15]. Original seasonal stamp sheets were given to each participant so that the residents could enjoy the stamp rallies at their own pace. To notify the residents that new stamps had arrived, we hanged posters on the notice boards across the CCRC in order to make the project almost always visible to all residents.
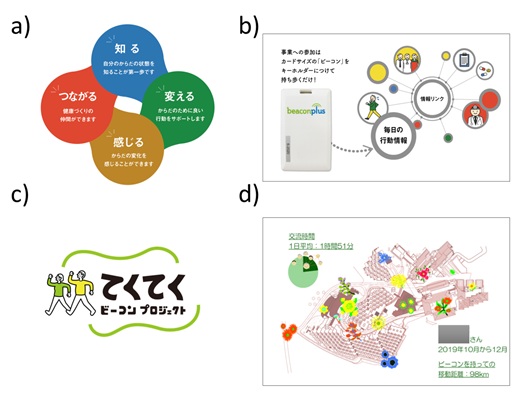 Figure 1: Examples of visual communication design used in the project.
Figure 1: Examples of visual communication design used in the project.
a)Conceptualized aims of the project: knowing (blue), changing (green), feeling (yellow), and connecting (red) are closely connected and circulating, implying a continuing improvement based on data generation
b)Illustration to show the residents what they needed to do in the project, saying “You only need to attach this card-sized beacon to your key holder”
c)Project logo, meaning tekuteku (a mimetic word of actively walking on foot) beacon project
d)A feedback sheet of 2019. Q4 of an 80-year-old female. It contains three pieces of information: total distance the person moved in and around the CCRC at the bottom right (98km), time for social interaction illustrated in the pie graph at the top left (1 hour 51 min), and flowered map to indicate the places the person visited
Individual feedback
Providing feedback helps encourage adaptation by beneficiary group [9]. The feedback form was designed to be as simple as possible to avoid the burden of excessive information for senior adults while containing the necessary information, leading to a one-page, double-sided sheet of paper. The front page displayed three kinds of information: (1) approximate distances over three months in km, (2) approximate time spent in social interaction and (3) visited locations. The locations were shown on the CCRC map with different flower signs. The flowers had three versions varying in size or growth and plotted on the basis of the tercile in the frequency of visiting the location (Figure 1d). The back page contained a message from the research team and a scale-like map from Kyoto to Tokyo to be painted by individuals. Later, the map was changed to show Kyoto to Sapporo to establish specific, short-term goals that would challenge the participants [16]. The sheet was provided quarterly.
Evaluation
We evaluated the project implementation using two aspects. The first was the proportion of participants among all the residents who are assumed to be living independently in the CCRC. Functional independence was defined as not meeting any of the “need care” criteria in the national long-term care insurance [17] at the time of the first recruitment. The date on which participation started was ascertained by the signed informed consent forms. The second aspect was the coherence of the data generated from the beacons with other compatible data, such as an average daily distance.
Institutional review board approval
The Institutional Review Board (IRB) of Kyoto University approved the study (R1669). We obtained written informed consent from all participants to use their information. We analyzed data anonymously using research IDs (resident names were securely linked to a research ID when making the individual feedback sheets) to ensure confidentiality. This research was conducted in accordance with the principles embodied in the Declaration of Helsinki.
RESULTS
Proportion of participants among eligible residents
The program participation rate increased gradually over 16 months (Figure 2). In total, 111 residents aged 67 to 97 years (mean age = 81.1 years, SD = 7.4) participated. Among them, 70.4 % were females. The total of participants was estimated to be 34.3% of the total 327 residents who were assumed to be living independently in the CCRC.
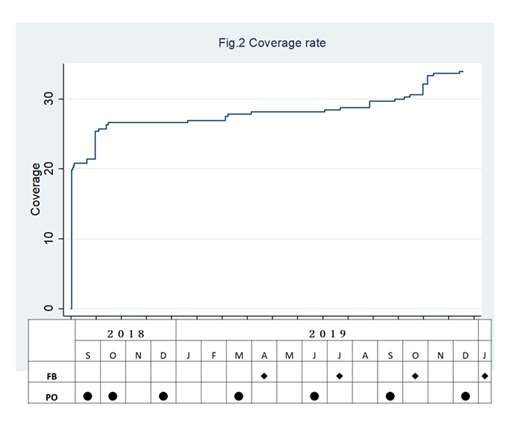 Figure 2: Coverage rate after the first recruiting event in September 2018.
Figure 2: Coverage rate after the first recruiting event in September 2018.
The top graph shows Kaplan-Meier curves for the coverage rate of residents. The censoring was ascertained by the date of submission of signed informed consent. The table below indicates the timings when individual feedback sheets were posted to individual resident (FB) and when posters about the project were posted to the notice boards across the CCRC (PO).
Summary data of individual feedback
Table 1 shows the summary data of four individual feedback sheets obtained in 2019. Nearly 90% of participants were consistently carrying the beacon card during their everyday activities. Distances captured by the beacons indicated that participants’ average daily distance was slightly less than 1 km. Considerable reduction in the covered distance was observed during the summer (Quarter 3), but not with respect to the time spent on social interaction. The average time spent socializing was between 1 to 1.5 hours per day.
|
2019 Quarter |
Residents submitted informed consent* |
Beacon carriers† |
Summary data of individual feedback |
|||
|
Total distance for the quarter in km |
Daily hours for social interaction |
|||||
|
n |
n (%) |
mean |
95% CI |
mean |
95% CI |
|
|
Q1 |
94 |
78 (83.0%) |
75.8 |
[59.9 - 91.7] |
0.97 |
[0.91 - 1.02] |
|
Q2 |
95 |
83 (87.4%) |
90.0 |
[71.3 - 108.6] |
1.29 |
[1.21 - 1.37] |
|
Q3 |
100 |
84 (84.0%) |
62.8 |
[51.3 - 74.3] |
1.24 |
[1.16 - 1.32] |
|
Q4 |
111 |
97 (87.4%) |
71.5 |
[58.5 - 84.5] |
1.24 |
[1.17 - 1.32] |
Table 1: Summary data of individual feedback in 2019.
CI: Confidence Interval, Q: Quarter, n: Number
*The number was ascertained by date of submission by the end of each period.
†Beacon carriers were determined as those whose total distance was not 0 km.
DISCUSSION
To date, real-time behavior logs from over 100 functionally independent older people are being continuously generated using the beacon technology. Participation is not mandatory, but voluntary and it covers about one-third of the residents, the largest coverage out of any project in the CCRC. However, recruiting more participants remains a challenging issue. The average daily distance of slightly less than 1 km generated from the beacon data is fairly consistent with the results of a government survey showing that the most common range of daily walking distance for senior adults in Japan was 0.5-1.0 km [18]. The significant reduction of daily distance covered by seniors during the hot summer period seems to reflect the characteristics of that population as a whole.
These behavior logs could potentially be complemented with additional information, such as medical information and staff documentation, within the CCRC to formulate the “performance to data” component of the LHS, aiming at a healthy ageing society (Figure 3). Further, as the next step, we plan to situate a beacon-linked communication device in the CCRC with a careful consideration of age-specific characteristics for technology use. By extending the target population, scope of data, and implementing an experimental study design, we expect that the factors affecting older people’s daily activities as well as their consequences on health outcomes are continuously studied, learned from, and improved.
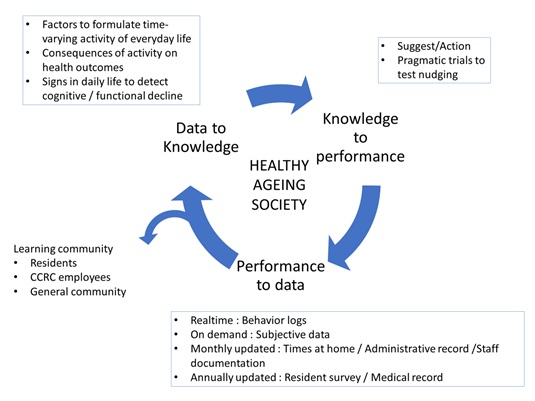 Figure 3: Goal of Learning Health System for healthy ageing society.
Figure 3: Goal of Learning Health System for healthy ageing society.
A Learning Health System (LHS) entails a cyclical process of data generation from daily practice, analysis of the data to evolve knowledge, and application of the knowledge to practice. The inside of the box contains particular components in this study.
ACKNOWLEDGEMENT
We would like to thank all the staff and residents in Kyoto Yuyunosato for their immeasurable cooperation.
FUNDING
This work was supported by the Japan Society for the Promotion of Science KAKENHIs (Grant: 17KT0041 and 19H03959). The funding sources had no other involvement in conducting the study.
DECLARATION OF COMPETING INTERESTS
None declared.
REFERENCES
- Institute of Medicine, Roundtable on Evidence-Based Medicine (2007) The National Academies Collection: Reports funded by National Institutes of Health. In: McGinnis JM, Aisner D, Olsen LA (eds.). The Learning Healthcare System: Workshop Summary. National Academies Press, Washington, D.C., USA. Pg no: 374.
- Wouters RHP, van der Graaf R, Voest EE, Bredenoord AL (2020) Learning health care systems: Highly needed but challenging. Learning Health Systems: 10211.
- Menear M, Blanchette M-A, Demers-Payette O, Roy D (2019) A framework for value-creating learning health systems. Health Research Policy and Systems 17.
- McLachlan S, Dube K, Johnson O, Buchanan D, Potts HWW, et al. (2019) A framework for analysing learning health systems: Are we removing the most impactful barriers? Learning Health Systems 3: 10189.
- Aiello AE (2017) Invited Commentary: Evolution of Social Networks, Health, and the Role of Epidemiology. Am J Epidemiol 185: 1089-1092.
- Chan AHS, Chen K (2011) A review of technology acceptance by older adults. Gerontechnology 10: 1-12.
- Álvarez-García J, Durán-Sánchez A, de la Cruz del Río-Rama M, Correa-Quezada R (2019) Older Adults and Digital Society: Scientific Coverage. Int J Environ Res Public Health 16: 2010.
- OECD (2013) Strengthening Health Information Infrastructure for Health Care Quality Governance: Good Practices, New Opportunities and Data Privacy Protection Challenges. OECD Publishing, Japan.
- Peters DH, Adam T, Alonge O, Agyepong IA, Tran N (2013) Implementation Research: What It Is and How to Do It. BMJ 347: 6753.
- Wu H-T, Tsai C-W (2018) A home security system for seniors based on the beacon technology. Concurrency and Computation: Practice and Experience 30: 4496.
- Ally BA, Waring JD, Beth EH, McKeever JD, Milberg WP, et al. (2008) Aging memory for pictures: Using high-density event-related potentials to understand the effect of aging on the picture superiority effect. Neuropsychologia 46: 679-689.
- Baadte C, Meinhardt-Injac B (2019) The Picture Superiority Effect in Associative Memory: A Developmental Study. Br J Dev Psychol 37: 382-395.
- Conci, M., Pianesi, F., & Zancanaro, M. (2009) Useful, Social and Enjoyable: Mobile Phone Adoption by Older People. Human-Computer Interaction: 63-76.
- Mitzner TL, Boron JB, Fausset CB, Adams AE, Charness N, et al. (2010) Older Adults Talk Technology: Technology Usage and Attitudes. Comput Human Behav 26: 1710-1721.
- McIntosh WD, Schmeichel B (2004) Collectors and Collecting: A Social Psychological Perspective. Leisure Sciences 26: 85-97.
- Haesner M, O’Sullivan JL, Gövercin M, Steinhagen-Thiessen E (2015) Requirements of Older Adults for a Daily Use of an Internet-Based Cognitive Training Platform. Inform Health Soc Care 40: 139-153.
- Ikegami N (2019) Financing Long-term Care: Lessons From Japan. Int J Health Policy Manag 8: 462-466.
- ESRI (2009) Economic and Social Research Institute on Town Planning for Walking. ESRI, California, USA.
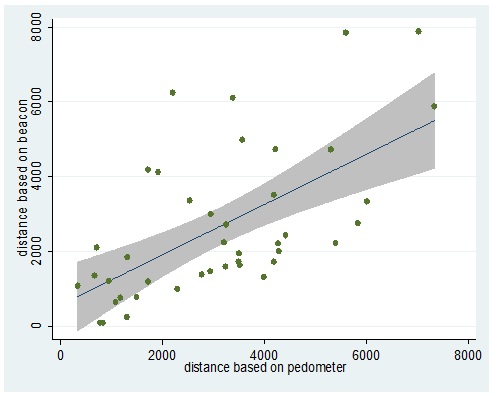
Appendix: Validation study of distance calculation based on beacon
The study was conducted with 10 CCRC employees. Each had a beacon card attached with pedometer on the day of working in the CCRC, regardless of shift for 4-5 days in June 2019. The beacon-based distance was estimated in the same way as the main study. The pedometer-based distance was estimated by an estimated stride calculated by the height (cm), multiplied by 0.45 (m). The regression equation showed a high correlation between the distances, although the pedometer-based distances are generally larger than the beacon-based distance.
Appendix figure: Scatter with regression line and 95% confidence intervals
Citation: Yamada Y, Uchida T, Shiose T, Ikenoue T, Kusunoki M, et al. (2020) Learning Health System in a Senior Retirement Community: A Platform to Promote Implementation Research. J Gerontol Geriatr Med 6: 060.
Copyright: © 2020 Yukari Yamada, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

