
Left Sided Pacemaker Implantation in a Left Persistent Superior Vena Cava -A Challenging Approach
*Corresponding Author(s):
Sara BorgesDepartment Of Cardiology, Centro Hospitalar De Tras Os Montes E Alto Douro, Vila Real, Portugal
Email:saracs.borges@gmail.com
Abstract
Congenital thoracic anomalies are being recognized increasingly given thewidespread use of advanced cardiac imaging, accompanied by a substantial growth in the number of cardiac invasive procedures in the last years; We describe a rare case of successful left-sided permanent pacemaker implantation in a patient a challenging anatomy due to Persistency of Superior Vena Cava (PLSVC) with continuation into the hemiazygos-azygos vein system.
Keywords
Accessory hemiazygos; Congenital vascular anomaly; Persistent left superior vena cava
Introduction
Congenital anomalies of the great thoracic veins are infrequent. While they are usually hemodynamically silent when not accompanied by other cardiac defects, they might pose significant challenges during vascular interventional procedures.
Persistent Left Superior Vena Cava (PLSVC) is the most common thoracic venous anomaly, accounting for ~0.5% in the general population and in up to 10% in patients with other congenital cardiac abnormalities [1]. It begins at the junction of the left subclavian and internal jugular veins, runs through the left side of the mediastinum adjacent to the aortic arcus. Typically, the drainage is into the right atrium via the coronary sinus, whose dilatation may be the first red flag to this anomaly [2].
The presence of PLSVC can make access to the right side of heart via left subclavian approach demanding, and complications have been widely reported during device implantation.
Case Report
A 90-year-old woman with hypertension and diabetes mellitus presented to the emergency department after a syncopal event. At admission, electrocardiogram revealed third-degree AV block with ventricular escape rhythm of 40 bpm; Common causes of reversible AV block were excluded, and the patient was admitted for permanent dual-chamber pacemaker implantation.
Venous access was obtained by uneventful left subclavian puncture, but the guidewire could not be advanced into the left brachiocephalic vein. Instead of reaching its anticipated course across the mediastinal midline, itmade a sharp turn and thenmaintained a vertical downward trajectory along the left cardiac border.The successive attempts showed the same result.
On cine venography, it was seen a left subclavian draining into a PLSVC which drained into a dilated azygos system - the accessory hemiazygos vein, the azygos vein and ultimately into the superior vena cava and the right atrium (Figure 1).
The PLSVC was connected to the right superior vena cava by a narrow communicating vein/innominate (Figure 2).
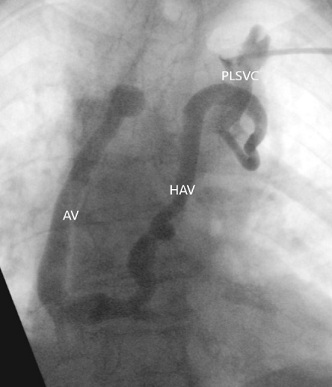 Figure 1: Venogram revealed a left subclavian vein draining into a Left Persistent Superior Vena Cava (LPSVC), accessory Hemiazygos Vein (HAV), Azygos Vein (AV) and the Superior Vena Cava (SVC).
Figure 1: Venogram revealed a left subclavian vein draining into a Left Persistent Superior Vena Cava (LPSVC), accessory Hemiazygos Vein (HAV), Azygos Vein (AV) and the Superior Vena Cava (SVC).
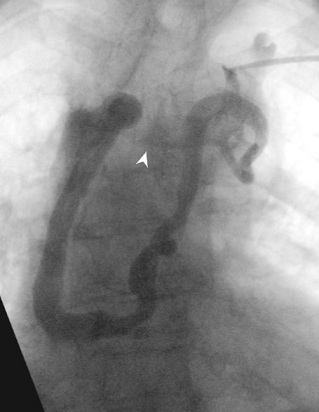 Figure 2: Venogram showing the presence of a innominate vein (arrow).
Figure 2: Venogram showing the presence of a innominate vein (arrow).
Once the anatomy was recognized, pacemaker leads were successfully implanted into the right atrium and right ventricular apex, through the inanimate vein. Both atrial and ventricular sensing and pacing parameters were adequate and a pos-procedure fluoroscopy is shown in Figure 3.
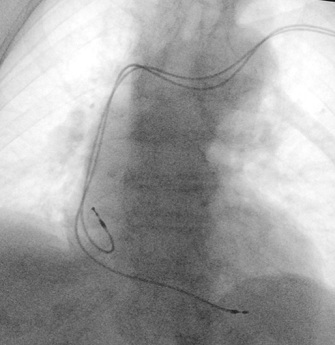 Figure 3: Post procedure lead positioning.
Figure 3: Post procedure lead positioning.
At follow up, the patient remains asymptomatic, and pacemaker is normal functioning.
Discussion
Diagnosis of PLSVC is usually made as an incidental finding during cardiovascular imaging or during procedures which require upper limb venous access.
The most common subtypes of PLSVC results in the presence of both left and right superior vena cava [3,4]. In our case, the patient a left subclavian draining into a PLSVC with an extremely atypical course into the hemiazygos-azygos vein system. Accessory hemiazygos vein is an infrequently visualized channel that normally drains the posterior intercostal veins of the left midthorax but can maintain critical venous return in case of left innominate vein stenosis.
Fortunately, our patient had an innominate vein connecting the two superior drainage systems, allowing the advancement of pacemaker leads, avoidingthe switch to a right subclavian approach.
Peripheral venography before the procedure can help to identify common venous anomalies and decrease the risk of complications, particularly in high-risk patients. Physicians performing thoracic venous procedures should be familiar with anatomic variants and with the technical alternatives to avoid complications.
Conclusion
PLSVC has diverse practical implications when the left subclavian is used to access the right side of the heart or pulmonary vasculature. Cardiac devices implantation is technically demanding but can be done safely with proper techniques.
References
- Wood P (1956) Disesase of heart and circulation. Philadelphia: JB Lippincott.
- Irwin RB, Greaves M, Schmitt M (2012) Left superior vena cava: revisited. Eur Heart J Cardiovasc Imaging 13: 284-291.
- Azizova A, Onder O, Arslan S, Ardali S, Hazirolan T (2020) Persistent left superior vena cava: clinical importance and differential diagnoses. Insights Imaging 11: 110.
- Goyal SK, Punnam SR, Verma G, Ruberg FL (2008) Persistent left superior vena cava: A case report and review of literature. Cardiovasc Ultrasound 6: 50.
Citation: Borges S, Margato R, Moreira JI (2021) Left Sided Pacemaker Implantation in A Left Persistent Superior Vena Cava -A Challenging Approach. J Angiol Vasc Surg 6: 079.
Copyright: © 2021 Sara Borges, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

