
Lessons from CL Psychiatry: Recognising Co-Existing Anti-Cholinergic Delirium in an Acute First Episode Psychosis Presentation in an Adolescent
*Corresponding Author(s):
Yiu Fung ManMental Health And Specialists Services, Gold Coast University Hospital, Australia
Email:YiuFung.Man@health.qld.gov.au
Summary
We describe the diagnostic challenges in differentiating anticholinergic delirium from first onset psychosis in an adolescent and aim to share lessons learnt.
A male adolescent patient presented with a combination of psychotic and fluctuating autonomic symptoms indicative of anticholinergic delirium at different time points.
The initial diagnosis was that of first onset psychosis, supported by a first-degree relative receiving treatment for schizophrenia. A concealed history of clozapine overdose was later disclosed, prompting re-consideration for organic causes. However, the diminishing and re-emergence of symptoms relating to delirium created a variable clinical picture as the adolescent is assessed by different specialists.
This highlights the importance for having a longitudinal approach with detailed information sharing between specialties.
Background
Delirium is a syndrome that can present with variable symptoms, including but not limiting to a global change in attention, awareness and cognition, it is caused by a medical condition that cannot be better explained by a pre-existing neurocognitive disorder.
Diagnosing delirium in children is a challenging task. Delirium is commonly seen with elderly patients but rare in children, at least 20% of the 12.5 million patients over 65 years of age hospitalized each year is thought to have experience delirium; in contrast, Paediatric delirium is mostly reported in ICU, and uncommon in other settings. Delirium presents variably and its course fluctuates [1,2]. Children’s potential limitation to communicate and express their symptoms adds to the challenge [3]. Furthermore, anticholinergic delirium is in itself rare [4] making the task of accurately diagnosing delirium ever more difficult. However, it remains important to exclude anti-cholinergic delirium, as it is associated with increased rate of mortality if the underlying cause is not treated [5,6].
Delirium is a syndrome that can present with variable symptoms, including but not limiting to a global change in attention, awareness and cognition, it is caused by a medical condition that cannot be better explained by a pre-existing neurocognitive disorder.
Diagnosing delirium in children is a challenging task. Delirium is commonly seen with elderly patients but rare in children, at least 20% of the 12.5 million patients over 65 years of age hospitalized each year is thought to have experience delirium; in contrast, Paediatric delirium is mostly reported in ICU, and uncommon in other settings. Delirium presents variably and its course fluctuates. Children’s potential limitation to communicate and express their symptoms adds to the challenge. Furthermore, anticholinergic delirium is in itself rare making the task of accurately diagnosing delirium ever more difficult. However, it remains important to exclude anti-cholinergic delirium, as it is associated with increased rate of mortality if the underlying cause is not treated.
Psychosis is an umbrella term for conditions affecting the mind and of contact with reality. It encompasses symptoms such as thought disorder, delusions, and hallucination, which confusingly can also be seen in delirium. Incidence of psychosis worldwide is estimated at 50 in 100,000 people [7]. First episode psychosis most commonly occurs between the ages of 15 to 30 years [8]. Psychosis in childhood is rare at approximately 1 in 10,000 and typically more common in boys [9].
Delirium involves global disturbance of higher cortical function; it can present with a large variety of central and peripheral symptoms resembling psychosis, such as delusions and hallucinations. It can be difficult to distinguish from other causes of psychosis, such as schizophrenia. Fould’s famously developed a diagnostic hierarchy suggesting that a primary psychiatric diagnosis cannot be made until delirium is excluded [10].
Intentional and non-intentional overdoses or poisonings cause significant morbidity and mortality. Poisoning consist of exploratory ingestions in younger children, recreational substance use or intentional ingestion in adolescents [11].
The significant association between the use of drugs with anticholinergic properties and delirium is well known [12], and is hypothesise to be caused by a cholinergic deficiency [13,14]. Newer psychotropic medications such as clozapine have anticholinergic properties, and its use is increasing in the pediatric population over the past two decades. This trend raises the risk of iatrogenic, and deliberate self-harm related anticholinergic delirium in the pediatric population.
The cause of a toxidrome is often identifiable, but a history of ingestion can often be missing or inaccurate in the paediatric population.
The term toxidrome was first coined in 1970 by Mofenson and Greensher [15]. There are 5 main types of toxidrome, anticholingergic, cholinergic, opioid, sedative-hypnotic, and sympathomimetic. Toxicity in acute overdose in newer antipsychotics such as clozapine, primarily are caused by anticholinergic toxicity and has an effect on the central nervous system (CNS) and cardiovascular system. Decreased consciousness, ranging from drowsiness, somnolence to coma, nausea, vomiting and oscillopsia are common CNS signs. The most common cardiovascular effects of this toxidrome are tachycardia and mild hypotension. ECG examination is recommended to exclude QT interval and the rare risk of Torsades de pointes [16]. Peripheral signs include dry mouth, mydriasis, flushed skin, urinary retention and tachycardia. The signs of an anti-cholinergic delirium can be summarized as ‘hot as a hare (hyperthermia), red as a beet (flushed skin), dry as a bone (dry mouth, urinary retention), blind as a bat (blurred vision, visual hallucination) and mad as a hatter (confusion) (See Figure 1).
The presentation of the delirium can differ between adult and children’s due to metabolism, brain development, and communication styles. Whilst cases in adults are reported [17], to our knowledge, this is the first report of clozapine related anticholinergic delirium in an adolescent making this a unique case.
Case Presentation
Presenting complaint
A 16 years old adolescent male without a previous mental health history, presented to the emergency department of a large, public metropolitan hospital with acute onset of visual hallucinations and paranoid delusions over a 3-day period. Parents brought him to the emergency department as he engaged in superficial self-harm, believing that there was ‘black blood in his body’ and that he transformed to a werewolf. Collateral history from parents revealed that his brother received Clozapine for treatment-resistant schizophrenia.
Management in the emergency department
At triage, he had a temperature of 38.3 °C, sinus tachycardia of 115 bpm, and a blood pressure of 94/68 mmHg. Four hours later, he had normalized vital signs, sustained blurred vision, and diplopia. Initial laboratory investigations, venous blood gases, serial ECGs and CT head scan were unremarkable. Urine drug screen was positive for cannabis.
Due to a lack of significant organic cause, and predominant symptoms of visual hallucination and delusions, he was referred to mental health services.
Psychiatric assessment
On mental state examination 6 hours after initial presentation, he appeared unkempt, with food around the mouth, and over his shirt. He was restless and was shaking uncontrollably. It was difficult to build rapport and maintain eye contact. His speech was slurred, rapid and loud. He was objectively anxious, and affect was labile and agitated. His thoughts were pressured, and incoherent. He was paranoid; he struggles to elaborate more on his thoughts. He reported vivid visual hallucinations of seeing ‘black blood’ on his skin, and he was observed picking at imaginary objects. Attention was poor, and he was disorientated with time. He had no insight.
On further questioning, patient disclosed a staggered overdose over a 5-day period of unknown quantity his brother’s clozapine medication. His intention was to ‘cleanse’ himself of the ‘black blood’. Physically, he felt cold, had a dry mouth, excessive thirst, and profound abdominal pain. He had paranoid persecutory delusions of others harming him. This additional information indicated the possibility of a clozapine induced anticholinergic delirium and a decision to further monitor the patient in ED was made.
Further monitoring in the emergency department
The patient later demonstrated progressive tachycardia between 100 to 120 bpm seen on serial ECGs within a 4-hour monitoring period. All other vital signs returned to normal. Cardiology and toxicology were both consulted, and after a safe monitoring period of 6 hours, he was cleared for psychiatric inpatient admission.
Psychiatric admission
Further physical examination 24 hours later by the junior psychiatric doctor again revealed blurred vision, but normal vital signs, and normal physical examination. Differential diagnoses are carefully considered (Table 1).
|
Differential diagnosis |
Criteria |
Signs seen |
Comments |
|
Neuroleptic malignant syndrome (NMS) |
1. Exposure to dopamine antagonist |
Y |
The most likely differential diagnosis with an established history of clozapine overdose. |
|
2. Hyperthermia |
N |
||
|
3. Rigidity |
Y |
||
|
4. Mental state alteration |
Y |
||
|
5. CK elevated |
N |
||
|
6. Sympathetic nervous system lability |
Y |
||
|
7. 25% increased heart rate |
Y |
||
|
8. 50% increased respiratory rate |
N |
||
|
First episode psychosis |
1. Thought disorder. |
Y |
History of a first-degree relative diagnosed with treatment resistant schizophrenia. |
|
2. Perceptual disturbance |
Y |
Prodromal symptoms preceding presentation. |
|
|
3. Delusions |
Y |
Symptoms and resolving with antipsychotic treatment within one month. |
|
|
Substance induced psychosis |
Urine drug screen |
Y |
Concurrent cannabis use may have caused presenting symptoms |
|
Structural brain anomaly |
1. Abnormal CT scan |
N |
CT scan was normal. There was no history of head injury. |
|
2. Abnormal MRI scan |
N/A |
||
|
CNS related infections and autoimmune diseases. |
1. Focal neurological signs |
Y |
This is the least likely differential diagnosis [18]. |
|
2. Visual difficulties |
Y |
||
|
3. Headache |
N |
||
|
4. Neck stiffness |
N |
||
|
5. Balancing difficulties |
N |
||
|
6. Fever |
Y |
||
|
7. Rash |
N |
Table 1: Differential diagnosis.
Outcome and Follow-Up
Due to a strong family history of schizophrenia and psychotic features in his presentation, the management plan was focused on the treatment of first episode psychosis.
On admission, patient received 4 hourly nursing observations and daily ECG monitoring. Physical monitoring revealed low-grade fever (38oC), blurred vision, which resolved on day 3, intermittent tachycardia (100-120bpm) on day 1 and 2, and tremors on the second night in hospital.
It was reported that the vivid visual hallucination resolved within the week. However, paranoid delusions persisted for one month. Patient had 2 weeks of psychiatric inpatient care; on discharge he was followed up by the early intervention psychosis community team. He was maintained on 1mg of risperidone and the presenting symptoms gradually resolved over 6 months.
Discussion
Diagnostic challenges did arise for this patient due to predominant features of agitation and confusion that were less typical of a Clozapine overdose where one would expect features of CNS depression, such as coma or drowsiness. Furthermore, Clozapine commonly causes sialorrhea, however in this case, xerostomia was observed. The fluctuating nature of delirium adds to the difficulty in the context of multiple speciality assessments, as each clinician only sees a snapshot of the patient's presentation. Over the course of admission, the patient did show cumulative signs of intermittent tachycardia, blurred vision, dry mouth, thirst, fever, and visual hallucinations, which fits the clinical picture of anticholinergic delirium. This highlights the importance of thorough longitudinal clinical observation with detailed communication between specialities and good note keeping ensuring a clear overview of all aspects of a case. Assessment of delirium in the paediatric population can pose additional challenges. A review on paediatric and adolescent delirium describes the difficulty in evaluating disorientation and defining impaired attention. Increased affective lability, psychomotor agitation and altered level of consciousness were more reported in younger patients [19]. Clinicians ought to be aware of the less commonly reported antimuscarinic properties of psychotropic medications used in the paediatric population such as olanzapine, quetiapine, and clozapine.
Clozapine and its metabolite N-desmthyclozapine cause stimulation (sialorrhea) and less commonly inhibition (xerostomia) of salivary flow. Individual’s sensitivity and response to antipsychotic medication depends on genetic susceptibility [20] and autonomous nervous system dysfunction [21] i.e., the balance of parasympathetic (M1 receptor) and sympathetic (M3 receptor) stimulation [22]. Hence, either over or under salivation can occur, depending on patients’ pre-disposition.
Furthermore, some studies have shown a possible additional mechanism of unconscious swallowing reflex impairment caused by clozapine. This may explain some empirical observations of patients suffering more severe symptoms of hyper salivation at night when conscious compensatory swallowing is not possible [23] (Figure 1).
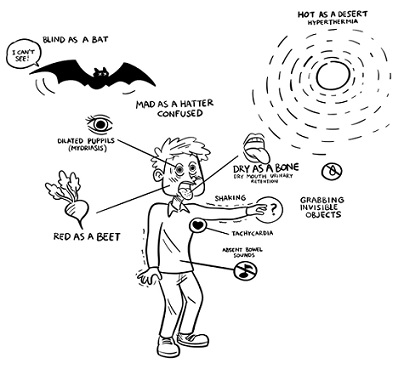 Figure 1: Cardinal signs of anti-cholinergic delirium. (Full copyright owned by Yiu Fung Man).
Figure 1: Cardinal signs of anti-cholinergic delirium. (Full copyright owned by Yiu Fung Man).
The cardinal signs of an anti-cholinergic delirium can be summarized as ‘red as a beet, blind as a bat, hot as a desert and mad as a hatter’.
Management is primarily supportive and symptomatic care. Further antipsychotic medications can worsen an anticholinergic delirium as they exacerbate anticholinergic effects. The use of benzodiazepines is preferable. Other management considerations of Clozapine could include activated charcoal, recommended within 2 hours of toxic ingestion. However, in cases with severe anticholinergic delirium, there is a risk of aspiration, and charcoal should only be used in patients with a secure airway. Physostigmine, which is an acetylcholinesterase inhibitor, can be useful as a potential treatment in an isolated anticholinergic delirium but can precipitate seizures in cases that also overdosed in Tricyclic Antidepressants.
Clozapine typically shows biphasic plasma concentration-time curves in overdose, which is relevant for drug level monitoring [24]. There is no consensus on the level indicative of toxicity, however it has been reported that the likelihood of side effects increases at a level higher than 1307mg/ml [25]. In this case, Clozapine and norclozapine serum level monitoring might be useful to support a diagnosis of anticholinergic delirium. Some studies have shown that the interplay between clozapine and its metabolite at muscarinic receptor sites could explain some of the significant interpatient variations in therapeutic response and tolerability. Considering the significant increase in clozapine: norclozapine ratio due to non-linear kinetics in an overdose scenario it is possible that the clozapine antagonistic effects on the muscarinic M1 receptor will become prevalent over the opposing norclozapine effects and increase the risk of cognitive impairment and/or anticholinergic delirium[26].
The term ‘medical clearance’ can be interpreted as having other organic illnesses being excluded rather than indicating that the patient is ‘fit for ward care’, which may preclude ongoing monitoring for physical illness and complications, such as delirium, on the psychiatric ward. It is a common feature for delirium to persist for days to weeks, in combination with its fluctuating course, making it challenging to diagnose, therefore medical and psychiatric clinicians all have responsibility to continuously assess and monitor for physical health concerns.
Scoring systems for delirium exist to aid assessment and management, such as the Cornell assessment, the preschool CAM-ICU the paediatric Confusion Assessment Method for ICU patients CAM-ICM are useful bedside delirium screening tools in critical care [27,28]. They have not been assessed or validated for use in the emergency and psychiatric departments. Future work should focus on developing a suitable age specific delirium scoring system for children in other clinical contexts other than ICU, which could improve the accuracy of delirium diagnosis and facilitate prompt and effective treatment.
Conclusion
In conclusion, psychosis in anticholinergic delirium can easily be missed. With the increased use of atypical antipsychotic medications in the paediatric population, it is important for clinicians to be aware of the distinct symptoms and course of anti-cholinergic delirium.
Learning Points/Take Home Messages 3-5 Bullet Points
- Anticholinergic delirium presents with a fluctuating course, therefore should always be considered as a differential diagnosis even with normal examination and investigations, especially during the initial week of admission. Fould’s hierarchy suggests that organic causes must first be excluded, prior to any formal psychiatric diagnosis.
- Features of vivid visual hallucinations, fluctuating level of consciousness or level of orientation to time, place, and person, and rapid onset of symptoms suggest a high probability of an organic cause, unlike psychosis related to psychiatric illness that tends to have a more gradual onset.
- The fluctuating nature of delirium highlights the importance of good inter-speciality communication and concise documentation of findings ensuring a good overview of the case.
- The use of new atypical antipsychotic medications in the paediatric population is becoming more popular and hence clinicians should be aware of the risk of associated complications such as anticholinergic delirium.
References
- Van Tuijl SG, Van Cauteren YJ, Pikhard T, Engel M, Schieveld JN (2015) Management of pediatric delirium in critical illness: a practical update. Minerva Anestesiol. 81: 333-341.
- Witlox J, Eurelings LSM, de Jonghe JFM, Kalisvaart KJ, Eikelenboom P, et al. (2010) Delirium in elderly patients and the risk of postdischarge mortality, institutionalization, and dementia: a meta-analysis. JAMA. 304: 443-451.
- Rasimas J, Liebelt EL (2012) Adverse effects and toxicity of the atypical antipsychotics: what is important for the pediatric emergency medicine practitioner? Clinical pediatric emergency medicine. 13: 300-310.
- Isbister GK, Oakley P, Dawson AH, Whyte IM (2003) Presumed Angel's trumpet (Brugmansia) poisoning: clinical effects and epidemiology. Emergency Medicine. 15: 376-382.
- Leentjens AFG, Schieveld JNM, Leonard M, Lousberg R, Verhey FRJ, et al. (2008) A comparison of the phenomenology of pediatric, adult, and geriatric delirium. J Psychosom Res. 64: 219-223.
- Smith HAB, Brink E, Fuchs DC, Ely EW, Pandharipande PP, et al. (2013) Pediatric delirium: monitoring and management in the pediatric intensive care unit. Pediatr Clin North Am. 60: 741-760.
- McGrath J, Saha S, Welham J, EL Saadi O, MacCauley C, et al. (2004) A systematic review of the incidence of schizophrenia: the distribution of rates and the influence of sex, urbanicity, migrant status and methodology. BMC medicine. 2: 1-22.
- Jones PB (2013) Adult mental health disorders and their age at onset. The British Journal of Psychiatry. 202: s5-10.
- Driver DI, Gogtay N, Rapoport JL (2013) Childhood onset schizophrenia and early onset schizophrenia spectrum disorders. Child and Adolescent Psychiatric Clinics. 22: 539-555.
- Foulds G, Bedford A (1975) Hierarchy of classes of personal illness. Psychological medicine. 5: 181-192.
- Gummin DD, Mowry JB, Beuhler MC, Spyker DA, Brooks DE, et al. (2020) 2019 annual report of the American association of poison control centers’ National Poison Data System (NPDS): 37th annual report. Clinical toxicology. 58: 1360-1541.
- Egberts A, Moreno-Gonzalez R, Alan H, Ziere G, Mattace-Raso FUS (2021) Anticholinergic Drug Burden and Delirium: A Systematic Review. J Am Med Dir Assoc. 22: 65-73.
- Hshieh TT, Fong TG, Marcantonio ER, Inouye SK (2008) Cholinergic deficiency hypothesis in delirium: a synthesis of current evidence. J Gerontol A Biol Sci Med Sci. 63: 764-772.
- Maldonado JR (2008) Pathoetiological model of delirium: a comprehensive understanding of the neurobiology of delirium and an evidence-based approach to prevention and treatment. Crit Care Clin. 24: 789-856.
- Mofenson HC, Greensher J (1970) The nontoxic ingestion. Pediatric Clinics of North America. 17: 583-590.
- Tan HH, Hoppe J, Heard K (2009) A systematic review of cardiovascular effects after atypical antipsychotic medication overdose. The American journal of emergency medicine. 27: 607-616.
- Khanra S, Sethy RR, Munda SK, Khess CRJ (2016) An Unusual Case of Delirium after Restarting Clozapine. Clin Psychopharmacol Neurosci. 14: 107-108.
- Jeppesen R, Benros ME (2019) Autoimmune Diseases and Psychotic Disorders. Frontiers in Psychiatry. 10:
- Turkel SB, Tavaré CJ (2003), Delirium in children and adolescents. The Journal of neuropsychiatry and clinical neurosciences. 15: 431-435.
- Scully CC (2003) Drug effects on salivary glands: dry mouth. Oral diseases. 9: 165-176.
- Hattori S, Suda A, Kishida I, Miyauchi M, Shiraishi Y, et al. (2018) Association between dysfunction of autonomic nervous system activity and mortality in schizophrenia. Comprehensive Psychiatry. 86: 119-122.
- Mohandoss AA, Thavarajah R (2019) Salivary Flow Alteration in Patients Undergoing Treatment for Schizophrenia: Disease-Drug-Target Gene/Protein Association Study for Side-effects. Journal of oral biology and craniofacial research. 9: 286-293.
- Rabinowitz T, Frankenburg FR, Centorrino F, Kando J (1996) The effect of clozapine on saliva flow rate: a pilot study. Biological psychiatry. 40: 1132-1134.
- Renwick AC, Renwick AG, Flanagan RJ, Ferner RE (2000) Monitoring of clozapine and norclozapine plasma concentration-time curves in acute overdose. Journal of Toxicology: Clinical Toxicology. 38: 325-328.
- Remington G, Agid O, Foussias G, Ferguson L, McDonald K, et al. (2013) Clozapine and therapeutic drug monitoring: is there sufficient evidence for an upper threshold? Psychopharmacology. 225: 505-518.
- Costa-Dookhan KA, Agarwal SM, Chintoh A, Tran VN, Stogios N, et al. (2020) The clozapine to norclozapine ratio: a narrative review of the clinical utility to minimize metabolic risk and enhance clozapine efficacy. Expert opinion on drug safety. 19: 43-57.
- Silver G, Traube C, Kearney J, Kelly D, Yoon MJ, et al. (2012) Detecting pediatric delirium: development of a rapid observational assessment tool. Intensive care medicine. 38: 1025-1031.
- Smith HAB, Boyd J, Fuchs DC, Melvin K, Berry P, et al. (2011) Diagnosing delirium in critically ill children: Validity and reliability of the Pediatric Confusion Assessment Method for the Intensive Care Unit. Critical care medicine. 39: 150.
Citation: Man YF, Wong YY, Stapelberg C, Woerwag-Mehta S (2023) Lessons from CL Psychiatry: Recognising Co-Existing Anti-Cholinergic Delirium in an Acute First Episode Psychosis Presentation in an Adolescent. J Clin Stud Med Case Rep 10:211
Copyright: © 2023 Yiu Fung Man, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

