
Living Wills and Geriatrics
*Corresponding Author(s):
Luciana Colares MaiaDiscente Da Universidade Estadual De Montes Claros/Unimontes, Centro De Ciências Biológicas E Da Saúde (CCBS), Montes Claros, MG, Brazil
Tel:+38 32248032,
Email:luciana.colares.maia@gmail.com
Abstract
Objective: Understand the application and importance of the living wills and the advance directives in geriatrics.
Method: This is an integrative literature review with descriptive and exploratory characteristics. The portal of the Virtual Health Library (VHL) was used for bibliographic research, with the inclusion of the databases Medical Literature Analysis and Retrieval System Online (MEDLINE), Índice Bibliográfico Españolem Ciencias de la Salud (IBECS) and Latin American and Caribbean Health Science Literature (LILACS). The following descriptors were used for the investigation: “advance directives”, “personal autonomy” and “aged”. Only full articles with free access to content, published between 2015 and 2020, in the languages Portuguese, Spanish and English were included. From the articles found, a table was developed for the analysis of these articles, correlating them with the proposed objectives of the study.
Results: The final sample consisted of five articles published between 2017 and 2019, with studies conducted in Brazil, Germany and Spain.
Conclusion: It was possible to observe the lack of information and knowledge about the advance directives by health professionals. This is an obstacle to ensuring autonomy and respect for end-of-life decisions of geriatric patients with terminal illness and a barrier to death with dignity.
Keywords
advance directives; Aged; Living wills; Personal autonomy
INTRODUCTION
According to 2019 data from the Pesquisa Nacionalpor Amostra de Domicílios Contínua - PNAD Contínua, the number of elderly in the Brazilian population corresponds to approximately 32 million people, representing more than 15% of the population [1]. According to IBGE projections, in 2054, about 30% of the country’s population will be over 60 years old [2]. In this context, the increase in life expectancy and population aging are accompanied by an increase in the prevalence of chronic diseases [3], many of them disabling and progressive, which can generate loss of the ability to make end-of-life decisions and be an obstacle to the patient autonomy [4], demonstrating the importance of the living wills in geriatrics.
The living wills is a document in which they are expressed in advance, while the patient is still lucid and able to exercise his autonomy and make decisions, his wishes regarding medical treatments that he may or may not be subjected to serious and irreversible illness and the inability to make decisions on his own [5]. The living wills originated in the United States in 1969. The living wills and the Durable Power of Attorney (DPOA) - appointment of a trusted person to decide on medical care and procedures when the individual is no longer able - make up the advance healthcare directives [6].
These directives become a mechanism to ensure that the final wishes of geriatric patients are met, in addition to becoming an instrument to alleviate conflicts between family members when they must decide on the health care of these patients [7]. Therefore, among other issues, the Federal Council of Medicine recognized the validity of these directives through Resolution 1.995/2012, to ensure that the wishes of patients or representatives designated by them will be respected by physicians and to establish criteria for its application [8].
According to the perspectives presented, the advance directives become an important tool of empowerment and respect for individual will at the end of life [9], and together with the living wills must be understood from the perspective of the humanization of death [10]. These instruments are, therefore, ways to guarantee the “die with dignity”, in which the patient has autonomy in the decisions of his own life [11], especially when it comes to elderly patients.
Based on the above, the present study aimed, through bibliographic review, to understand the application and importance of the living wills and the advance directives in geriatrics, especially in a context of population aging and epidemiological transition, where there is an increase in the prevalence of disabling chronic-degenerative diseases.
METHODOLOGY
This is an integral review of the literature, of a descriptive and exploratory nature, based on the development of the following steps: identification of the theme and definition of the guiding question – “how does the application of the vital will and of the early directives of will take place in geriatrics?” -; establishing the criteria for inclusion and exclusion; searches in databases; categorization of studies; evaluation; interpretation and synthesis of the knowledge obtained.
Based on the study’s guiding issue, the selection of articles was based on the parameters: analysis of early directives of will, focusing on the vital will in geriatric patients. The process for searching and selecting the articles in the databases is detailed in flowchart 1.
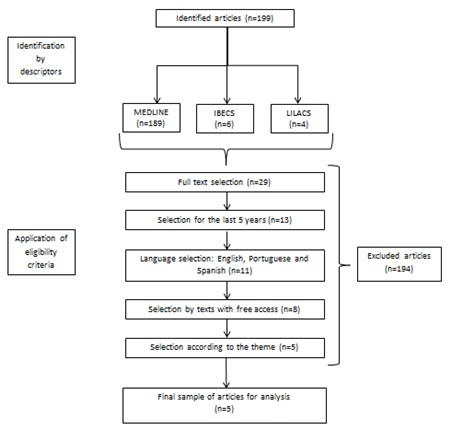 Flowchart 1: Flowchart for selecting the articles found.
Flowchart 1: Flowchart for selecting the articles found.
For the bibliographical investigation, the Virtual Library on Health (BVS) portal was used, with the inclusion of the Medical Literature Analysis and Retrieval System Online (MEDLINE) databases, the Spanish Bibliographical Index in Salud Sciences (IBECS) and the Latin American and Caribbean Literature in Health Sciences (LILACS).
The Descriptors in Health Sciences selected for the research were: “early directives”, “personal autonomy” and “old age”. The cross-check between the descriptors was carried out using the boolean and operator. The elected inclusion criteria involve the availability of complete texts with free access to content covering the proposed theme, published between 2015 and 2020, in Portuguese, Spanish and English. After the application of the criteria, the final sample consisted of six articles and was read and analyzed in full.
For the organization of the information contained in each study, a table has been drawn up containing: title, periodical and year of publication, type of study, objectives and main results obtained (Table 1). The data found were analyzed and correlated with the objectives of this work.
RESULTS
The final sample was made up of five articles, with studies conducted in Brazil, Germany and Spain, with a predominance of the first two countries. The year of publication was between 2017 and 2019. The quality of the production in each periodical varied, according to Qualis Periodicals, between B2 and A2. Transversal studies constituted those with the greatest representativeness in the final sample.
|
|
Title |
Periodical, Qualis Periodicals, year, country and data base |
Contributions |
|
1 |
Nurses defending the autonomy of the elderly at the end of life [12] |
Revista Brasileira de Enfermagem, A2, 2019, Brazil, LILACS. |
In a research conducted with nurses, doctors and nursing technicians, it was concluded that the study participants exercise actions to defend the right of autonomy of the elderly, listening to their decisions and acting together with the family. |
|
2 |
Advance directives in geriatric medicine [5] |
Revista Bioética, B2, 2018, Brazil, LILACS. |
In the study, the knowledge of medical students, teachers and caregivers of the elderly in a geriatric office about the advance directives was evaluated. Only 20% know or have any idea what these directives are. Regarding the terminally ill elderly, 56% reported trusting their medical team to respect their decisions and 83% trust their family. |
|
3 |
Declaration of living wills, a vital testament for ensuring personal self-reliance [4] |
Gerokomos, B2, 2019, Spain, IBECS. |
In a descriptive observational cross-sectional study carried out with 1652 people between 18 and 79 years old distributed throughout the Spanish territory, just over 50% of the interviewees said they knew what the advance directives would be. Part of the participants reported that it was too early to decide on the realization of these documents, understanding that the loss of decision-making capacity occurs only at older ages. |
|
4 |
Advance directives and power of attorney for health care in the oldest-old - results of the AgeQualiDe study [13] |
BCM Geriatrics, B1, 2017, Germany, MEDLINE. |
The data were taken from the German study called AgeQualiDe, carried out with elderly patients over 85 years old, whether from the community or institutionalized. Of the patients considered not to have dementia (n = 704), 69% said they had documented an advance directive for health care. Those participants who did not have it, justified their failure to do so by relying on family members and doctors to make decisions when necessary. |
|
5 |
Critical appraisal of advance directives given by patients with fatal acute stroke: an observational cohort study [14] |
BCM Medical Ethics, B2, 2017, Germany, MEDLINE. |
Study in a retrospective observational cohort, carried out with patients who died due to stroke in a German health unit. The mean age of the patients was 83.3 ± 8.5 at the time of death. Of the 143 patients, 29.4% (n = 42) had a written and signed advance directive document. However, only 35 of them were accessible and valid. The retrospective review showed that only 16 of the 35 documents had circumstances that could have been applied by doctors. Thus, most of the advance directives were flaws in the determination of medical procedures, as there was no full knowledge about the scenarios in which they would be applicable. |
Table 1: Studies analysed in the integrative literature review.
DISCUSSION
Philosopher Imannuel Kant stated that man is an end in itself, so from this perspective it is possible to understand that the individual, in a physical-psychiatric condition, is capable of deliberating decisions related to his life, so autonomy is a principle that must be respected, since it guarantees the dignity of human life [15]. In the light of this, it is necessary to reflect on how to guarantee the autonomy of the individual in geriatric patients.
Technological developments in medicine are known to have contributed to a better understanding of the human body and also to an increase in life expectancy, but it is necessary to reflect that many times the longest time lived may not correspond to a longer time with quality of life. In this way, it has to be understood that extending life by means of modern apparatuses can generate more health burdens than a benefit [13]. Furthermore, it is noted that with the increase in life expectancy there has also been the amplification of chronic non-Communicable Diseases (NCDs), being many incapacitators, progressive and incurable, such as dementia. Thus, the geriatric patients attacked by the NNCTs and the family/caregivers, due to the lack of knowledge of information about the anticipative directives, do not express their desire for them to be properly obeyed [12].
In this context, respect for the patient's autonomy is carried out by means of the VDAs, such as the vital will (TV), which testifies to the patient's will, when he is in a situation of mental lucidity, about how his clinical treatment [5] should be carried out. Furthermore, one can note the need for the training of the health team in relation to the subject. By means of a cross-cutting study carried out at the Medical Sciences School of Minas Gerais (FCMMG), only 12% of those interviewed understood the meaning of advance guidelines [5]. In another observational study with 1,652 people who only 50% of them had knowledge about the knowledge about declarations of will in life, making clear the need to widen the discussion on the theme [4]. Furthermore, it was verified in research carried out between the nurses, nurses and doctors that the participation of these professionals was fundamental in the guidelines of the patients and the families/caregivers. Therefore, sharing information on end-of-life care and co-responsibility among those involved occupies an unparalleled position to guarantee the autonomy, safety and dignity of the geriatric patient and family/caregiver, and even when the patient does not have a family nucleus qualified for this purpose [12].
CONCLUSION
In short, no matter how much there is a resolution from the Federal Council of Medicine on the advance directives of will (DAV), it is noted that this subject is still unknown to a large part of the population and health professionals, which makes it difficult to preserve and guarantee the autonomy of the elderly patients, particularly when they are affected by some irreversible and incurable ailment. In this way, it is understood that by means of these tools, anyone can express how they would like to be careful in a situation of finality, proposing limits for the use of measures for extending life, and thus guaranteeing dignity and better quality in dying.
REFERENCES
- Instituto Brasileiro de Geografia e Estatística (2019) Pesquisa Nacional por Amostra de Domicílios Contínua - PNAD Contínua, Instituto Brasileiro de Geografia e Estatística, State of Rio de Janeiro, Brazil.
- Instituto Brasileiro de Geografia e Estatística (2018) Projeções da População, Instituto Brasileiro de Geografia e Estatística, State of Rio de Janeiro, Brazil.
- Campolina AG, Adami F, Santos JLF, Lebrão ML (2013) A transição de saúde e as mudanças na expectativa de vida saudável da população idosa: Possíveis impactos da prevenção de doenças crônic Cad Saúde Pública 29: 1217-1229.
- Gómez MCB, Braojos RB, García MRD, Sánchez MCP, Díez SS (2019) Declaration of living wills, a vital testament for ensuring personal self-reliance. Gerokomos 30: 119-123.
- Gomes BMM, Salomão LA, Simões AC, Rebouças BO, Dadalto L, et al. (2018) Advance directives in geriatric medicine. Rev Bioética 26: 429-439.
- Dadalto L, Tupinambás U, Greco DB (2013) Diretivas antecipadas de vontade: Um modelo brasileiro. Rev Bioética 21: 463-476.
- Hausseler DPP (2014) Análise da percepção do paciente idoso em relação à Diretiva Antecipada de Vontade. Trabalho de Conclusão de Curso apresentado à Comissão de Residência Médica do HSPM-SP, para obter o título de Residência Médica, na área de Geriatria, São Paulo, Brazil.
- http://www.portalmedico.org.br/resolucoes/CFM/2012/1995_2012.pdf.
- de Melo JN (2019) Diretivas antecipadas de vontade: A possibilidade de inclusão do testamento vital no ordenamento jurídico
- Nunes MI, Anjos MF (2014) Diretivas antecipadas de vontade: Benefícios, obstáculos e limites. Rev Bioética 22: 241-251.
- Hassegawa LCU, Rubira MC, Vieira SM, Rubira APA, Katsuragawa TH, et al. (2019) Approaches and reflexions on advance healthcare directives in Brazil. Revista Brasileira de Enfermagem 72: 256-264.
- Gaspar RB, da Silva MM, Zepeda KGM, Silva IR (2019) Nurses defending the autonomy of the elderly at the end of life. Rev Bras Enferm 72: 1639-1645.
- Luck T, Rodriguez FS, Wiese B, van der Leeden C, Heser K, et al. (2017) Advance directives and power of attorney for health care in the oldest-old - results of the AgeQualiDe study. BMC Geriatr 17: 85.
- Alonso A, Dörr D, Szaboo K (2017) Critical appraisal of advance directives given by patients with fatal acute stroke: an observational cohort study. BCM Medical Ethics 18: 7.
- Da Silva TD (2020) Dignidade e autonomia na filosofia moral de Kant. Universidade Do Vale do Rio dos Sinos, São Leopoldo, Brazil.
Citation: Abritta MLR, Neri AC, Líbero IS, Colares TFB, Maia LC (2020) Living Wills and Geriatrics. J Gerontol Geriatr Med 6: 070
Copyright: © 2020 Marina Luiza Resende Abritta, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

