
Lower Seminal Oxytocin Levels have a Positive Association with Successful Intrauterine Insemination
*Corresponding Author(s):
Roudebush WEUniversity Of South Carolina School Of Medicine Greenville, Greenville, South Carolina, United States
Email:ROUDEBUS@greenvillemed.sc.edu
Abstract
Oxytocin is a neuropeptide that is mostly recognized for its role in parturition and lactation. Oxytocin and its receptor are also present in the reproductive tracts of males and females and is understood to support sperm transport in both as well. However, there is little to no information on seminal oxytocin levels and pregnancy outcomes, therefore this study compared oxytocin content in seminal fluid and Intrauterine Insemination (IUI) with known pregnancy outcomes. Retrospective analysis of seminal flid oxytocin levels from the male partner of couples undergoing IUI and pregnancy outcomes. Seminal fluid was obtained following semen washing (90% density centrifugation) prior to IUI. Seminal fluid was collected and frozen prior to being thawed and assayed. Oxytocin levels in saved seminal fluid were measured using a commercially available ELISA kit per manufacturer’s instructions. Seminal oxytocin levels between non- pregnant and pregnant IUI groups were compared using Students’ t-test. There were significantly (P < 0.01) lower seminal oxytocin levels in the pregnant (1.55 pg/mL) IUI group than the non-pregnant (3.76 pg/mL) IUI group. This study demonstrates that oxytocin is present in seminal fluid and patients with a successful IUI pregnancy outcome had significantly less oxytocin. The role of oxytocin, while not fully understood, may primarily facilitate sperm transport in the reproductive tracts in both sexes. Conflicting conclusions have been reported regarding the relationship between seminal oxytocin levels and sperm parameters. Further studies are required to elucidates the role seminal oxytocin has in male/female reproduction.
Keywords
Intrauterine insemination; Oxytocin; Pregnancy; Seminal fluid
Introduction
To facilitate spermatozoa survival, semen consists of secretions from the testes and the male secondary sex glands, i.e., seminal vesicles, prostate and the bulbourethral gland [1]. Some of the substances within the seminal fluid include fructose, prostaglandins, proteases and hormones. Fructose is broken down to pyruvate and lactate to provide energy for spermatozoa for survival and motility [2]. Of the various kinds of prostaglandins, PGE, 19-hydroxyl PGE1 and 19-hydroxyl PGF are some of the forms which have been demonstrated to have effects on sperm motility [3,4]. It has been shown that increased or decreased levels of PGE and 19- hydroxyl PGE decreased sperm motility [4]. While the addition of 19-hydroxyl PGF to semen reduced sperm motility [3]. Seminal fluid also contain proteases, which are primarily secreted by the prostate and have proteolytic effects that govern semen liquefaction [5].
Oxytocin is also found within seminal fluid. Oxytocin and oxytocin-like peptides are neuropeptides that occur in almost all vertebrate species [6]. Oxytocins also derived from the testes and play a role in male reproduction if affecting steroidogenesis and sperm transport [7]. In the female, oxytocin is known to stimulate uterine contractions, and has also been shown to play a role in other processes like proliferation of malignant cells and metabolism [8,9]. It had previously been postulated that seminal oxytocin may also have direct effects on sperm motility and transport [10]. The reason for the wide array of effects shown by oxytocin may lie in the high homology oxytocin shares with other neuropeptides, allowing for signaling crosstalk in different target tissues [10]. More knowledge on the role oxytocin plays in sperm transport may aid in intrauterine insemination practices.
Intrauterine Insemination (IUI) involves the direct transfer washed spermatozoa directly into the uterus. It bypasses the normal process of sperm transportation through the vagina and cervix from the seminal fluid in order to reach the uterus. Washing spermatozoa free of any seminal fluid prior to IUI effectively minimizes the peristaltic effect that a woman’s reproductive tract would normally undergo in response to seminal fluid since seminal prostaglandins and oxytocin are no longer present. The adequacy and technique utilized for seminal fluid washing and preparation may influence IUI success [11]. Additionally, IUI success can be affected by numerous factors, including female anatomy, partner age, infertility duration and type as well as the ovarian stimulation protocol [12].
The purpose of this pilot study was to analyze oxytocin content in seminal plasma and compare levels in patients whose IUI was successful versus those that were unsuccessful.
Materials and Methods
This retrospective cohort study, analysed seminal oxytocin content between positive and non-positive pregnancies following IUI. A total of 16 semen samples (deidentified) were evaluated in the manner described following. After an initial recording of semen volume, liquefaction, degree of viscosity and pH an aliquot (5 μL) of semen was loaded onto a disposable counting sperm chamber and evaluated for sperm concentration and motility. Sperm were washed free of seminal fluid via centrifugation (300g) prior to IUI. An aliquot (0.5-2.0 mL) of the sperm-free semen (post washed) was saved, and stored at - 80oC until analyzed. Seminal oxytocin content was determined by a commercial available ELISA (Enzo Life Sciences, Farmingdale, NY, USA) per manufacturer’s instructions.
Statistics
Oxytocin content and IUI pregnancy outcomes (deidentified) were compared by Students’ t-test. Data on patient demographics (deidentified), or other factors affecting the samples were not investigated for purposes of this study.
Results
The overall pregnancy rate was 62.5% (10/16). We noted a statistically significant difference in oxytocin levels between the pregnant group and the non-pregnant group, t(15)=5.82, p < 0.01. Patients who became pregnant had a significantly lower oxytocin level of 1.55 pg/mL (SD=0.70), when compared to non-pregnant patients, who had an oxytocin level of 3.76 pg/mL (SD=1.69) (Figure 1).
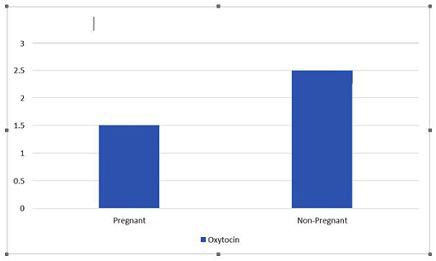 Figure 1: Seminal oxytocin and IUI outcomes.
Figure 1: Seminal oxytocin and IUI outcomes.
Discussion
Successful pregnancy outcomes has a myriad factors related to both male and female components, with approximately half of all infertile cases are found to be “male factor” in origin [13]. Male factor infertility can be caused by impaired testicular function due to chromosomal abnormalities, isolated spermatogenic impairment due to Y chromosome microdeletions, and congenital absence of the vas deferens due to cystic fibrosis transmembrane conductance regulator (CTFR) gene mutation [14]. Other, non-spermatogenesis factors, may result in male factor such as abnormal oxytocin secretions.
Oxytocin plays a diverse role in human biology across a plethora of physiological systems. In addition to numerous non-reproductive roles, oxytocin may aid in facilitating delivery of sperm to the site of fertilization via peristaltic contractions of the female reproductive tract [8], as well as supporting of sperm motility. We are now learning more about the role that oxytocins play by means of acting directly on male spermatozoa. Previous research has demonstrated the impact that oxytocins have on human sperm function with regards to motility [10].
Conclusion
Results from this pilot study do suggest that seminal oxytocin may be linked to the pregnancy potential of the spermatozoa used in intrauterine insemination. Our preliminary findings seem to point toward an association between improved IUI pregnancy outcomes and a lower oxytocin content. While this information is promising for better understanding the role oxytocin plays in fertility potential, additional studies will aid in the determination of just the role of seminal oxytocin has to ensure sufficient sperm motility, transport, and successful fertilizations. Further studies may lead us to a better understanding of why seminal oxytocin levels differ across males and samples given, as well as interventions that impact seminal oxytocin, and how to optimize levels prior to attempting pregnancy.
Acknowledgement
Not applicable.
Ethics Approval and Consent to Participate
This study has been reviewed and approved by the institutional review board of the University of South Carolina (Pro00070342), and all study procedures were carried out in compliance with the Declaration of Helsinki.
Consent for Publication
Not applicable.
Conflict of Interest
The authors declare no conflict of interest.
Funding
This study was funded, in part, by Prisma Health, Greenville, SC, USA.
References
- Ahmed B, Vaidyanathan G, Pillai SA, AlSabti J, Al-Khaduri M, et al. (2017) Factors influencing the success rate of intrauterine insemination: A retrospective study in Sultan Qaboos University Hospital. J Women's Health Care 6: 402.
- Kumar N, Singh AK (2015) Trends of male factor infertility, an important cause of infertility: A review of literature. J Hum Reprod Sci 8: 191-196.
- Tsujii H, Ohta E, Miah AG, Hossain S, Salma U (2006) Effect of fructose on motility, acrosome reaction and in vitro fertilization capability of boar spermatozoa. Reprod Med Biol 5: 255-261.
- Noda T, Ikawa M (2019) Physiological function of seminal vesicle secretions on male fecundity. Reprod Med Biol 18: 241-246.
- Isidori A, Conte D, Laguzzi G, Giovenco P, Dondero F (1980) Role of seminal prostaglandins in male fertility. I. Relationship of prostaglandin E and 19-OH prostaglandin E with seminal parameters. J Endocrinol Invest 3: 1-4.
- Gottlieb C, Svanborg K, Eneroth P, Bygdeman M (1988) Effect of prostaglandins on human sperm function in vitro and seminal adenosine triphosphate content. Fertil Steril 49: 322-327.
- Goverde HJ, Bisseling JG, Wetzels AM, Braat DD, Pesman GJ, et al. (1998) A neuropeptide in human semen: oxytocin. Arch Androl 41: 17-22.
- Watson ED, Nikolakopoulos E, Gilbert C, Goode J (1999) Oxytocin in the semen and gonads of the stallion. Theriogenology 51: 855-865.
- Anamthathmakula P, Winuthayanon W (2020) Mechanism of semen liquefaction and its potential for a novel non-hormonal contraception†. Biol Reprod 103: 411-426.
- Stadler B, Whittaker MR, Exintaris B, Middendorff R (2020) Oxytocin in the Male Reproductive Tract; The Therapeutic Potential of Oxytocin-Agonists and-Antagonists. Front Endocrinol (Lausanne) 11: 565731.
- McCormack SE, Blevins JE, Lawson EA (2020) Metabolic Effects of Oxytocin. Endocr Rev 41: 121-145.
- Müller A, Siemer J, Renner S, Hoffmann I, Beckmann MW, et al. (2006) Modulation of uterine contractility and peristalsis by oxytocin in estrogen-primed non-pregnant swine uteri. Eur J Med Res 11: 157-162.
- Leslie SW, Soon-Sutton TL, Khan MAB (2023) Male Infertility. StatPearls Publishing.
- Boomsma CM, Cohlen BJ, Farquhar C (2019) Semen preparation techniques for intrauterine insemination. Cochrane Database Syst Rev 10: CD004507.
Citation: Sanni M, Fowler LA, Zimmerman S, Chosed RJ, Roudebush WE (2024) Lower Seminal Oxytocin Levels have a Positive Association with Successful Intrauterine Insemination. J Reprod Med Gynecol Obstet 9: 158.
Copyright: © 2024 Sanni M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

