
Management of Pharyngocutaneous Fistula Post Total Laryngectomy during COVID-19 Pandemic using Type A Botulinum Toxin (Botox A)
*Corresponding Author(s):
Sakina GhauthDepartment Of Otorhinolaryngology, Faculty Of Medicine, University Of Malaya, Kuala Lumpur, Malaysia
Tel:+603-79677576,
Email:sakinaghauth@gmail.com
Abstract
Background: Pharyngocutaneous Fistula (PCF) is a well-known and devastating complication post total laryngectomy. With ongoing COVID-19 pandemic resulting in health resource constraints, non-surgical option with Botox A did wonder.
Methods: We presented two patients with residual/recurrent laryngeal carcinoma (T2N0M0) who developed PCF after total laryngectomy. Both subjects had curative radiotherapy for total dose of 70Gy to primary site and cervical regions. They had spontaneous saliva leakage a week after surgery. One of them had reconstruction with pectoralis major flap but failed to fully closure the fistula. Botox A was introduced into bilateral submandibular and parotid glands using ultrasound guided technique. Each gland was infiltrated with 20MU.
Results: Both patients recovered fully after 1 to 4 weeks after the Botox A injection, in addition to strict nasogastric feeding, wound dressing and broad spectrum antibiotics.
Conclusion: With limited timing for operation theatre during the most acute COVID-19 situation in our country, Botox A injection has been a successful adjunct in the conservative treatment of PCF.
Introduction
Pharyngocutaneous Fistula (PCF) remains the main and most common complication after total laryngectomy in laryngeal cancer. It usually develops within the first two weeks of laryngectomy. Surgical closure is warranted in cases of failed medical treatment. Unfortunately, the resulting coronavirus disease 2019 (COVID-19) pandemic has swept across the globe. Many institutions including our hospital in University Malaya Medical Center, Malaysia have cancelled elective and non-urgent procedures to conserve resources and limit exposure. Working within the resource constraint, other supplementary medical option is of utmost importance to allow the pharynx to heal. Here, we present two cases of PCF who were successfully treated with Type A botulinum toxin (Botox A) injection during the Covid-19 pandemic.
Case Report
Case 1
The patient was a 77-year-old man smoker who presented with worsening hoarseness and shortness of breath 3 months after completion of concurrent chemoradiation (CCRT, 35#, 70Gy) for glottic squamous cell carcinoma (SCC) T2N0M0. A residual cancer was confirmed from biopsy and he underwent total laryngectomy. Unfortunately, he developed wound breakdown and a fistula leak from the midline neopharynx, day 9 post operatively. Since the leak was huge, surgical closure with pectoralis major flap with insertion of salivary bypass tube was performed a week later. Despite the efforts of optimising his nutrition, comorbidities which included chronic obstructive pulmonary disease, the PCF persisted. We could not proceed with another revision flap closure due to a surge of COVID-19 cases and resource constraint, and he was subjected to Botox A injection to both submandibular and parotid gland. He recovered fully 4 weeks later with normal oral intake (Figure 1).
 Figure 1: 1a: Picture shows wound breakdown in the midline with discontinuity at the neopharynx and even exposed nasogastric tube; 1b: Leakage recurred 2 days post reconstruction of pectoralis major flap; 1c: Full recovery of fistula 1 month after Botox A injection
Figure 1: 1a: Picture shows wound breakdown in the midline with discontinuity at the neopharynx and even exposed nasogastric tube; 1b: Leakage recurred 2 days post reconstruction of pectoralis major flap; 1c: Full recovery of fistula 1 month after Botox A injection
Case 2
The patient was a 56-year-old man with T2N0M0 glottic squamous cell carcinoma 5 years ago where a curative CCRT 35#, 70Gy was completed. He had a recurrent laryngeal SCC proven from biopsy. A salvage total laryngectomy was performed, but he developed PCF at day 7 after surgery at stoma edge. A conservative treatment with broad spectrum antibiotics, strict nasogastric feeding, and wound dressing for 2 weeks, but to no avail. Botox A injection was done at the similar fashion as in case 1. The PCF healed completely after a week (Figure 2).
 Figure 2: 2a: Pharyngocutaneous fistula at the left stoma edge, post total laryngectomy 7 days; 2b: Total closure of PCF at 1 week after Botox A injection
Figure 2: 2a: Pharyngocutaneous fistula at the left stoma edge, post total laryngectomy 7 days; 2b: Total closure of PCF at 1 week after Botox A injection
Technique
The Botox A injection was performed by an experienced interventional radiologist using ultrasound guidance. Patient was placed in supine position. The skin over the parotid and submandibular glands was disinfected with antiseptic. An ultrasound with linear transducer (5-12MHz) was used to identify the glands in real-time and for precise needle visualization. A 22G needle was used to inject Type A botulinum toxin to the submandibular gland and superficial lobe of the parotid gland. Type A botulinum toxin (Dysport®) was diluted in normal saline to a final concentration of 10 MU/ml. The submandibular and parotid gland were injected with 20 MU each. A total of 80 MU was used. Except for mild discomfort, there were no serious complications encountered (Figure 3).
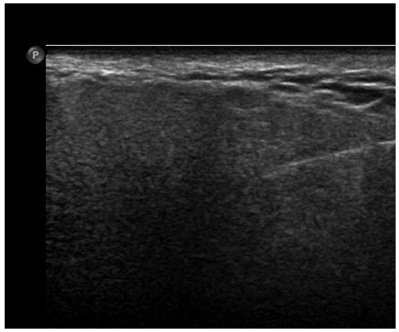 Figure 3: Ultrasound guided injection of right parotid glands, which showed accurate intraglandular needle position.
Figure 3: Ultrasound guided injection of right parotid glands, which showed accurate intraglandular needle position.
Discussion
PCF is a well-known and devastating complication post total laryngectomy, and remains an all to frequent complication of total laryngectomy, reporting rates of up to 58% [1]. Spontaneous closure with meticulous local wound care can be achieved in up to 86% of the cases [2]. The decision to return to theatre was taken by the lead surgeon and depended on a various factor including failure of conservative management and fitness of the patient. One of the most important factors was the current COVID--19 pandemic which the surge of cases started to peak from September 2020 in our country. This has placed an extraordinary demand on our health care system, particularly significant number of health care workers were also infected with coronavirus. Our case prioritization consisted of 4 categories: Acute emergency, emergency, and semi-emergency (Urgent and less urgent). PCF fell under the category of less urgent semi-emergency where the waiting period for a definitive reconstruction surgery was around 3 weeks, especially so when there was an internal outbreak of COVID--19 infection within our hospital.
In view of the above situation, we recommended Type A botulinum toxin injection to buy time and to ‘rest’ the fistula. The most important therapeutic principle was to reduce the secretion of the glandular tissue to facilitate the closure.
Botox A has been widely used in various head and neck conditions, which included strabismus, cervical dystonia, primary axillary hyperhidrosis, and blepharospasm, sialorrhoea and is approved by the U.S Food and Drug Administration (FDA) [3].
Ultrasound guided Botox A injection is safe, fast and easy to perform without subjecting the patient to general anaesthesia. Sonographic guided injection improves accuracy and helps avoid accidental injection into surrounding muscles such as pterygoid, masseteric muscles which is better than solely relying on anatomical landmarks [4].
In the presented cases, PCF healed as early as day 7 post injection of Botox A. In addition to that, both patients had subjective relief of coughing few days later due to reduction of saliva flowing into the stoma. There have been very limited reports on the use of Botox A in the treatment of PCF. It has been shown to be effective as an adjunct to temporarily reduce salivation, by Guntinas-Lichius in three patients with PCF where the fistula closed after 3 to 4 weeks [5]. Recent experiences suggest that, up to 100 MU Botox A into each parotid gland, leads to success. In our presented cases, each dose of 20 MU Dysport®, was injected using the above-mentioned technique.
In conclusion, with limited timing for operation theatre during the most acute COVID-19 situation in our country, Botox A injection has been a successful adjunct in the conservative treatment of PCF.
Conflict of Interest
There are no conflicts of interest to declare. The authors have no financial or proprietary interest in this manuscript to declare.
References
- Liang JW, Li ZD, Li SC, Fang FQ, Zhao YJ, et al. (2015) Pharyngocutaneous fistula after total laryngectomy: A systematic review and meta-analysis of risk factors. Auris Nasus Larynx 42: 353-359.
- Mäkitie AA, Niemensivu R, Hero M, Keski-Säntti H, Bäck L, et al. (2006) Pharyngocutaneous fistula following total laryngectomy: A single institution’s 10-year experience. Eur Arch Otorhinolaryngol 263: 1127-1130.
- Squires N, Wills A, Rowson J (2012) The management of drooling in adults with neurological conditions. Curr Opin Otolaryngol Head Neck Surg 20: 171-176.
- Ellies M, Laskawi R, Rohrbach-Volland S, Arglebe C, Beuche W (2002) Botulinum toxin to reduce saliva flow: Selected indications for ultrasound-guided toxin application into salivary glands. Laryngoscope 112: 82-86.
- Guntinas-Lichius O, Eckel HE (2002) Temporary reduction of salivation in laryngectomy patients with pharyngocutaneous fistulas by botulinum toxin A injection. Laryngoscope 112: 187-189.
Citation: Toong LY, Ghauth S, Bakar MZA, Narayanan P, Ng WL, et al. (2024) Management of Pharyngocutaneous Fistula Post Total Laryngectomy during COVID-19 Pandemic using Type A Botulinum Toxin (Botox A). J Otolaryng Head Neck Surg 10: 090.
Copyright: © 2024 Liew Yew Toong, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

