
Masked Uterine Rupture after Myomectomy Occluded by the Fetus: A Case Report
*Corresponding Author(s):
Koichiro KidoDepartment Of Obstetrics And Gynecology, School Of Medicine, Teikyo University, 2-11-1 Kaga, Itabashi-ku, Tokyo, Japan 173-8605, Japan
Tel:+81 339641211,
Email:kidoksci@gmail.com
Abstract
Background: Typical symptoms of uterine rupture are usually recognizable. Here, we present a case of masked uterine rupture in which the fetus was found to occlude the uterine tear.
Case presentation: A 31-year-old woman with a history of laparoscopic cystectomies and myomectomy presented with a normal first pregnancy. At 30 weeks’ gestation, she complained of uterine contractions. The pregnancy was maintained until 36 weeks, when the patient experienced sudden abdominal pain with no specific abnormalities in her vital signs or fetal well-being in both physical examination and laboratory test results. Threatened uterine rupture was diagnosed. During emergency laparotomy, the right torso of the fetus was found to block a full-thickness uterine tear. Both mother and neonate had uneventful recoveries.
Conclusion: Our case suggests that women who conceive after laparoscopic myomectomy are at a risk of silent uterine rupture and that symptoms of complete uterine rupture may be masked by the fetus. Recognizing the possibility of masked uterine rupture may aid in early diagnosis and lead to a better prognosis.
INTRODUCTION
Uterine rupture is a life-threatening condition for the mother and fetus [1]. Previous uterine operations, such as myomectomy and cesarean section, are risk factors for uterine rupture during pregnancy [2]. The number of pregnancies that occur after these conditions is increasing because of the increase in operative interventions for gynecological conditions and cesarean sections [3]. Typical symptoms of uterine rupture, such as severe abdominal pain and fetal bradycardia, are usually recognizable. Here, we report a case of complete uterine rupture with mild symptoms and reassuring fetal status after a previous myomectomy. During emergency cesarean section, the fetus was found to cover the uterine tear site and was considered to have masked typical findings.
CASE PRESENTATION
A 31-year-old nulligravida presented to our hospital with amenorrhea for the first time and was diagnosed with intrauterine pregnancy. At 24 years of age, she underwent laparoscopic cystectomy of a left endometriotic cyst. At 30 years, she underwent laparoscopic myomectomy and right endometriotic cystectomy. The pregnancy was uneventful until 30 weeks’ gestation when she complained of uterine contractions and was admitted to our hospital. The pregnancy was continued with bed rest, and ritodrine hydrochloride was administered initially intravenously and then orally. At 36 weeks’ gestation, she developed sudden abdominal pain. Her vital signs were stable, and the pain was localized to the upper abdomen. The abdominal wall was soft with no tenderness. There was no vaginal bleeding. Transabdominal ultrasound revealed the following: no perihepatic low echoic area; single fetus of appropriate size for gestational age; normal amniotic ?uid volume with an amniotic fluid index of 6.4 cm; no signs of placental thickening or retro-placental hematoma; and positive fetal heart rate with no bradycardia or tachycardia. Cardiotocogram monitoring showed irregular uterine contractions with no signs of diminished baseline variability or deceleration of the fetal heart rate, which was interpreted as a reactive pattern that indicated reassuring fetal status. Based on her past history and the above findings, she was diagnosed with threatened uterine rupture, and emergency laparotomy and cesarean section were performed.
During laparotomy, a small amount of lightly sanguineous ascites was noted. The uterine wall showed a full-thickness tear, measuring approximately 5 cm, of the left fundus, with the fetal right torso abutting the tear (Figures 1 and 2). The amniotic membrane beneath the ruptured uterine muscle site remained intact. A lower uterine segment cesarean section was performed, and a male neonate was delivered. The neonate weighed 2,764 grams and appeared non-asphyxiated with Apgar scores of 8 and 9 at 1 and 5 minutes, respectively. Umbilical arterial gas analysis showed a pH of 7.077; the neonate was not diagnosed with respiratory distress syndrome. The neonate had a subcutaneous hematoma of the right torso measuring approximately 5 cm in diameter (Figures 2 and 3). The placenta was delivered without complications. The ruptured uterine muscle was successfully repaired by two-layer suturing using 2-0 and 0 Vicryl, and an intrauterine device (FD-1®Fuji Latex, Tokyo, Japan) was placed in the uterine cavity. Postoperatively, the mother and neonate displayed uneventful puerperal and neonatal courses, respectively. They were discharged on day 8 according to the Japanese standard treatment course. Histopathological examination of the placenta revealed no signs of abruption.

Figure 1: Uterine tear.
The uterus is completely ruptured at the left fundus, with the tear measuring approximately 5 cm in diameter.

Figure 2: Infant subcutaneous hematoma.
The hematoma is 5 cm in diameter, corresponding to the size of the uterine rupture site.
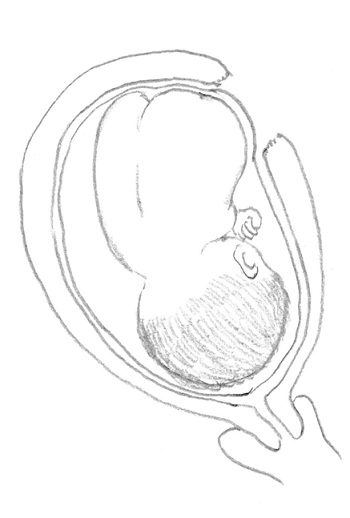 Figure 3: Schematic diagram of the operative findings.
Figure 3: Schematic diagram of the operative findings.
The uterine wall is completely torn at the left fundus, with the tear measuring approximately 5 cm in diameter; the fetal right torso was lodged in the tear. The amniotic membrane beneath the ruptured uterine muscle site remained intact.
CONSENT
The patient provided written consent for the publication of this case report and accompanying images.
DISCUSSION
Uterine rupture occurs in 1,500-5,000 births [3]. It is classified as either (A) complete uterine rupture when all layers of the uterine wall are separated or (B) incomplete uterine rupture when the uterine muscle is partially separated (uterine dehiscence). Recognized risk factors include prior cesarean sections, multiple births, past surgical operations, induction of labor, and augmentation of labor [1-3]. When uterine ruptures are not properly diagnosed and promptly treated, the maternal death rate is 0.2%, and fetal mortality rates range from 50% to 75%, with severe neurological morbidity developing in 18% of neonates [3]. In recent years, the number of at-risk cases has increased due to an increase in uterine fibroid nucleus surgeries and cesarean sections [3].
Typical symptoms of complete uterine rupture are severe abdominal pain, aberrant uterine contractions, uterine tenderness, circulatory collapse and fetal bradycardia. These signs and symptoms are easy to recognize and diagnose. Early symptoms of complete uterine rupture or incomplete uterine rupture, however, include weak abdominal pain, irregular uterine contractions, and mildly to moderately variable patterns in the fetal heart rate, which are not specific to this condition and are similar to findings seen in other complications such as threatened labor, threatened uterine rupture, or placental abruption. Therefore, uterine rupture is often not recognized in a timely manner and early diagnosis is difficult.
In our case, we first suspected early stage uterine rupture or incomplete uterine rupture based on the patient’s past history, but we were unable to identify typical findings and considered the diagnosis of threatened uterine rupture. Operative findings showed masked uterine rupture. Silent uterine rupture occluded by the intestine or omentum from outside the uterus has been reported and is relatively well recognized [4-6]. Recently, cases of occlusion of a myometrial tear by fetal parts, such as the fetal leg, have been reported [7]. In these cases, occlusion delays a vicious cascade consisting of bleeding from the ruptured site, fetal expulsion through the rupture, placental separation, circulatory collapse and finally fetal and/or maternal death.
The concept of masked uterine rupture consists of occlusion of the rupture and perforation by organs or the fetus, either from outside or inside the uterus [8]. The symptoms of this condition may lack the typical signs of severe abdominal pain or circulatory collapse and instead present with mild abdominal pain or mild-to-moderate variations in the fetal heart rate [8]. As the rate of high-risk pregnancies with previous operative history increases, clinicians should be more aware of the risk of masked uterine rupture.
In conclusion, our case findings suggest that women who conceive after laparoscopic myomectomy are at a risk of silent uterine rupture and that symptoms of complete uterine rupture may be masked by the fetus. Therefore, recognizing the possibility of masked uterine rupture may aid in early diagnosis, which can save maternal and fetal lives, and lead to a better prognosis.
DATA AVAILABILITY
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
CONFLICTS OF INTERESTS
The authors declare that there is no conflict of interest regarding the publication of this article.
ACKNOWLEDGEMENTS
We would like to thank Editage (www.editage.jp) for English language editing.
REFERENCES
- Pontis A, Prasciolu C, Litta P, Angioni S (2016) Uterine rupture in pregnancy: Two case reports and review of literature. Clin Exp Obstet Gynecol 43: 304-309.
- Koo Y-J, Lee J-K, Lee Y-K, Kwak D-W, Lee I-H, et al. (2015) Pregnancy Outcomes and Risk Factors for Uterine Rupture After Laparoscopic Myomectomy: A Single-Center Experience and Literature Review. J Minim Invasive Gynecol 22: 1022-1028.
- Vilchez G, Nazeer S, Kumar K, Warren M, Dai J, et al. (2017) Contemporary epidemiology and novel predictors of uterine rupture: A nationwide population-based study. Arch Gynecol Obstet 296: 869-875.
- Kuwata T, Matsubara S, Usui R, Uchida S-I, Sata N, et al. (2011) Intestinal adhesion due to previous uterine surgery as a risk factor for delayed diagnosis of uterine rupture: A case report. J Med Case Rep 5: 523-525.
- Koshiba A, Koshiba H, Noguchi T, Iwasaku K, Kitawaki J (2012) Uterine perforation with omentum incarceration after dilatation and evacuation/curettage: Magnetic resonance imaging findings. Arch Gynecol Obstet 285: 887-890.
- Fukutani R, Hasegawa J, Arakaki T, Oba T, Nakamura M, et al. (2017) Silent uterine rupture occluded by intestinal adhesions following laparoscopic myomectomy: A case report. J Obstet Gynaecol Res 43: 1209-1211.
- Blihovde L, Tawfik J, Hill DA (2010) Prelabor third-trimester uterine rupture in an unscarred uterus with occlusion by fetal small parts: A case report. J Reprod Med 55: 437-440.
- Matsubara S (2012) "Masked uterine rupture": key to diagnosis. Arch Gynecol Obstet 286: 1075-1076.
Citation: Yatsugi K, Kido K, Shiba M, Ryo E, Ayabe T (2020) Masked Uterine Rupture after Myomectomy Occluded by the Fetus: A Case Report. J Reprod Med Gynecol Obstet 5: 060.
Copyright: © 2020 Keita Yatsugi, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

