
Maternal Death Due to Acute Aortic Dissection-Autopsy Diagnosis: A Case Report
*Corresponding Author(s):
Burcu KasapDepartment Of Obstetrics And Gynecology, School Of Medicine, Mugla Sitki Kocman University, Mugla, Turkey
Tel:+90 2522114800/5156,
Email:burcuharmandar@gmail.com, burcuharmandar@mu.edu.tr
Abstract
Aortic dissection is a very rare but potentially fatal entity during pregnancy. Herein, we report a case of sudden maternal death due to aortic dissection which was diagnosed via autopsy. A 36-year-old, 39 weeks, G3P2 (G:Gravida, Parity:2) patient admitted to emergency department with onset of labor. During the clinical examination all vital signs were normal but the patient suddenly fell down before obstetrical examination. The patient had no cardiac or respiratory function in the emergency room and underwent emergent cesarean section under cardiopulmonary resuscitation. The neonate survived without any hypoxic sequela but the patient died. According to autopsy reports there was an intimal tear on the ascending aorta and hemopericardium with 1000 ml of blood was found. In general, aortic dissection occurs in patients with previous hypertension or collagen formation disorders. However the presented case had two previous pregnancies which were able to reach term without any complications and had no any preexisting risk factors like preeclampsia or collagen vascular diseases for aortic dissection. Despite the advances in antenatal care, unpreventable and unexpected maternal deaths still remain high. So in order to decrease maternal mortality rates, unexpected maternal deaths must be evaluated by collaboration with forensic medicine.
INTRODUCTION
Acute aortic dissection is a very rare but potentially fatal entity during pregnancy unless treated [1]. Aortic dissection is characterized by a tear in the intimal layer of aorta which allows blood to flow into medial layer. The blood stream penetrates into the damaged medial segment, splits the median laminar plate and finally dissects the aorta [2].
The incidence of aortic dissection in overall population is 2.6-3.5 per 100,000 persons annually [3]. But female population generally present with the disease at later ages compared to males [4]. The incidence of acute aortic dissection during pregnancy is about 0.4 cases per 100,000 person years [5,6]. Half of the aortic dissection cases occur in the third trimester of pregnancy and in the postpartum period when the hemodynamic stress is the greatest [1,7]. Despite its rarity, aortic dissection in pregnancy may result in adverse maternal and fetal outcomes [8]. Atherosclerosis, hypertension, genetic disorders of connective tissue, genetic conditions such as turner’s syndrome, valvular abnormalities and vascular diseases like preeclampsia are risk factors of aortic dissection [9]. In pregnancy aortic compression due to the gravid uterus was also hypothesized to increase outflow resistance on the aorta [10]. Pregnancy induced hormonal changes, like increased estrogen concentrations during pregnancy, also may disrupt the normal corrugation of elastic fibers [11]. These alterations increase the risk of aortic dissection during pregnancy especially in women with predisposing genetic conditions and other risk factors.
It may be very difficult to diagnose aortic dissection in pregnant women without preexisting risk factors since the symptoms of this rare entity might interfere with symptoms of pregnancy. Herein, we report maternal death of a 36 years old woman without any existent risk factors for aortic dissection and we aimed to report the maternal and fetal outcome of this rare entity and supplement the data of autopsy findings with the related literature.
A CASE PRESENTATION
A 36-year-old, 39 weeks, G3P2 patient died suddenly after admission to emergency department with onset of labor. Her medical history revealed no predisposing risk factors for vessel pathology like connective tissue or genetic disorders. The patient’s previous two pregnancies had reached to term without any complications and she delivered two term babies via vaginal route. Her vital signs were in normal ranges during admission. She had abdominal and back pain resembling labor pain. Just after admission to the emergency department after the vital signs was taken she fell down and turned black-blue and cardio respiratory arrest was diagnosed. She had been intubated and emergency perimortem cesarean section was performed via cardiopulmonary resuscitation and fortunately the neonate survived without any hypoxic sequela. The woman died despite all efforts. The public prosecutor of Milas- Mu?la ordered medico-legal autopsy. One Forensic Medicine specialist performed the autopsy on the same day of death. All three body cavities (cranium, thorax and abdomen) were examined.
RESULTS
External inspection
Autopsy findings

Figure 1: 1000 ml of blood in pericardial cavity.
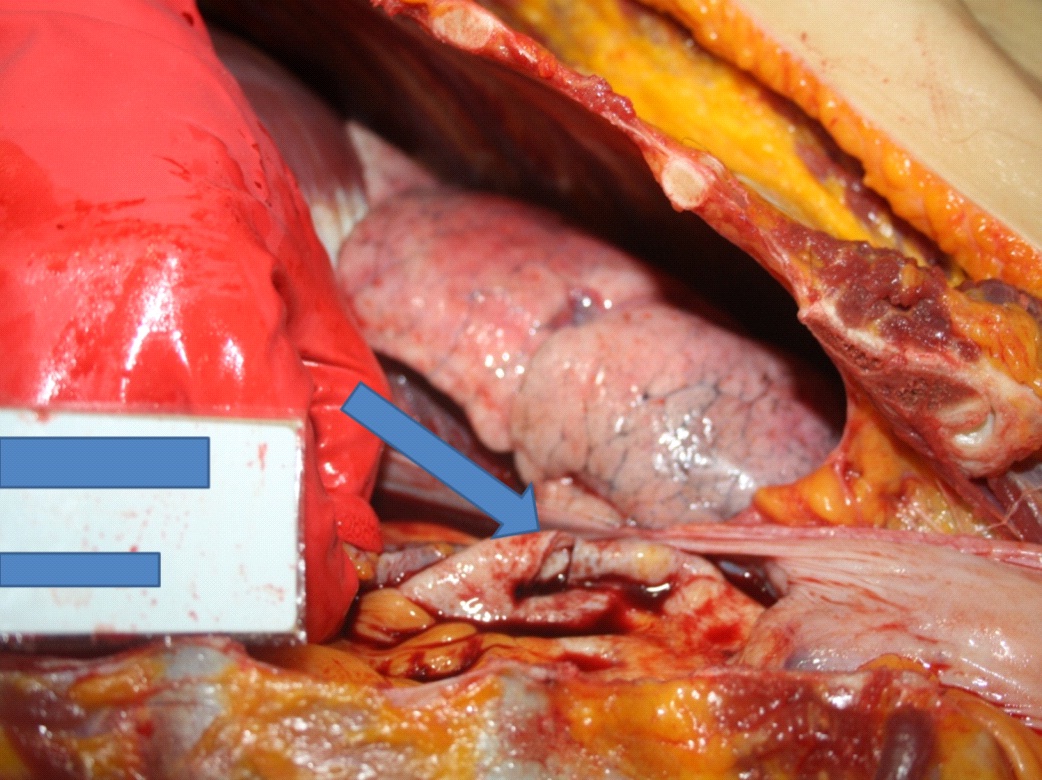
Figure 2: A two cm intimal tear on the ascending aorta over the aortic arch.
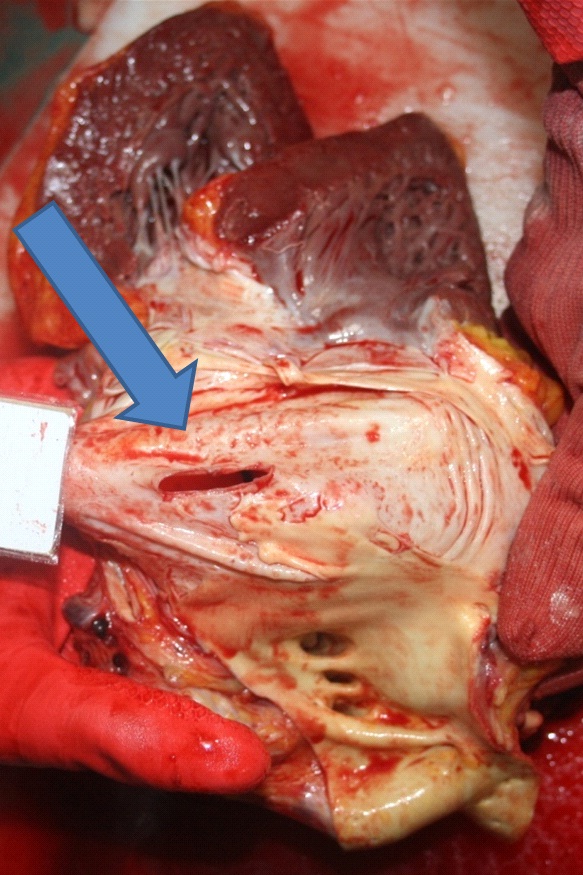
Figure 3: A two cm intimal tear on the ascending aorta over the aortic arch.
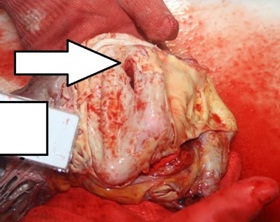
Figure 4: Absence of intimal plate in the ascending aorta.
The abdominal cavity was normal except the postpartum appearance of uterus. No toxic material was detected in toxicological examination.
DISCUSSION
The incidence of acute aortic dissection during pregnancy is 0.4 cases per 100,000 person years [5,6]. The estimated incidence of aortic dissection was 11.7-fold higher in pregnant women compared to non-pregnant women [9]. Atherosclerosis and hypertension are general risk factors for acute aortic dissection, but the incidence of aortic dissection might increase in pregnant women with genetic disorders of connective tissue such as Marfan Syndrome (MFS), Loeys-Dietz Syndrome (LDS), some forms of familial Thoracic Aortic Aneurysms and Aortic Dissections (TAAD), genetic conditions such as turner’s syndrome, valvular abnormalities like bicuspid aorta and vascular diseases like preeclampsia [9]. The presented case had no diagnosed familial connective tissue disorders such as MFS, LDS, TAAD or turner’s syndrome. She had no previous history of cardiac and vascular disorders or no history of hypertension in the current pregnancy. The autopsy findings also confirmed normal valvular structure of the heart and aorta with 3 cusps. The size of the aortic root was within the normal ranges and no aneurysms were detected on the vascular structures.
Besides the preexisting congenital valvular, connective tissue or genetic disorders, aortic compression due to gravid uterus was hypothesized to increase outflow resistance on the aorta [10]. Pregnancy induced hormonal changes, like increased estrogen concentrations during pregnancy, may also disrupt the normal corrugation of elastic fibers [11]. These alterations together may increase the risk of aortic dissection during pregnancy especially in women with predisposing genetic conditions.
Patients with inherited connective tissue disorders and valvular disorders like bicuspid aorta should be counseled preconceptionally and should be informed about the increased risk for acute aortic dissection during pregnancy. Rajagopalan et al., reported an overall maternal mortality of 21% and fetal mortality of 10% and 35% for type A and B dissections [12].
In patients with increased risk of acute aortic dissection surgical repair of the preexisting disorder can be performed with less morbidity before pregnancy. If the aortic dissection is diagnosed during pregnancy the management depends on the gestational age. Before 28 weeks of singleton pregnancies, surgical repair of aortic dissection is recommended while the fetus is in utero. However, after 32 weeks of gestation synchronous cesarean delivery and surgical repair of aortic dissection might be performed. Between 28 and 32 weeks surgical repair of aortic dissection and cesarean delivery in the case of fetal distress should be considered [13].
Acute aortic dissection is a catastrophic disorder in pregnancy. So the patients with preexisting risk factors for aortic dissection should be counseled before pregnancy and should be followed up by a team including perinatologist, anesthesiologist, cardiovascular surgeon and neonatologist during pregnancy. But in patients without known risk factors for aortic dissection, symptoms should be evaluated delicately and interventions should be performed timely in order to save both maternal and neonatal lives. In conclusion, the relative increased risk acute aortic dissection during pregnancy should be kept in mind in symptomatic patients without risk factors.
REFERENCES
- Özdemir B (2005) Aortic Dissection in Pregnancy. Turkish Clinics J Int Med Sci 1: 54-58.
- Vega SJ, Zamorano GJ, Pereira CN, Galleguillos GA (2014) [Acute aortic syndrome. Review and update of the literature]. Rev Med Chil 142: 344-352.
- Mészáros I, Mórocz J, Szlávi J, Schmidt J, Tornóci L, et al. (2000) Epidemiology and clinicopathology of aortic dissection. Chest 117: 1271-1278.
- Nienaber CA, Fattori R, Mehta RH, Richartz BM, Evangelista A, et al. (2004) Gender-related differences in acute aortic dissection. Circulation 109: 3014-3021.
- Thalmann M, Sodeck GH, Domanovits H, Grassberger M, Loewe C, et al. (2011) Acute type A aortic dissection and pregnancy: a population-based study. Eur J Cardiothorac Surg 39: 159-163.
- Immer FF, Bansi AG, Immer-Bansi AS, McDougall J, Zehr KJ, et al. (2003) Aortic dissection in pregnancy: analysis of risk factors and outcome. Ann Thorac Surg 76: 309-314.
- Guo C, Xu D, Wang C (2011) Successful treatment for acute aortic dissection in pregnancy---Bentall procedure concomitant with cesarean section. J Cardiothorac Surg 6: 139.
- Ray P, Murphy GJ, Shutt LE (2004) Recognition and management of maternal cardiac disease in pregnancy. Br J Anaesth 93: 428-439.
- Nasiell J, Lindqvist PG (2010) Aortic dissection in pregnancy: the incidence of a life-threatening disease. Eur J Obstet Gynecol Reprod Biol 149: 120-121.
- Ohlson L (1978) Effects of the pregnant uterus on the abdominal aorta and its branches. Acta Radiol Diagn (Stockh) 19: 369-376.
- Manalo-Estrella P, Barker AE (1967) Histopathologic findings in human aortic media associated with pregnancy. Arch Pathol 83: 336-341.
- Rajagopalan S, Nwazota N, Chandrasekhar S (2014) Outcomes in pregnant women with acute aortic dissections: a review of the literature from 2003 to 2013. Int J Obstet Anesth 23: 348-356.
- Zeebregts CJ, Schepens MA, Hameeteman TM, Morshuis WJ, de la Rivière AB (1997) Acute aortic dissection complicating pregnancy. Ann Thorac Surg 64: 1345-1348.
Citation: Karbeyaz K, Kasap B, Erba? M, Balc? Y, Canverenler E (2015) Maternal Death Due to Acute Aortic Dissection-Autopsy Diagnosis: A Case Report. J Clin Stud Med Case Rep 2: 013.
Copyright: © 2015 Burcu Kasap, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

