
Medical Malpractice in Adult Hydrocephalus: An Analysis of 32 Cases
*Corresponding Author(s):
Isabella L. PecorariDepartment Of Neurological Surgery, Montefiore Medical Center, Albert Einstein College Of Medicine, Bronx, New York, United States
Tel:718-920-4216,
Fax:718-547-4591
Email:isabella.pecorari@einsteinmed.edu
Abstract
- Introduction
Malpractice litigation is common in the medical field, with surgical specialties facing some of the highest prosecution rates. Understanding the reasons for litigation related to the treatment of specific neurosurgical conditions remains limited. The aim of this study is to identify factors that influence legal claims in cases related to the management of adult hydrocephalus.
- Methods
A systematic search of the online legal database Westlaw was utilized to identify cases pertaining to the management of adult hydrocephalus between 1989-2021. Variables related to plaintiff demographics, reason for litigation, plaintiff complaints, defendant specialties, trial outcomes, and payouts were recorded. These characteristics were compared between cases in favor of plaintiffs versus defendants.
- Results
Thirty-two cases met inclusion criteria. The most common reason for litigation was failure to diagnose (50%), with the most common preoperative medical complaints being headache (50%) and nausea and/or vomiting (28.1%). Hospitals (25%) were the most frequently named defendant, followed by neurosurgeons (21.9%) and emergency medicine physicians (21.9%). Most cases resulted in a jury verdict in favor of the defense (50%). For the cases that returned a plaintiff verdict, the average payout was $2,030,578.18 while the average cost of settlement was $298,333.33.
- Conclusion
The most common reason for litigation in the management of hydrocephalus was due to a failure in diagnosing the condition, with half of all cases returning a defense verdict. While a majority of cases were brought against a hospital or medical center, neurosurgery and emergency medicine were the most frequently listed medical specialists.
Keywords
Hydrocephalus; Medical Malpractice; Medico legal; Neurosurgery
Introduction
Malpractice in medicine is a common occurrence and is considered an almost inevitable incident for most physicians. Out of all the medical fields, surgical subspecialties have historically been known to face the high estrates of lawsuits. Neurosurgeons, in particular, have been found to be one of the most frequently sued surgical subspecialists, with yearly proceeding rates as high as 20% and average claims of almost $500,000.00 [1, 2]. Although awareness of the prevalence of medical lawsuits among physicians and residents has been increasing, the understanding of the nuances related to litigation and the treatment of specific medical conditions remains limited. Legal trials related to the treatment of hydrocephalus, for example, is one area where malpractice claims analysis is needed to provide physicians with further insight into what risk factors may increase the risk of prosecution.
Hydrocephalus is the aberrant accumulation of cerebrospinal fluid (CSF) within the ventricular system of the brain. This condition can be congenital, idiopathic, or develop subsequent to an underlying problem, such as trauma or infection [3]. Hydrocephalus is often classified into communicating versus non communicating subtypes, which occur due to impaired CSF absorption or obstruction to the flow of CSF between ventricular pathways, respectively [4]. Although this disorder can occur at any age, it is most commonly observed in pediatric patients and the elderly [5]. While symptoms may be variable among those who are affected, the most commonly experienced side effects in the adult population include nausea, lethargy, headaches, seizures, gait abnormalities, cognitive deficits, and visual disturbances [3, 6]. Due to the somewhat nonspecific symptoms that some patients may exhibit, this condition may be undiagnosed during initial evaluation. However, timely diagnosis is crucial as untreated hydrocephalus can lead to serious and fatal consequences, including brain herniation and death [7]. Management of hydrocephalus depends on the underlying etiology of the condition and may include medical and surgical interventions, including lumbar puncture, external ventricular drains, or ventriculoperitoneal shunts [8]. Definitive surgical management is often ultimately required for many patients with hydrocephalus, however, shunts frequently develop complications, requiring additional surgeries and revisions [9].
At this time, litigation analysis focused on the management of hydrocephalus remains limited. Our aim is to delineate the most common reasons for legal proceedings to occur against physicians treating patients with this condition. Through detailing plaintiff complaints, demographics, and reasons for litigation, we hope to recognize which variables may contribute to adverse legal outcomes and identify ways to mitigate these risk factors.
Methods
In this study, a review of cases focused on the management of hydrocephalus between 1989-2021 was conducted utilizing Westlaw Edge (Thomas Reuters). This database serves as an online resource for subscription-users to access a wide-array of attorney-verified medical malpractice claims made throughout the United States. Cases that related to malpractice and the medical treatment of adult hydrocephalus were the focus of the analysis. Statements from state and federal-level courts that contained the search terms “malpractice and hydrocephalus” were queried. Each case was individually analyzed in order to determine if eligibility for inclusion was met. Inclusion criteria included plaintiffs at least 18 years of age and claims specifically related to the diagnosis or treatment of hydrocephalus. Criteria for exclusion included duplicate cases, plaintiffs less than 18 years of age, and cases that were not relevant to the management of hydrocephalus. The primary outcomes of interest for each case included plaintiff demographics, geographic location of court trials, reasons for litigation, medical specialties of defendants, plaintiff claims, and trial outcomes. Payouts for cases resulting in settlements or those ruling in favor of plaintiffs were also recorded. For our statistical analysis, means and standard deviations were used to summarize continuous variables and a t-test (parametric) or Wilcoxon rank-sum test (non-parametric) was used to compare cases in favor of defendants and cases in favor of plaintiffs. Categorical variables were analyzed using proportions and frequencies and compared using Fisher exact or chi-square tests.
Results
Demographics
A total of 212 cases relating to hydrocephalus were initially identified from our search criteria, 32 of which met the criteria for inclusion. Out of the 180 cases that were excluded, 19 cases were duplicates, 6 cases demonstrated no evidence of hydrocephalus, and the remaining were unrelated to the treatment of hydrocephalus. Out of the cases that were included in our analysis, 16 (50%) were male and 16 (50%) were female (Table 1). The average age of plaintiffs was 41.9 +/- 14.5 years.
|
Variable |
Total (n = 32) |
|
Demographics |
|
|
No. of males |
16 (50.0%) |
|
No. of females |
16 (50.0%) |
|
Patient age in years (mean +/- SD) |
41.9 +/- 14.5 |
|
Geographic Distribution |
|
|
California |
7 (21.9%) |
|
Texas |
4 (12.5%) |
|
New York |
3 (9.4%) |
|
Alabama |
2 (6.3%) |
|
Florida |
2 (6.3%) |
|
Maryland |
2 (6.3%) |
|
Michigan |
2 (6.3%) |
|
Missouri |
2 (6.3%) |
|
New Jersey |
2 (6.3%) |
|
Virginia |
2 (6.3%) |
|
Connecticut |
1 (3.1%) |
|
Idaho |
1 (3.1%) |
|
Illinois |
1 (3.1%) |
|
Pennsylvania |
1 (3.1%) |
|
Reasons for litigation |
|
|
Failure to diagnose |
16 (50.0%) |
|
Failure to treat |
7 (21.9%) |
|
Failure to recognize EVD or shunt malfunction |
7 (21.9%) |
|
Post-surgical complication |
3 (9.4%) |
|
Delayed treatment |
2 (6.3%) |
|
Surgical complication |
2 (6.3%) |
|
Failure to diagnose post-surgical infection |
1 (3.1%) |
|
Plaintiff complaints |
|
|
Pre-op claims/those who did not undergo surgery |
|
|
Headache or Chronic Headache |
16 (50.0%) |
|
Nausea/Vomiting |
9 (28.1%) |
|
Death |
7 (21.9%) |
|
Hemorrhage |
6 (18.8%) |
|
Respiratory Distress |
6 (18.8%) |
|
Vision Impairment or Loss |
4 (12.5%) |
|
Paraplegia |
2 (6.3%) |
|
Seizure |
1 (3.1%) |
|
Aphasia |
1 (3.1%) |
|
Financial Loss |
1 (3.1%) |
|
Motor Weakness |
1 (3.1%) |
|
Meningitis |
1 (3.1%) |
|
Memory Loss |
1 (3.1%) |
|
Post-op claims |
|
|
Death |
11 (34.4%) |
|
Financial Loss |
4 (12.5%) |
|
Headache or Chronic Headache |
4 (12.5%) |
|
Emotional distress |
2 (6.3%) |
|
Hemorrhage |
1 (3.1%) |
|
Memory Loss |
1 (3.1%) |
|
Vision Impairment or Loss |
1 (3.1%) |
|
Seizure |
1 (3.1%) |
|
Aphasia |
1 (3.1%) |
|
Nausea/Vomiting |
1 (3.1%) |
|
Specialties of Defendants |
|
|
Hospital, Medical Center, or Healthcare System |
9 (28.1%) |
|
Neurosurgery |
7 (21.9%) |
|
Emergency |
7 (21.9%) |
|
Neurology |
5 (15.6%) |
|
Internal Medicine |
2 (6.3%) |
|
General surgeon |
1 (3.1%) |
|
OBGYN |
1 (3.1%) |
|
Family Medicine |
1 (3.1%) |
|
Physiatry |
1 (3.1%) |
|
Physician Assistant |
1 (3.1%) |
|
Radiology |
1 (3.1%) |
|
Legal Outcome |
|
|
Settlement |
5 (15.6%) |
|
Defendant verdict |
16 (50.0%) |
|
Plaintiff verdict |
11 (34.4%) |
|
Mean Payouts |
|
|
Settlement |
$ 298,333.33 |
|
Plaintiff verdict |
$2,030,578.18 |
|
Settlement range |
$250,000 - $395,000 |
|
Plaintiff verdict range |
$145,000 - $6,000,000 |
*5 cases had more than one reason for litigation
**10 cases with unknown defendant specialties, 8 cases had more than one defendant specialty listed
***2 settlements did not disclose payment amount
Table 1: Summary of Key Characteristics
- Geographic Distribution
There was a total of 14 states represented in the analysis. The state with the most number of court filings was California (n = 7, 21.9%), followed by Texas (n = 4, 12.5%) and New York (n = 3, 9.4%) (Table 1).
- Specialties of Defendants
Cases included in the analysis listed a hospital, medical center, or healthcare system as the most frequently cited defendants (n = 9, 28.1%) (Table 1). Neurosurgery (n = 7, 21.9%), emergency medicine (n = 7, 21.9%), and neurology (n = 5, 15.6%) were the next most frequently listed specialty of cases relating to the treatment of hydrocephalus. There were 10 cases (31.2%) that did not specify the medical specialty of the defendants.
- Reasons for Litigation
Failure to diagnose hydrocephalus was the most frequently cited reason for litigation among cases (n = 16, 50%) (Table 1). The next most common allegations were failure to treat hydrocephalus (n = 7, 21.9%) and failure to recognize an external ventricular drain (EVD) or shunt malfunction (n = 7, 21.9%). Other reasons for filing a malpractice claim included post-surgical complication (n = 3, 9.4%), surgical complication (n = 2, 6.3%), delayed treatment (n = 2, 6.3%), and failure to diagnose post-surgical infection (n = 1, 3.1%).
- Plaintiff Complaints
Among those complaints listed by plaintiffs in the pre-operative period and by plaintiffs who did receive surgical treatment of hydrocephalus, headache was the most common grievance (n = 16, 50%), followed by nausea and/or vomiting (n = 9, 28.1%) (Table 1, Figure 1). Other reported complaints included death (n = 7, 21.9%), intracranial hemorrhage (n = 6, 18.8%), respiratory distress (n = 6, 18.8%), and vision loss or impairment (n = 4, 12.5%). Post-surgical plaintiff complaints included death (n = 11, 34.4%), financial loss (n = 4, 12.5%), and headache (n = 4, 12.5%).
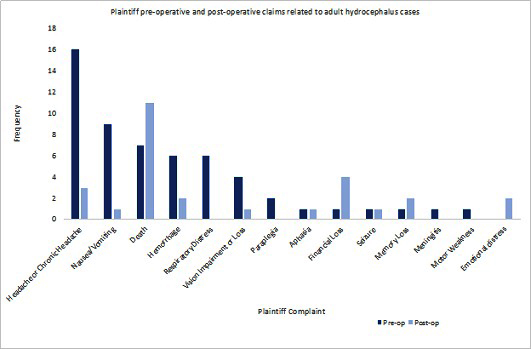 Figure 1: The most frequent pre-operative claims, including those claims for plaintiffs who did not undergo surgery, were headache (n=16, 50%), nausea/vomiting (n=9, 28.1%), and death (n=7, 21.9%). The most frequent post-operative complaints were death (n=11, 34.4%), financial loss (n=4, 12.5%), and headache (n=4, 12.5%).
Figure 1: The most frequent pre-operative claims, including those claims for plaintiffs who did not undergo surgery, were headache (n=16, 50%), nausea/vomiting (n=9, 28.1%), and death (n=7, 21.9%). The most frequent post-operative complaints were death (n=11, 34.4%), financial loss (n=4, 12.5%), and headache (n=4, 12.5%).
- Legal Outcomes and Payments
Out of the 32 medical malpractice cases that were analyzed in this study, a jury verdict in favor of the plaintiff was ruled in 11 cases (34.4%) and in favor of the defendant in 16 cases (50%) (Table 1). There were 5 cases (15.6%) that resulted in a settlement. The average cost for settlements was $298,333.33 and the average payout for cases with plaintiff verdicts was $2,030,578.18. Analyzing the medical specialties that had at least 2 cases listed, the defendants with the greatest average payout was neurology at $3,937,943.50 (Table 2). The second highest payout was among cases that listed a hospital, medical center, of healthcare system as a defendant, at $2,508,629.00. The next highest payouts were for neurosurgeons ($1,853,460.00) and emergency medicine physicians ($1,265,000.00). Out of the 5 cases that ended in a settlement, 2 cases did not list the payment amount while the remaining 3 cases did not specify the medical specialty involved in the case.
|
Average Payout |
||
|
Specialties of Defendants |
Plaintiff Verdict |
Settlement |
|
Emergency |
$1,265,000.00 |
- |
|
Family Medicine |
$1,650,000.00 |
- |
|
Hospital, Medical Center, or Healthcare System |
$ 2,508,629.00 |
- |
|
Internal Medicine |
- |
- |
|
Neurology |
$ 3,937,943.50 |
- |
|
Neurosurgery |
$1,853,460.00 |
- |
|
OBGYN |
$ 2,000,000.00 |
- |
|
Physiatry |
$ 4,000,000.00 |
- |
|
Physician Assistant |
$ 1,650,000.00 |
- |
|
Radiology |
- |
- |
|
General surgeon |
- |
- |
|
N/A |
$ 1,208,610.00 |
$298,333.33 |
*2 settlements did not disclose payment amount
Table 2: Average payout of defendants based on specialty
- Comparative Analysis between Plaintiff versus Defendant Verdicts
Comparative analysis of the 27 lawsuits that went to court revealed no statistically significant difference in cases that resulted in a plaintiff versus defendant verdict. However, cases that were tried before a circuit or superior court more likely to result in a defendant verdict (37.5%, n = 6 vs 3; 43.8%, n = 7 vs 2, respectively) (Table 3). Additionally, cases were more likely to return a verdict in favor of the defense rather than the plaintiff when a neurosurgeon was involved (31.2%, n = 5 vs 2, p = 0.446) or the reason for litigation was failure to recognize a shunt malfunction (31.2%, n = 5 vs 1, p = 0.174).
|
|
Defendant (N=16) |
Plaintiff (N=11) |
p value |
|
Age |
0.302 |
||
|
Mean (SD) |
46.182 (16.5) |
38.9 (13.6) |
|
|
Range |
26 – 73 |
22-62 |
|
|
Sex |
0.93 |
||
|
Female |
7 (43.8%) |
5 (45.5%) |
|
|
Male |
9 (56.2%) |
6 (54.5%) |
|
|
State |
0.143 |
||
|
Alabama |
1 (6.2%) |
1 (9.1%) |
|
|
California |
7 (43.8%) |
0 (0.0%) |
|
|
Connecticut |
1 (6.2%) |
0 (0.0%) |
|
|
Illinois |
1 (6.2%) |
0 (0.0%) |
|
|
Maryland |
1 (6.2%) |
1 (9.1%) |
|
|
Michigan |
1 (6.2%) |
0 (0.0%) |
|
|
Missouri |
1 (6.2%) |
1 (9.1%) |
|
|
New Jersey |
0 (0.0%) |
2 (18.2%) |
|
|
New York |
0 (0.0%) |
3 (27.3%) |
|
|
Pennsylvania |
0 (0.0%) |
1 (9.1%) |
|
|
Texas |
2 (12.5%) |
1 (9.1%) |
|
|
Virginia |
1 (6.2%) |
1 (9.1%) |
|
|
Type of Court |
0.147 |
||
|
Circuit Court |
6 (37.5%) |
3 (27.3%) |
|
|
Court of Common Pleas |
0 (0.0%) |
1 (9.1%) |
|
|
District Court |
2 (12.5%) |
1 (9.1%) |
|
|
State Court |
1 (6.2%) |
0 (0.0%) |
|
|
Superior Court |
7 (43.8%) |
2 (18.2%) |
|
|
Supreme Court |
0 (0.0%) |
3 (27.3%) |
|
|
Unknown |
0 (0.0%) |
1 (9.1%) |
|
|
Defendant Type |
0.678 |
||
|
Hospital |
2 (12.5%) |
1 (9.1%) |
|
|
Individual |
5 (31.2%) |
2 (18.2%) |
|
|
Multiple |
9 (56.2%) |
8 (72.7%) |
|
|
Defendant Specialty |
|
||
|
Hospital, Medical Center, or Healthcare System |
5 (31.2%) |
3 (27.3%) |
0.824 |
|
Emergency |
3 (18.8%) |
3 (27.3%) |
0.601 |
|
Neurology |
2 (12.5%) |
2 (18.2%) |
0.683 |
|
Neurosurgery |
5 (31.2%) |
2 (18.2%) |
0.446 |
|
Physiatry |
0 (0.0%) |
1 (9.1%) |
0.219 |
|
Physician Assistant |
1 (6.2%) |
1 (9.1%) |
0.782 |
|
Family Medicine |
0 (0.0%) |
1 (9.1%) |
0.219 |
|
Ob-Gyn |
0 (0.0%) |
1 (9.1%) |
0.219 |
|
Internal Medicine |
2 (12.5%) |
0 (0.0%) |
0.223 |
|
Radiology |
1 (6.2%) |
0 (0.0%) |
0.398 |
|
General Surgeon |
1 (6.2%) |
0 (0.0%) |
0.398 |
|
Reason for Litigation |
|
||
|
Post-surgical complication |
2 (12.5%) |
1 (9.1%) |
0.782 |
|
Failure to diagnose |
6 (37.5%) |
7 (63.6%) |
0.182 |
|
Failure to treat |
3 (18.8%) |
2 (18.2%) |
0.97 |
|
Surgical complication |
2 (12.5%) |
0 (0.0%) |
0.223 |
|
Failure to recognize shunt malfunction |
5 (31.2%) |
1 (9.1%) |
0.174 |
|
Delayed treatment |
1 (6.2%) |
1 (9.1%) |
0.782 |
*5 defendant and 2 plaintiff cases did not list sex
Table 3: Comparative Analysis of Plaintiff versus Defendant Verdicts
Discussion
This paper describes 32 years of malpractice litigation related to the management of adult hydrocephalus in the United States, from 1989 to 2021. In this analysis, we found that the most common reason for litigation was failure of a physician to diagnose hydrocephalus (n=16, 50%), followed by failure to treat and failure to recognize EVD or shunt malfunction (n=7,21.9%, respectively). Since failing to timely diagnose hydrocephalus in patients can result in serious consequences, it naturally follows that malpractice litigation related to a failed diagnosis of this condition would be common. Interestingly, although failure to diagnose was the main reason for litigation, jury verdicts ruled equally in favor of plaintiffs versus defendants in cases where this was the main cause for prosecution. However, given the high rates of shunt placement in the management of hydrocephalus and the ensuing shunt malfunctions that often develop, it is surprising that more cases did not list a surgical or post-surgical complication as a reason for litigation. Shunt infection, malfunction, and occlusion are all prevalent issues that may arise after surgery. As a result of these complications, patients tend to require shunt revision surgeries at an exceedingly high rate, with one study reporting that over 80% of patients need at least one revision during their lifetime [10]. Furthermore, techniques to diagnose shunt failure have not shown significant recent improvements. Neuroimaging remains a first line diagnostic tool to identify shunt malfunction, however, the results of such studies do not always accurately reflect the clinical scenario since normal ventricular size cannot reliably be used to rule out shunt failure [11]. Other methods, such as CSF dynamic testing or ultrasonic transit time flow sensors, have limited use as they are either invasive or not widely used in the clinical setting [12, 13]. Therefore, it would be expected for more malpractice cases regarding the treatment of hydrocephalus be related to shunt malfunction in gland failure to diagnose this condition than was observed in this study.
While the range of symptoms of those with hydrocephalus may be variable, some of the most frequently cited include headache, nausea, vomiting, and behavioral changes, such as lethargy [14]. These symptoms are in line with the results of our study, which report headache (n = 16, 50%) and nausea and/or vomiting (n = 9, 28.1%) as the two most reported preoperative claims. As a result of the increased intracranial pressure that hydrocephalus imposes on the brain due to the expanding ventricular system, failing to diagnose and ultimately treat this condition can result in devastating consequences. Death, which was the third most cited plaintiff complaint prior to surgical intervention, can ensue following the herniation of brain tissue in the setting of increased intracranial pressure. This may in part explain why failure to diagnose hydrocephalus was the most common reason for litigation as lack of appropriate treatment to relieve elevated pressure within the brain can lead to permanent damage to the brain parenchyma.
The most frequently sued physician specialties in this study were neurosurgery (n = 7, 21.9%), emergency medicine (n = 7, 21.9%), and neurology (n = 5, 15.6%). Given the involvement that neurosurgeons have with the treatment of hydrocephalus and their direct management of cases via surgical intervention, it is not unexpected that they are the most cited medical specialty. However, it is important to observe the role of emergency medicine physicians and neurologists in diagnosing patients who are initially presenting with symptoms of this disorder. Emergency medicine physicians, in particular, are often the first to see patients in acute situations, while neurologists are likely to encounter a large number of patients presenting with signs of normal pressure hydrocephalus in the outpatient setting. This may explain why neurologists were reported to have the highest payout compared to the other defendant specialties cited in this study. Given that failure to diagnose hydrocephalus was the most common inciting factor for litigation, it highlights the need for heightened awareness of the signs of hydrocephalus in emergency and outpatient settings.
In analyzing the demographic information related to hydrocephalus litigation, a wide geographic distribution of cases was observed in this study. Overall, states within the northeast were representative of the largest number of cases. Among individual states, California (n = 7, 21.9%), Texas (n = 4, 12.5%) and New York (n = 3, 9.4%) were the most frequently listed for litigation. Given that these states are among the 4 most populous states in the country, it is not surprising that they would have the highest rates of malpractice [15]. Despite the greater number of total cases observed in California and New York, however, there was a significant difference in the ruling of court cases between these two states, with juries more likely to rule in favor of defendants in California, while those in New York were more likely to rule in favor of plaintiffs. Additionally, it is interesting to note that Florida, despite being the 3rd most populated state in the nation, only listed 2 cases related to hydrocephalus malpractice. While it is not entirely clear why this may be the case, varying state laws and limitations on the ability of plaintiffs to pursue legal claims via tort reform may explain the higher levels of prosecution observed in the northeast [16].
The majority of cases in this study reported a jury verdict in favor of the defendant (n = 16, 50%), rather than the plaintiff (n = 11, 34.3%). This is comparable to previous malpractice analyses related to the management of various neurological conditions that listed a defendant over a plaintiff verdict in the majority of cases [17-20]. For cases that resulted in a plaintiff verdict, the average payment was $2,030,578.18, substantially more than the average cost of a settlement at $298,333.33. While this is in contrast to previous legal studies which have found that, in general, settlements often offer larger payouts to plaintiffs than jury verdicts, many medical malpractice studies have found settlements to be favorable for physicians with lower payout costs than jury verdicts [17, 18, 21, 22].
Although the Westlaw database provides useful information with regards to medical malpractice cases, there are some limitations to utilizing this method for legal analyses. One such limitation is that due to the administrative and legal nature of this database, it may lack specificity regarding the medical details of each case. Another potential drawback relates to the use of search terms in identifying relevant cases, as some may have used descriptive terminology of plaintiffs medical history rather than the keywords utilized to query the database. This may have resulted in the limited sample size of the current study. Additionally, cases that reached a settlement prior to being formally entered into the judicial system were not included in our analyses.
Conclusion
This study presents a 32-year analysis of cases related to the medical management of adult hydrocephalus in the United States. Failure to diagnose hydrocephalus was the most common reason for litigation, while a surgical complication was among the least cited reason for prosecution. Half of cases returned a verdict in favor of the defendant. The majority of cases named a hospital, medical center, or healthcare system as a defendant, with the most frequently named medical specialists being neurosurgery and emergency medicine. The cases with the highest average payouts were those that listed a hospital or neurologist as a defendant (for specialties listed in at least 2 cases). Cases ending in a settlement had a lower average payout compared to cases that went to trial and received a jury verdict in favor of the plaintiff. Through the analysis of malpractice related to the management of hydrocephalus, we hope to increase awareness around which factors serve as the most common reasons for litigation and how these factors may lead to unfavorable legal outcomes.
Declarations of interest
none
Funding
none
References
- Schaffer AC, Jena AB, Seabury SA, Singh H, Chalasani V, et al. (2017) Rates and characteristics of paid malpractice claims among US physicians by specialty, 1992-2014. JAMA internal medicine 177: 710-718.
- Jena AB, Seabury S, Lakdawalla D, Chandra A (2011) Malpractice risk according to physician specialty. New England Journal of Medicine 365: 629-636.
- Hochstetler A, Raskin J, Blazer-Yost BL (2022) Hydrocephalus: historical analysis and considerations for treatment. Eur J Med Res 27: 168.
- Rekate HL (2009) A contemporary definition and classification of hydrocephalus. Semin Pediatr Neurol 16: 9-15.
- Isaacs AM, Riva-Cambrin J, Yavin D, Hockely A, Pringsheim TM, et al. (2018) Age-specific global epidemiology of hydrocephalus: Systematic review, metanalysis and global birth surveillance. PLoS One 13: 0204926.
- Kirkpatrick M, Engleman H, Minns RA (1989) Symptoms and signs of progressive hydrocephalus. Archives of Disease in Childhood 64: 124-128.
- Maller VV, Gray RI (2016) Noncommunicating hydrocephalus. Seminars in Ultrasound, CT and MRI 37: 109-11.
- Stagno V, Navarrete EA, Mirone G, Esposito F (2013) Management of hydrocephalus around the world. World neurosurgery 79: 17-20.
- Merkler AE, Chang J, Parker WE, Murthy SB, Kamel H (2017) The Rate of Complications after Ventriculoperitoneal Shunt Surgery. World Neurosurg 98: 654-658.
- Mitchell KAS, Zelko I, Shay T, Horen S, Williams A, et al. (2021) The Impact of Hydrocephalus Shunt Devices on Quality of Life. Journal of Craniofacial Surgery 32: 1746-1750.
- Winston KR, Lopez JA, Freeman J (2006) CSF Shunt Failure with Stable Normal Ventricular Size. Pediatric Neurosurgery 42: 151-155.
- Weerakkody RA, Czosnyka M, Schuhmann MU, Schmidt E, Keong N, et al. (2011) Clinical assessment of cerebrospinal fluid dynamics in hydrocephalus. Guide to interpretation based on observational study. Acta Neurologica Scandinavica 124: 85-98.
- Pennell T, Yi JL, Kaufman BA, Krishnamurthy S (2016) Noninvasive measurement of cerebrospinal fluid flow using an ultrasonic transit time flow sensor: a preliminary study. Journal of Neurosurgery: Pediatrics 17: 270-277.
- Koleva M, De Jesus O (2022) Hydrocephalus. StatPearls Publishing, Florida, USA.
- Bureau USC (2023) State Population Totals and Components of Change: 2020-2022. Bureau USC, USA.
- Deng Y, Zanjani G (2018) What drives tort reform legislation? An analysis of state decisions to restrict liability torts. Journal of Risk and Insurance 85: 959-991.
- Bader ER, Boyke A, Alvi MA, Sethi A, Funari A, et al. (2021) Medical Malpractice and Vestibular Schwannomas: A Nationwide Review. World Neurosurgery 150: 714-726.
- Boyke AE, Bader ER, Naidu I, Lam S, Alvi MA, et al. (2020) Medical malpractice and meningiomas: an analysis of 47 cases. Neurosurgical focus 49: 22.
- Kessler RA, Benzil DL, Loewenstern J, Chen S, Bhammar A, et al. (2019) Malpractice litigation in brain tumor surgery: a 31-year analysis of causative factors in the United States from the Westlaw database. World Neurosurgery 122: 1570-1577.
- Pecorari IL, Flaquer I, Bergemann R, Funari A, Alvi MA, et al. (2023) Medical malpractice and intracranial hemorrhages in the US: An analysis of 121 cases over 35 years. Heliyon 9: 14885.
- Boyke AE, Naidu I, Lam S, Alvi MA, Bader ER, et al. (2021) Medical malpractice and trigeminal neuralgia: an analysis of 49 cases. Journal of Oral and Maxillofacial Surgery 79: 1-1026.
- Kiser RL, Asher MA, McShane BB (2008) Let's not make a deal: an empirical study of decision making in unsuccessful settlement negotiations. Journal of Empirical Legal Studies 5: 551-591.
Citation: Pecorari IL, Flaques I, Bergemann R, Alvi MA, Agarwal V (2023) Medical Malpractice in Adult Hydrocephalus: An Analysis of 32 Cases. Archiv Surg S Educ 5: 047.
Copyright: © 2023 Isabella L. Pecorari, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

