
Medical Suspicion Overcomes Misleading Clinical and Laboratory Aspects of Genitourinary Tuberculosis
*Corresponding Author(s):
Florencia NeffaDepartment Of Urology, Hospital De Clinicals, Montevideo, Uruguay
Tel:+598 99930860,
Fax:+598 224873405
Email:floneffa@gmail.com
Abstract
Introduction: Tuberculosis is accountable for 2 billion people infected from Mycobacterium tuberculosis worldwide; ultimately 5 to 10% will get sick. Gold standard treatment is effective for the vast majority of the affected population. However, it remains an unresolved public health problem.
Case presentation: In this case report the authors portray the long journey of an immune competent, healthy, young patient towards genitourinary tuberculosis detection.
Conclusion: Tuberculosis is still to this day a concern of public health. Pulmonary as well as extra-pulmonary manifestations could develop in a misleading manner delaying best course of treatment. Specific and effective medication is available, which only evidences the fact that we are failing to diagnose properly and timely this deceiving disease.
Keywords
Genitourinary; Tuberculosis; Mycobacterium tuberculosis
KEY NOTE MESSAGE
Fast and proper diagnosis of tuberculosis is of the essence to provide an optimal treatment and clinical care to the patient. Consideration of Genitourinary tuberculosis in patients from endemic areas who present with urinary symptoms, negative urine cultures, abnormal urinary tract imaging and in whom treatment for common urinary infections have failed, is clearly necessary. Even though medical therapy is currently available, delayed diagnosis could lead to chronic and/or fatal consequences.
INTRODUCTION
Tuberculosis (TB) is a major global cause of death, being a public health concern worldwide. Around one third of the world population is infected with Mycobacterium Tuberculosis (MBT), whereas these have a 5 to 15% lifetime risk of getting sick sick [1]. An alarming 95% is concentrated in developing countries [2]. According to 2012 ciphers, Asia concentrates up to 60% of all new cases per year [1]. Albeit specific standardized treatment is effective for most part of the affected population, it still remains an unresolved public health problem [3]. An estimated 1.3 million people died from TB in 2017. Out of the 10 million people who developed the illness 9% were HIV-positive. Immunological integrity status is key to successfully overcome the disease, being HIV carriers much more expose to disease and death [4]. Uruguay is denominated the Latin-American country with the lowest disease prevalence, detecting 2,76 deaths per 100.000 habitants in 2016 [5].
Extrapulmonary involvement can be expected in 10 to 42% of cases. The order of organ affection being: Pleural, lymph node, and renal TB (3 to 21%) [6]. Urogenital TB (UGTB) is a much more silent ailment, mostly overlooked compared to pulmonary TB, although being the second most common form of TB in countries with a severe epidemic situation and the third most common form in regions with a low incidence of TB.
The kidneys are primary targets due to hematogenous spread of the bacilli, mainly derived from prime pulmonary infection, with a 3 to 10-year dilatation, according to the host immune system integrity. Nonspecific clinical manifestations are the rule, often resulting in delayed diagnosis and ominous prognosis [7]. Sub diagnosis of UGTB arises many inconsistencies regarding different nomenclature, disease classification, therapeutic strategies and management.
The present publication describes a case of GUTB in a young, immuno-proficient man, with no personal or environmental history of TB, with severe renal function loss and urinary tract obstruction symptoms, portraying the importance of acknowledging the misleading nature of clinical manifestations and naïve background.
MATERIALS AND METHODS
The patient is a healthy 34-year-old male, with no personal or familial history of TB or HIV, nor previous contact with known TB individuals. He first presented at 31 years of age with symptomatic elevated blood pressure ciphers treated successfully with standard medication. Subsequent controls over a 3-year period of time showed a marked increase in creatinine levels. Recent episodes of persistent fever and dysuria in an acute renal failure context, triggered a full medical, urological and nephrological evaluation. Clinical examination was consistent with: Lumbar bilateral pain, enlarged prostate in rectal palpation and multiple urethral strictures. Computed tomography of chest-abdomen and pelvis without contrast was done. Figure 1 laboratory tests showed the following results: hemoglobin 8,4 mg/dL; white blood count 12,690 mg/mm3; creatinine 6.08 mg/ dL (estimated glomerular filtration rate (GFR) = 18,16 mL/ min based on Cockroft-Gault formula); urea 133 mg/dL; the patient tested negative for hepatitis B, hepatitis C, Human Immune Deficiency Virus (HIV) infection and syphilis. Urinalysis showed the following results: pH 5.5, leukocyturia 50/high power field and hematuria 15/high power field. One hemo culture and three consecutive urine cultures were performed not yielding any positive findings. Urine and pulmonary bacilloscopys were negative for Mycoplasma TB (Figure 1).
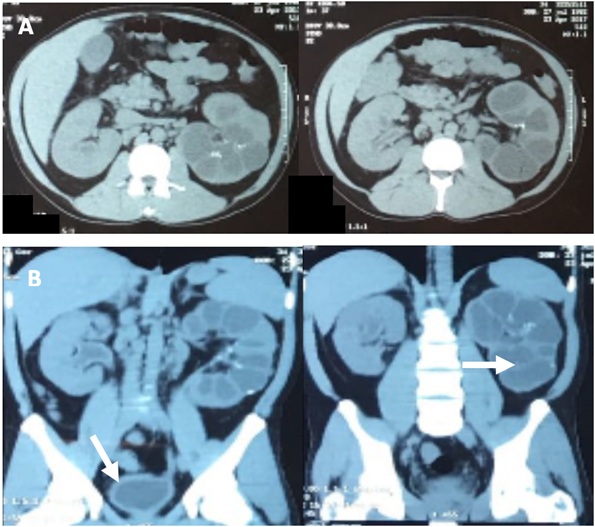 Figure 1: A) Sagittal view of abdominal computer tomography. B) Coronal view of abdómino-pelvis computer tomography.
Figure 1: A) Sagittal view of abdominal computer tomography. B) Coronal view of abdómino-pelvis computer tomography.
Arrows pointing at pyelocaliceal dilation of RK; severe hydronefrosis of LK; and thick bladder walls.
Patient manifested rapid clinical deterioration with increasing creatinine and azotemia ciphers and infection parameters, combined with high fever, pyuria and right flank pain. An anesthetized exploratory urethro-cystoscopy was performed, observing an indurated urethra with diminished caliber, a poor capacity bladder with inflammatory aspect and a whitish substance covering almost all vesical surface. Sample biopsy from bladder wall and pyuric urine from left urether were taken for analytic purposes. Urine derivation was performed by placing a uretheral and vesical catheter. The pathology report informed a granulomatous necrotic process of the bladder with a negative Ziehl Nielsen test result. The urine bacilloscopy was finally positive for Mycobacterium TB. A posterior urine culture using the Lowenstein-Jensen medium isolated M. tuberculosis.
Based on these results, the patient began a 6-month course of rifampin, isoniazid, pyrazinamide and ethambutol according to World Health Organization current guidelines. According to the classification of UGTB8 some of the complications already observed were: unilateral kidney loss, right polycavernous kidney, hydronefrosis, shruncken bladder, renal failure, urethral stricture and clinical prostate TB. Patient is now in a pre-hemodialysis list, with a GFR of 28 ml/seg despite adequate treatment.
DISCUSSION
As stated by the World Health Organization (WHO) in 2014, over 30% of the worldwide population are infected by Mycobacterium tuberculosis, and these carry an accumulated risk of 10% of suffering from Tuberculosis throughout their lifetime [8]. This disease is the second most frequent cause of death due to a single infectious microorganism8. Most of the focus is put into pulmonary TB, however, GUTB is a frequent manifestation of Mycobacterium tuberculosis infection and due to misleading symptoms causing late diagnosis, the prognosis is often compromise, in spite of having an adequate course of treatment.
Regarding GUTB, there are no specific clinical signs a practitioner could rely to diagnose it. When considering this pathology, it includes a wide spectrum of symptoms among different patients, but most importantly between the various forms and stages of the disease, making it impossible to apply a standard unified approach of diagnosis and treatment [8]. In patients from endemic areas who present with: urinary symptoms, negative urine cultures, abnormal urinary tract imaging and in whom treatment for common urinary infections have failed, a high degree of clinical suspicion is clearly necessary. Delayed diagnosis is detrimental, leading to chronic and fatal consequences [9].
CONCLUSION
Tuberculosis is an ancient disease which still remains in a latent form in a great part of the world’s development countries population, affecting the most vulnerable individuals, generating millions of deaths. Both pulmonary and extra-pulmonary manifestations could develop in a misleading manner, causing late diagnosis and delaying best course of treatment. Specific and effective medication is available, which only adds concern to the fact that we are failing in recognizing properly and timely this deceiving disease. We portrayed the story of one immune proficient, healthy, young patient through his 3-year journey towards GUTB detection.
REFERENCES
- WHO (2018) Tuberculosis. WHO, Geneva, Switzerland.
- Kulchavenya E (2013) Best practice in the diagnosis and management of urogenital tuberculosis. Ther Adv Urol 5: 143-151.
- Barry C, Konstantinos A; National Tuberculosis Advisory Committee (2009) Tuberculosis notifications in Australia, 2007. Commun Dis Intell Q Rep 33: 304-315.
- World Health Organization (2014) Global Tuberculosis report 2014. World Health Organization, Geneva, Switzerland.
- Pan American Health Organization (2016) Situation of tuberculosis in Uruguay. Pan American Health Organization, Uruguay.
- Gibson MS, Puckett ML, Shelly ME (2004) Renal tuberculosis. Radiographics 24: 251-256.
- Abbara A, Davidson RN (2011) Etiology and management of genitourinary tuberculosis. Nat Rev Urol. 8: 678-688.
- Kulchavenya E (2014) Urogenital tuberculosis: Definition and classification. Ther Adv Infect Dis 2: 117-122.
- Zarrabi AD, Heyns CF (2009) Clinical Features of Confirmed Versus Suspected Urogenital Tuberculosis in Region With Extremely High Prevalence of Pulmonary Tuberculosis. Urology 74: 41- 45.
Citation: Neffa F, Galvan A, Huelmo S, Despaux A, Montana E, et al. (2019) Medical Suspicion Overcomes Misleading Clinical and Laboratory Aspects of Genitourinary Tuberculosis. J Clin Stud Med Case Rep 6: 075.
Copyright: © 2019 Florencia Neffa, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

