
Medical Termination of Pregnancy: Follow up Protocol, Adherence Rates, and Predictors of Success
*Corresponding Author(s):
Aya LewkowiczDepartment Of Obstetrics And Gynecology, Hadassah Hebrew University Medical Center, Ein Kerem, POB 12000, Jerusalem, Israel
Tel:+972 508573729,
Fax:+972 29947762
Email:aya.lewkowicz@gmail.com
Abstract
Objectives: Medical Termination of Pregnancy (TOP) is a safe and effective method for women with unwanted pregnancies. Heterogeneity exists in the follow up protocols and in the definition of complete abortion following treatment. The purpose of this study was to evaluate efficacy and adherence to the follow up protocol and identify clinical and sonographic predictors of medical TOP success.
Study design: This was a retrospective study evaluating the institutional follow up protocol for women who had undergone medical TOP with mifepristone and misoprostol. We evaluated demographic, clinical and sonographic parameters. We conducted uni- and multi-variable analyses to identify predictors of failure.
Results: A total of 346 women were evaluated, of which 12% required additional intervention and were considered as failure of procedure. Only 44% adhered to the full follow up protocol. Women in the failure group exhibited higher rates of vaginal bleeding (38.9% vs.6.3%, p<0.001), fetuses with or without a pulse by ultrasound (9.6% vs 0.0%, p<0.001) and presence of Doppler flow (80.9% vs. 1.1%, p<0.001) at the premenstrual follow-up. At the second visit, patients again exhibited higher rates of vaginal bleeding, Doppler flow and a thicker endometrium. In the multivariable regression model, vaginal bleeding, endometrial thickness, and Doppler flow were independently associated with procedure failure, while controlling for maternal age, gravidity and gestational age (aOR=2.9, p<0.003, aOR=1.2 for any additional mm, p<0.001, and aOR=3.3, respectively, p<0.001).
Conclusion: Adherence to the full protocol is low. Vaginal bleeding, thicker endometrium and presence of uterine cavity Doppler flow are independently associated with procedure failure.
Implication statement: Medical termination is becoming more widely available. It is essential to have consistent and implementable follow up protocols to ensure safety and adherence. Our study aims to identify which factors will predict the need for intervention.
Keywords
Dilation and curettage; Doppler; Hysteroscopy; Mifegyne; Misoprostol; Ultrasound; Vaginal bleeding
INTRODUCTION
Women around the world elect to terminate their pregnancies (termination of pregnancy-TOP) for various reasons, often because the pregnancies endanger their health or wellbeing. In the past, the only possible way to terminate a pregnancy was with a surgical procedure, namely dilation and curettage. Since the beginning of the 21st century, the possibility of terminating a pregnancy thorough a medical route has become available and has now become an effective and practical alternative. In 2000, the Food and Drug Administration (FDA) first approved the use of mifepristone, a progesterone antagonist for use in the medical termination of pregnancy. According to the recommendations from 2011 [1], a 600 Mg dose of mifepristone is followed up 2 days later by 400 mcg of misoprostol, a prostaglandin that causes uterine contraction and cervical dilation and leads to evacuation of the pregnancy.
One of the main challenges that arise from published studies evaluating medical termination of pregnancy is that the optimal follow up policy is unknown and varies significantly between institutions. Moreover, the definition of success, namely whether the woman has achieved complete abortion (and does not require any additional intervention) is inconsistent. The label for mifepristone, which was issued by the manufacturer in 2011, reads: “Patients should follow-up with their healthcare provider approximately 7 to 14 days after the administration of MIFEPREX. This assessment is very important to confirm that complete termination of pregnancy has occurred and to evaluate the degree of bleeding…The existence of debris in the uterus (e.g., if seen on ultrasonography) following the treatment procedure will not necessarily require surgery for its removal” [1].
In practice, there is great heterogeneity in follow up protocols for women who have undergone medical termination of pregnancy between countries and institutions [2-6]. Even more importantly, there is no universal definition for complete abortion, whether sonographic, clinical, or hCG level based, nor is there a consensus as to which patients require additional dosages of misoprostol versus surgical intervention. At our institution, we have offered patients the option to undergo medical TOP since 2006. The purpose of this study was to determine patient adherence rates to our local stringent follow up protocol and to isolate clinical or sonographic characteristics predictive of failure. Such predictors may determine the need for further follow up.
MATERIALS AND METHODS
This was a retrospective database study conducted at Hadassah Mount Scopus Hospital in Jerusalem, Israel. We received approval from our Institutional Review Board. At our institution, the option to undergo medical termination has been available since 2006. We used computerized files and were able obtain information on all patients who underwent medical termination between the years 2011-2014 at our institution. During the period of this study, we offered the procedure up to 56 days since the previous LMP. Eligible patients who opted for medical termination, received the standard protocol which included mifepristone (600 mg) and, after 48 hours, misoprostol (800 mcg). Women were then scheduled for a follow up visit 14 days later. At the follow up visit, bleeding and pain are discussed and an Ultrasound (US) examination is performed. The physician who saw the patient at the follow up visit decided whether the patient had a complete abortion, required immediate intervention, or should be referred for additional follow up. If the endometrium was thin, bleeding had stopped and no Doppler flow was detected, the patient was discharged. In intermediate cases, patients were asked to come for an additional follow up visit following their next menstrual period. If a fetus or a gestational sac were still demonstrated or if the endometrium thickness was measured to be over 10 mm, especially if Doppler flow was present, the patient was referred for intervention. The same parameters were evaluated at the second visit.
Potential interventions included a second dose of misoprostol, Dilatation and Curettage (D&C), or hysteroscopy. We recorded demographic criteria including patient age, gravidity, parity, gestational week, obstetrical history, modes of previous deliveries, and history of previous missed abortion or medical termination of pregnancy. At the initial follow-up we obtained data regarding the presence of vaginal bleeding as well as sonographic criteria including endometrial thickness and presence of Doppler flow. We defined complete abortion according to the decision made by the attending physician. If the clinician decided to refer the patient for a second follow up (after the subsequent menstrual period), we recorded the same clinical and US parameters at the second visit. For the purpose of this study, we defined “treatment failure” as the need for any additional intervention; either D&C or hysteroscopy. Patients and the public were not involved in the design of this study.
Statistical analysis
We compared different demographic, clinical and sonographic characteristics of successful and unsuccessful cases. As mentioned above, any need for a surgical intervention was defined as medical TOP failure. We have performed all analyses in two stages: In the first set, we included all women lost to follow up as part of the success group - out of the assumption that they did not return because they were asymptomatic. In the second set of analyses (i.e., - sensitivity analyses), all “loss of follow up” cases were excluded. We compared women with a known outcome of complete abortion to those who required any additional surgical intervention.
Statistical analysis was performed using SPSS software Version 21 (SPSS, Chicago, IL). Quantitative variables were compared using the Student T-test in cases of normal distribution and the Mann-Whitney test in cases of non-normal distribution. Categorical variables are shown in counts and percentages and the differences were assessed by Chi-Square test (or Fisher Exact test as appropriate). Multivariable logistic regression models were constructed to study the association and prediction of demographic sonographic and clinical findings on medical termination failure, while controlling for potential confounders. Statistical significance was set at p < 0.05.
RESULTS
A total of 346 women were included in the study. Patient adherence to the follow up protocol and failure rates is detailed in figure 1.
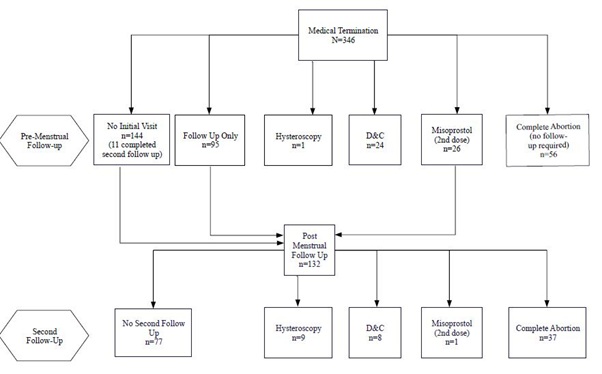 Figure 1: Patient adherence to the follow up protocol and failure rates.
Figure 1: Patient adherence to the follow up protocol and failure rates.
The initial follow up visit was attended by 58% (202) of the participants, while 38% (133) were lost to follow up (Figure 1). Of patients attending the first follow-up visit, 28% (56) had a complete abortion and 47% (95) were asked to come for a second follow up visit after their next menstrual period. In the remaining cases (51), in which the clinician decided an immediate intervention is required: 47% (24) underwent D&C, 2% (1) underwent hysteroscopy and 51% (26) received a second dose of misoprostol (400 mcg) and were asked to come for a second follow up visit.
Of the 121 patients who were asked to come for a second follow up visit (26 of which were following a second dose of misoprostol), 36% (44 women) actually attended.
Table 1 depicts demographic characteristics of the study participants while comparing successful to unsuccessful cases. Older maternal age, higher parity, and a more advanced gestational age were significantly more common in the treatment failure group.
|
|
Unsuccessful Medical Termination N=43 |
Successful Medical Termination N=303 |
Total N=346 |
p-value |
|
General Characteristics |
||||
|
Maternal age (Years) |
30 ± 7.6 |
25.9 ± 7.8 |
26.5 ± 7.9 |
0.001 |
|
Obstetrical Characteristics |
||||
|
Gravidity |
3.2 ± 1.9 |
2.2 ± 2.0 |
2.4 ± 2.0 |
<0.001 |
|
Parity |
1.7 ± 1.6 |
0.9 ± 1.6 |
1.0 ± 1.6 |
<0.001 |
|
Gestational age |
5.8 ± 0.7 |
5.6 ± 0.7 |
5.6 ± 0.7 |
0.023 |
|
Previous cesarean section |
23.3% (10) |
9.6% (29) |
11.3% (39) |
0.017 |
|
Previous NSVD |
48.8% (21) |
26.4% (80) |
29.2% (101) |
0.002 |
|
Previous medical Top |
11.6% (5) |
9.2% (28) |
9.5% (33) |
0.582 |
|
Previous missed abortion |
18.6% (8) |
10.9% (33) |
11.8% (41) |
0.143 |
Table 1: Demographic and obstetrical characteristics of patients who underwent medical termination of pregnancy.
Data are presented as % (n) or mean ± SD; Significance for difference was measured using Chi squared and Mann-Whitney test; NSVD: Normal Spontaneous Vaginal Delivery; Top: Termination for Pregnancy.
In table 2, clinical and sonographic parameters obtained at the initial follow up visit and in the post-menstrual visit (if required), were compared. In the initial visit, presence of a fetus with a pulse was significantly more common in the treatment failure group. Additionally, and in both visits, the presence of vaginal bleeding, Doppler flow within the uterine cavity, and a thicker endometrium were significantly more common in the treatment failure group (Table 2).
|
|
Unsuccessful Medical Termination |
Successful Medical Termination |
Total |
p-value |
|
Premenstrual Follow-Up (N=346) |
N=157 |
N=189 |
N=346 |
|
|
Vaginal bleeding |
38.9% (61) |
6.3% (12) |
21.1% (73) |
<0.001 |
|
Fetus with or without pulse |
9.6% (15) |
0.0% (0) |
4.3% (15) |
<0.001 |
|
Endometrial thickness (mm) |
13.6 ± 5.6 |
8.5 ± 3.3 |
12.0 ± 5.5 |
<0.001 |
|
Endometrial thickness>15 mm |
26.1% (41) |
3.2% (6) |
13.6% (47) |
<0.001 |
|
Endometrial thickness>10 mm |
64.3% (101) |
8.5% (16) |
33.8% (117) |
<0.001 |
|
Doppler flow at US |
80.9% (127) |
1.1% (2) |
37.3% (129) |
<0.001 |
|
Second Follow-Up (N=265) |
N=18 |
N=247 |
N=265 |
|
|
Vaginal bleeding |
16.7% (3) |
0.8% (2) |
1.9% (5) |
0.002 |
|
Endometrial thickness (mm) |
12.7 ± 6.5 |
7.4 ± 2.8 |
8.7 ± 4.6 |
0.001 |
|
Endometrial thickness>15 mm |
22.2% (4) |
0.8% (2) |
2.3% (6) |
<0.001 |
|
Endometrial thickness>10 mm |
44.4% (8) |
3.2% (8) |
6.0% (16) |
<0.001 |
|
Doppler flow at US |
72.2% (13) |
3.6% (9) |
8.3% (22) |
<0.001 |
Table 2: Comparision of clinical and sonographic charecteristics of patinets who underwent medical termination of pregnancy.
Data are presented as % (n) or mean ± SD; Significance for difference was measured using Chi squared and Mann-Whitney test; US: Ultrasound.
Premenstrual Follow-Up occurred 2 weeks after initial treatment. Possible outcomes include complete abortion, lost to follow up, need additional follow up need or need for immediate intervention (misoprostol, D&C or hysteroscopy).
Second Follow-Up occurred 4-6 weeks after initial treatment; we excluded patients with complete abortion or those who required hysteroscopy or D&C at the premenstrual visit.
A sensitivity analysis was performed on confirmed cases only (excluding loss of follow up cases, namely 93 with complete abortion and 42 failures). Again, older maternal age (30.3±7.6 vs. 24.2±6.9, p<0.001), higher gravidity (3.2±1.9 vs. 1.5±1.3, p<0.001) and more advanced gestational age (5.8±0.7 vs. 5.5±0.8, p<0.015) were associated with treatment failure. Treatment failure was significantly associated with: vaginal bleeding (first visit 41.8% vs. 21.4% p=0.007, second visit 16.7% vs. 0%, p=0.029), presence of fetus with or without a pulse (10% vs. 0%, p=0.013) thickened endometrium (first visit 13.6 vs. 8.5, p<0.01, second visit 12.7 vs. 7.1, p=0.001) and presence of Doppler flow (first visit 87% vs. 3.6%, p<0.001, second visit 72.2% vs. 13.2%, p<0.001).
Several multi-variable regression analyses were conducted in order to assess the independent association between different clinical and sonographic predictors and treatment failure, while controlling for potential confounders. These included maternal age, gravidity, and gestational age. Table 3 confirmed that the presence of vaginal bleeding (OR 2.9, 95%CI 1.4-5.9, p=0.003), endometrial thickness as a continuous parameter (OR 1.2, CI 1.1-1.3, p=0.01) and greater than 10 or 15 mm (OR 2.1, p=0.027 and OR=4.4, p<0.001, respectively), presence of a fetus (with or without a pulse OR=231.1, p<0.00), and presence of Doppler flow (OR 3.3, CI 1.7-6.6, p=0.001), were each independently and significantly associated with treatment failure. Gravidity was not found to be an independent predictor of treatment failure.
|
|
Adjusted OR |
95% CI of OR |
p value |
|
Vaginal bleeding* |
2.9 |
1.4-5.9 |
0.003 |
|
Fetus with or without pulse* |
231.1 |
26.3-2029.7 |
<0.001 |
|
Doppler flow* |
3.3 |
1.7-6.6 |
0.001 |
|
Endometrial thickness* |
1.2 |
1.1-1.3 |
<0.001 |
|
Endometrial thickness>15 mm* |
4.4 |
2.0-9.3 |
<0.001 |
|
Endometrial thickness>10 mm* |
2.1 |
1.1-4.1 |
0.027 |
|
Gravidity** |
0.9 |
06.-1.3 |
0.651 |
Table 3: Multivariate analyses for demographic and clinical findings premenstrual follow-up: results from 7 multivariable models.
Data is presented using logistic regression models.
*Controlled for maternal age, gravity, gestational age.
** Controlled for maternal age, vaginal bleeding, endometrial width, Doppler flow.
In the sensitivity analysis of confirmed cases only, the regression demonstrated endometrial thickness (OR 1.3, CI 1.1-1.5, p<0.001) to be a significant predictor of treatment failure. Presence of Doppler flow within the uterine cavity approached significance (OR 2.3 CI 0.9-5.4 p=0.056).
DISCUSSION
In this retrospective cohort study of patients who underwent medical termination of pregnancy, designed to ascertain follow up adherence and possible predictors for treatment failure, we found very low adherence rates, with only 63% of patients coming in for an initial follow up visit and only 36% coming in for a second follow up. The success rate was 82%, and 62% after excluding loss of follow up cases. Persistent vaginal bleeding, a thickened endometrium, and presence of Doppler flow independently predicted treatment failure and a need for an additional medical or surgical intervention. Older maternal age, higher parity, and a more advanced gestational age were significantly more common in the women who required additional intervention.
These rates are substantially lower than those reported in the literature, which are reported to be above 95%. The most probable explanation for this discrepancy is that there is significant heterogeneity in the definition of a successful treatment. Our institution considers sonographic assessment a key feature in the follow up protocol. While this practice reduces the likelihood of failing to diagnose an ongoing pregnancy, it probably increases the likelihood of over-diagnosis and the subsequent potential for over-treatment. Although initially we thought that higher parity (more common in our population than elsewhere in Western Europe and North America) possibly elevated treatment failure rates, gravidity was not found to be independently associated with failure (Table 3). At a more advanced gestational age, the fetus is larger, and the precursor of the placenta is likely more adherent to the uterus; these features may offer an explanation as to higher rates of failure at later stages of the pregnancy. On the other hand, we expected that women with higher parity would have lower failure rates but found the opposite. This finding requires further exploration in future studies. From a clinical perspective, we saw the low adherence rate as a mostly positive finding since it, most likely, meant that our patients felt well enough that they did not even deem it necessary to come to their follow up appointment. In the future, we plan to conduct a prospective study that would include telephone conversation with participants who did not come to their follow up appointments to better understand their considerations.
Different treatment protocols of medical pregnancy termination have been widely investigated in the published literature, but our study adds a unique clinical angle; due to the routine use of sonographic parameters at every follow up visit, we were able to evaluate the utility of sonographic prediction of treatment failure early on in the process. While previous authors have not found endometrial thickness to be significant [6], our results show that both the thickness (over 10 mm and more so over 15 mm) as well as the presence of Doppler flow are independently predictive of treatment failure. We are not aware of other published data focused on Doppler flow measurements in this context. Length of follow-up also distinguishes our protocol from others. On one hand - our strict policy lowers the chances for a missed case of an on-going pregnancy. On the other hand, we realize adherence rates are low, and the cost (in terms of time and expense) may be unjustified.
CONCLUSION
Although the study is limited by its retrospective design and relatively small number of patients, we feel we have reached some important insights including a true representation of the low follow up adherence rates and the predictive potential of different clinical and sonographic parameters. In light of our findings, and especially the low adherence to the follow-up protocol, we believe that a less stringent follow up protocol will probably yield similar outcomes in terms of success and safety. Our insights are in line with others: In 2016, the FDA changed the prescribing instructions for mifepristone so that they no longer require an in-person visit following treatment [7]. Moreover, in 2018 the World Health Organization changed its guidelines and no longer recommends the need for a follow up appointment unless the patient is still experiencing bleeding or symptoms of pregnancy [8]. Not only follow up recommendations have changed; recent studies from both Kazakhstan and the US have shown that women can safely administer both medications at home in a safe and efficacious manner and that most participants found this to be more comfortable [9,10]. Medical termination of pregnancy is a safe and effective method to end an unwanted pregnancy and does not seem to require a strict follow up regimen or the routine use of ultrasound. It is time to adopt a less stringent protocol in the best interests of our patients. Future local protocols should consider these findings as well as patient safety and comfort, legal aspects, and cost benefit considerations.
FUNDING
This study did not receive funding.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
ETHICAL APPROVAL
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
REFERENCES
- FDA (2011) MIFEPREX® (mifepristone) Tablets, 200 mg For Oral Administration Only. FDA, Maryland, USA.
- Kulier R, Kapp N, Gülmezoglu AM, Hofmeyr GJ, Cheng L, et al. (2011) Medical methods for first trimester abortion. Cochrane Database Syst Rev 2011: CD002855.
- Bar-Hava I, Aschkenazi S, Orvieto R, Perri T, Shalev J, et al. (2001) Spectrum of normal intrauterine cavity sonographic findings after first-trimester abortion. J Ultrasound Med 20: 1277-1281.
- Wang G, Li D, Manconi F, Dong B, Zhang Y, et al. (2010) Timing and indication for curettage after medical abortion in early pregnant women with prior uterine incision. Contraception 81: 62-66.
- Gatter M, Cleland K, Nucatola DL (2015) Efficacy and safety of medical abortion using mifepristone and buccal misoprostol through 63 days. Contraception 91: 269-273.
- Reeves MF, Fox MC, Lohr PA (2009) Endometrial thickness following medical abortion is not predictive of subsequent surgical intervention. Ultrasound Obstet Gynecol 34: 104-109.
- FDA (2016) MIFEPRISTONE- mifepristone tablet. FDA, Maryland, USA.
- World Health Organization (2018) Medical Management of Abortion. WHO, Geneva, Switzerland.
- Platais I, Tsereteli T, Grebennikova G, Lotarevich T, Winikoff B (2016) Prospective study of home use of mifepristone and misoprostol for medical abortion up to 10weeks of pregnancy in Kazakhstan. Int J Gynaecol Obstet 134: 268-271.
- Chong E, Frye LJ, Castle J, Dean G, Kuehl L, et al. (2015) A prospective, non-randomized study of home use of mifepristone for medical abortion in the U.S. Contraception 92: 215-219.
Citation: Lewkowicz A, Cahen-Peretz A, Gilad R, Walfisch A (2020) Medical Termination of Pregnancy: Follow up Protocol, Adherence Rates, and Predictors of Success. J Reprod Med Gynecol Obstet 5: 064.
Copyright: © 2020 Aya Lewkowicz, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

