
Meta-analysis of Acupuncture-Related Therapy Versus Western Drug Replacement Therapy in the Treatment of Hashimoto's Thyroiditis
*Corresponding Author(s):
Weichen SiSchool Of Acupuncture-Massage And Tuina, Shanghai University Of Traditional Chinese Medicine, China
Tel:+86 15311000917,
Email:weichens14@163.com
Abstract
Objective: To systematically evaluate the improvement of symptoms and indicators in patients with Hashimoto's thyroiditis by acupuncture-related therapy and western drug replacement therapy.
Methods: A computerized search of CNKI, VIP, Wan Fang, CBM, PubMed, Cochrane and other databases was used to search for clinical randomized controlled trials that have been published on acupuncture-related therapy and western drug replacement therapy for Hashimoto's thyroiditis. The time frame for the literature search was from the creation of the database until 1 March 2021. the Cochrane Risk of Bias Assessment Form was used to assess the risk of bias in the included literature, and RevMan 5.4 software was used to conduct a meta-analysis of the included literature.
Results: A total of 7 publications involving 449 patients were included, and the results of the Meta-analysis showed that: in terms of efficiency: acupuncture-related therapy improved patients' symptoms better than western drug replacement therapy [RR=1.29, 95%CI (1.17, 1.42), P<0.001]; in terms of all indicators: improving serum TPO-Ab levels, the acupuncture-related therapy group was better than the In terms of indicators: improvement in serum TPO-Ab levels was better in the acupuncture-related therapy group than in the Western medicine substitution therapy group [SMD=-3.37, 95%CI (-3.83, -2.90) at 1 treatment frequency for 1 day], [SMD=-0.96, 95%CI (-1.31, -0.60) at 1 treatment frequency for 2 days], and improvement in serum TG-Ab levels was better in the acupuncture-related therapy group than in the Western medicine substitution therapy group [SMD=-2.86, 95%CI (-3.68, -2.03) at 1 treatment frequency for 1 day], [SMD=-0.72, 95%CI (-1.26, -0.19) at 1 treatment frequency for 2 days], improved serum FT3 levels, better in the acupuncture-related therapy group than in the western drug replacement therapy group [SMD=0.69, 95%CI (0.15,1.22)], improved serum FT4, TSH levels, and The acupuncture-related therapy group was superior to the western drug replacement therapy group.
Conclusion: Acupuncture-related therapy was superior to western drug replacement therapy in improving symptoms and indicators in patients with Hashimoto's thyroiditis. The majority of the literature, including the one on acupuncture, has methodological flaws and the level of evidence is not high, so the conclusions need to be further validated.
Keywords
Acupuncture; Alternative Therapy; Hashimoto's Thyroiditis; Meta-analysis; Moxibustion
Introduction
Hashimoto's Thyroiditis (HT) was first described by the Japanese scholar Hashimoto in 1912. It is a chronic autoimmune, aseptic inflammatory disease that uses its own thyroid tissue as the antigen [1]. Lymphocytic Thyroiditis (CLT), and chronic autoimmune thyroiditis [2,3]. Autoimmunity is the accepted cause in the medical community, but the pathogenesis is unclear and may be related to mechanisms such as oxidative stress, apoptosis, imbalance in the function of T lymphocyte subsets and associated cytokines, and micro RNA (miRNA) [4]. According to epidemiological studies, the global incidence of HT is 0.3-1.5 cases per 1000 people per year. The prevalence of positive antibody tests in women is >10% and accounts for at least 2% of clinical disease [5]. The prevalence is up to 40% in older women and 10% to 20% in men [6], while in our own country the prevalence is higher and is gradually increasing [7,8].
Modern medicine has no cure for HT. At present, the main treatment is symptomatic. In the case of normal thyroid function, observation is the mainstay; in the case of hyperthyroidism, the symptoms are mostly transient and generally do not require special management; in the case of hypothyroidism, clinical treatment is mostly with levothyroxine replacement therapy; patients with severe hypothyroidism may require lifelong thyroxine replacement therapy [9,10]. There are adverse effects and side effects such as increased hormone dependence late in the course of medication, the required dosage can increase to the point of ineffectiveness, easy relapse after discontinuation, and low thyroid function [11]. In recent years, there has been increasing research into the effects of selenium on HT, but the jury is still out on whether it can be used as a routine treatment [12]. Therefore seeking sustainable treatments for HT with high efficacy, low adverse effects and high safety, together with early and active intervention, is important for treating HT and delaying the progression of the disease [13].
According to research, acupuncture has the effect of regulating the neuroendocrine immune system and bi-directional regulation of the body's immune function, and this brings the body's immune dysfunction to a new dynamic balance while harmonizing and stabilizing the internal and external environment, thus improving the clinical symptoms of HT [11,14], and these effects have been increasingly emphasized in studies on the treatment of HT, and clinical studies on the treatment of HT are being reported [15]. Therefore, in this study, meta-analysis was used to compare the improvement of symptoms and indicators of HT patients with acupuncture-related therapies and modern medicine, which in turn can provide a reference for clinical medical decisions [16].
Data And Methods
Inclusion criteria
Combined with acupuncture-related therapies; the drugs and the dose and frequency are not limited. The duration of treatment was limited to at least 4 weeks (1 month); (4)The main outcome indicators were the rate of reduction in the Traditional Chinese Medicine Syndrome Scale (TCMSSS) score, changes in serum TSH, FT3, FT4, TPO-Ab and TG-Ab levels; (5)The clinical randomized control of acupuncture-related therapy and Clinical randomised controlled trials of modern medicine for HT, regardless of whether allocation concealment or blinding was mentioned, regardless of the time of publication and geographical area of study. Only if all five of these were met simultaneously were they included in the analysis [17,18].
Exclusion criteria
(i) Non-randomised controlled trials; (ii) Repeatedly published or unpublished literature, unavailable in full, with incorrect data or ambiguous descriptions; (iii) Treatment groups or control groups containing treatment modalities other than the inclusion criteria; (iv) Incomplete data for all outcome indicators; (v) Unclear diagnostic criteria. Those meeting any of the above were excluded.
Search strategy
Computer searches of databases such as China Knowledge Network, Vipshop, Wanfang, CBM, PubMed, and Cochrane were conducted. The time frame for the literature search was from the establishment of the database to 1 March 2021. Chinese search terms include: "acupuncture" "electro-acupuncture" "head acupuncture" "warm acupuncture" "moxibustion" "spacer moxibustion" "acupuncture therapy" "acupuncture therapy" Randomized control" "Hashimoto's thyroiditis" "autoimmune thyroiditis" "chronic lymphocytic thyroiditis" [19] English search terms include: “moxibustion”“acupuncture”“Warming needle-moxibustion”“Electroacupuncture”“Hashimoto’s thyroiditis”“chronic lymphocytic thyroiditis”“chronic autoimmune thyroiditis”.
Literature screening and data extraction
After the two research workers searched the literature individually according to the above search strategy, eliminated duplicates, checked the titles and abstracts, excluded literature that did not meet the study objectives in the initial screening, then downloaded the rest of the literature and read the full text, excluded literature that did not meet the inclusion criteria and/or met the exclusion criteria, included the rest of the literature that met the inclusion criteria in the study, and finally the two evaluators jointly checked their own and each other's included The remaining literature that met the inclusion criteria was included in the study, and finally the two evaluators checked their own and each other's included literature, discussed and harmonised the inconsistent literature or had other researchers assist in their judgement [20,21].
Evaluation of the quality of the literature
The quality of the included literature was assessed using the Cochrane Risk of Bias Assessment Form [22], which includes seven entries: method of random allocation, allocation protocol concealment, blinding (to subjects, investigators and outcome assessors), completeness of outcome data, selective reporting of study results, and other sources of bias. Each entry was divided into three categories: "low risk", "unclear" and "high risk". In case of disagreement, the corresponding author was consulted for a decision. Risk of bias maps for the quality of the included literature were created using RevMan 5.4 software based on the evaluation results [23,24].
Statistical methods
Meta-analysis was performed using RevMan 5.4 software. Data on each outcome indicator in the included literature were tested for heterogeneity, and a fixed effects model was selected for analysis with combined study results if I2<50%, or a random effects model if I2≥50%. When there was significant clinical heterogeneity, subgroup analyses were performed based on the quality of the included literature, acupuncture treatment protocol, duration of treatment, and frequency of treatment. When heterogeneity was large (I2 > 80%), no quantitative data merging was performed and only descriptive analyses were performed for individual studies of interest. Dichotomous variables (TCMSSS score reduction rate) were used as effect sizes in terms of relative risk (RR), continuous variables (post-treatment serum TPO-Ab, TG-Ab, TSH, FT3, FT4 levels) were used as effect Sizes in terms of weighted Mean Difference (SMD), and combined effect sizes were represented by 95% Confidence Intervals (CI), with differences considered statistically significant at P < 0.05 [25,26].
Results
Literature search results
In the initial review of each database, a total of 75 relevant publications were obtained, 29 duplicates were excluded, and a further 39 publications were excluded after the initial screening and re-screening, resulting in the inclusion of 7 RCTs involving a total of 449 patients with HT in various regions of our China. The flow chart of the literature search is shown in figure 1.
Basic characteristics of the included literature
The 7 literature included in this study involved a total of 449 HT patients from different regions of our country, including 224 cases in the observation group (acupuncture) and 225 cases in the control group (modern medicine), all studies reported comparable general information such as gender, age and duration of illness with comparable or no significant differences. The shortest duration of treatment among them was 10 days and the longest was 12 weeks. The basic characteristics of each literature are shown in table 1 [27].
|
Inclusion of literature |
Sample size |
Gender |
Interventions |
Duration of treatment |
Frequency |
Outcome indicators |
|
|
T/C |
M/F |
Experimental group |
Compare group |
||||
|
Danni Zhou 2019[28] |
30/32 |
15/47 |
Acupuncture + Tuina |
Levothyroxine Sodium Tablets |
10days |
1 time/day |
(1)(2)(3)(4)(5)(6) |
|
Zhenkun Zhou 2014[29] |
38/38 |
30/46 |
Peripheral Acupuncture |
Thyroxine tablets |
2weeks |
1 time/day |
(1)(4)(5)(6) |
|
Yunhua Cui 2020[30] |
29/28 |
8/49 |
interlayer moxibustion |
Levothyroxine Sodium Tablets |
12weeks |
3times/week |
(1)(4)(5)(6) |
|
Huifen Xu 2013[31] |
30/29 |
13/46 |
interlayer moxibustion |
Levothyroxine Sodium Tablets |
28days |
1 time/day |
(1)(2)(3)(4)(5)(6) |
|
Shuting Lin 2017[32] |
30/30 |
5/55 |
Warm Acupuncture |
Levothyroxine Sodium Tablets |
12weeks |
1 time in 2 days |
(1)(2)(3)(5)(6) |
|
Xiuyu Hong 2020[33] |
37/38 |
22/53 |
Acupuncture+interlayer moxibustion |
Levothyroxine Sodium Tablets |
12weeks |
1 time in 2 days |
(1)(2)(3)(4)(5)(6) |
|
Zian Chen 2019[34] |
30/30 |
13/47 |
Acupuncture+Tuina |
Levothyroxine Sodium Tablets |
10days |
1 time/day |
(1)(2)(3)(4)(5)(6) |
Table 1: Basic characteristics of the included literature.
Note: (1): TCMSSS score reduction rate (2): APO-Ab (3): TG-Ab (4): FT3 (5): FT4 (6): TSH.
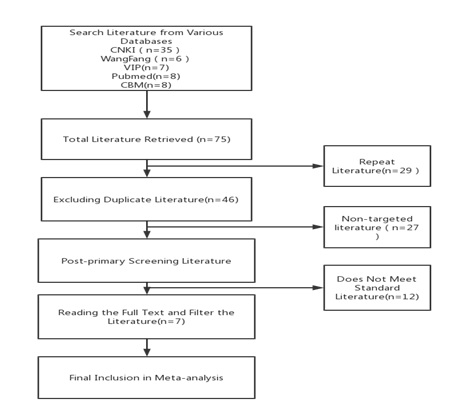 Figure 1: Flow chart of literature screening.
Figure 1: Flow chart of literature screening.
Western diagnostic criteria for Hashimoto's thyroiditis: 5 studies [28,30,32-34] used the 2007 Chinese Guidelines for the Diagnosis and Treatment of Thyroid Diseases prepared by the Endocrine Society of the Chinese Medical Association, and 2 studies [29,31] used the Morita Roku criteria (Japanese Ministry of Health and Welfare criteria); Chinese diagnostic criteria: 4 studies [28,30,32,34] referred to Chinese diagnostic criteria and all used the Guidelines for Clinical Research on New Chinese Medicines (2002), of which three studies [28,32,34] used the 2003 edition of Chinese Medicine Internal Medicine and one study [30] also used the 2009 edition of Practical Chinese Medicine Internal Medicine of Shanghai Science and Technology.
Literature quality evaluation
Four studies [30,32-34] were randomised with a clear method (using random number table method or lottery method) and were evaluated as "low risk"; two studies [28,29] were randomised but the method was not specifically described and were evaluated as "unclear "One study [31] had randomized groupings based on chronological order of admission and rated it as "high risk"; one study [32] had the method of concealed random sequence as the envelope method and rated it as "low risk"; the rest did not One study [34] mentioned single-blinding of performers, subjects and outcome evaluators, but the specific protocol was not given; the remaining six studies did not blind performers, subjects or outcome evaluators and all were rated as "unclear". "Three studies [28,30,32] reported cases of shedding and a small percentage of shedding, all <10%, but the possibility of an effect on outcome was present and was rated as "unclear"; the remaining four studies [29,31,33,34] reported no cases of shedding and the data were One study [31] reported primary and secondary outcome indicators and mentioned the absence of adverse events, which was evaluated as "low risk"; the remaining six studies [28-30,32-34] reported primary and secondary outcome indicators and were evaluated as "low risk". The remaining six studies [28-30,32-34] reported both primary and secondary outcome indicators and were evaluated as 'unclear'. The risk of bias graph is shown in figure 2.
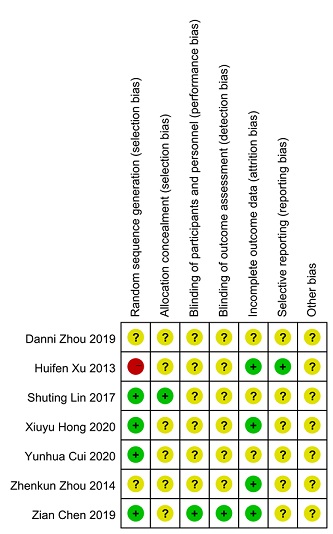 Figure 2: Risk of bias diagram.
Figure 2: Risk of bias diagram.
Meta-analysis
Rate of TCMSSS score reduction: All study literature reported scoring according to TCMSSS, and the rate of TCMSSS score reduction before and after treatment was used as an important observation. All reports were considered effective with a TCMSSS score reduction rate of ≥30%. The total sample size was 449 cases, with 224 cases in the experimental group and 198 cases effective, and 225 cases in the control group and 155 cases effective. The results of the heterogeneity test on the effective rate showed I2=26%, P=0.23, suggesting that there was no significant heterogeneity among the included studies, and a fixed effect model could be selected, with RR as the combined effect size indicator. thyroiditis was more effective than the control group [RR=1.29, 95%CI (1.17, 1.42), P < 0.001] (Figure 3).
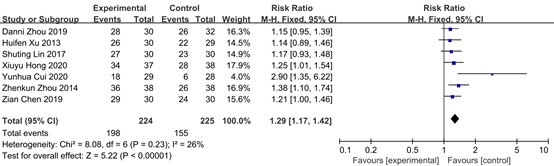 Figure 3: Forest plot of TCMSSS score reduction rates.
Figure 3: Forest plot of TCMSSS score reduction rates.
TPO-Ab levels: Five studies [28,31-33] reported on serum TPO-Ab levels and changes before and after treatment. A test of heterogeneity of serum TPO-Ab levels after treatment in these five papers showed a significant difference with I2=94%, P
Therefore, a subgroup analysis of post-treatment serum TPO-Ab levels was performed according to treatment frequency. 3 studies [28,31,34] had a treatment frequency of once a day, and the test of heterogeneity for these 3 studies showed I2=0%, P=0.38 suggesting low between-group differences and good homogeneity. A random effects model was chosen, and the results showed SMD=-3.37, 95% CI (-3.83, -2.90) .2 studies [32,33] had a treatment frequency of once every 2 days and the test of heterogeneity for these 2 studies was I2=0%, P=0.77, suggesting good homogeneity, choosing a random effects model, the results showed SMD=- 0.96, 95% CI (-1.31, -0.60), suggesting that the improvement in serum TPO-Ab levels was better in the treatment group than in the control group at a treatment frequency of once every 2 days; taken together, the improvement in serum TPO-Ab levels in patients with HT was better at a treatment frequency of once every 1 day than at a treatment frequency of once every 2 days(I2=98.5%, P<0.001) (Figure 4).
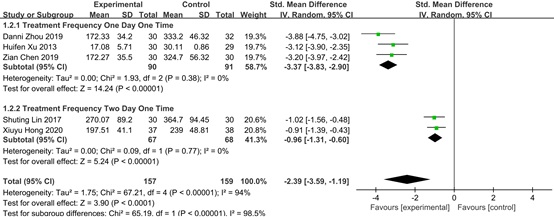 Figure 4: Forest plot for subgroup analysis of TPO-Ab levels after treatment.
Figure 4: Forest plot for subgroup analysis of TPO-Ab levels after treatment.
TG-Ab levels: Five studies [28,31-34] reported on serum TG-Ab levels and changes before and after treatment. Examination of the heterogeneity of serum TG-Ab levels after treatment in these five papers showed significant variability with I2=94%, P
Therefore, a subgroup analysis of post-treatment serum TG-Ab levels was performed according to treatment frequency. 3 studies had a treatment frequency of once a day, and the test of heterogeneity for these 3 studies showed I2=74%, P=0.02, suggesting a large difference between groups [28,31,34] . A random effects model was chosen and the results showed SMD=-2.86, 95% CI (-3.68, -2.03), suggesting a better improvement in serum TG-Ab levels in the treatment group than in the control group at a treatment frequency of 1 day. 2 studies [32,33] had a treatment frequency of 2 days 1 time and the test of heterogeneity for these 2 studies was I2=57%, P=0.13, suggesting some heterogeneity, selecting a random effects model, the results showed SMD=-0.72 , 95% CI (-1.26, -0.19), suggesting that the improvement in serum TG-Ab levels was better in the treatment group than in the control group when the frequency of treatment was 1 in 2 days; taken together, it is possible that the improvement in serum TG-Ab levels in HT patients was better when the frequency of treatment was 1 in 1 day than when the frequency of treatment was 1 in 2 days(I2=94.5%, P<0.001) (Figure 5).
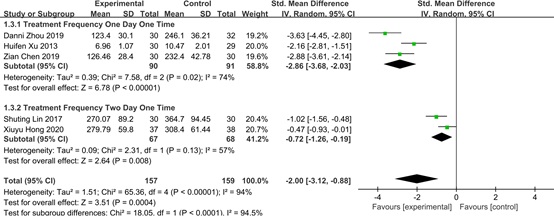 Figure 5: Forest plot for subgroup analysis of TG-Ab levels after treatment.
Figure 5: Forest plot for subgroup analysis of TG-Ab levels after treatment.
TSH levels: All studies used serum TSH levels as the primary outcome indicator. 1 study [30] reported no statistically significant difference in serum TSH levels before and after treatment, and 6 studies [28,29,31-34] reported statistically significant serum TSH levels before and after treatment. 1 study [33] had incomplete data (missing s), therefore, the remaining 5 studies of post-treatment Serum TSH levels were tested for heterogeneity and the results showed I2=90%, P<0.001, suggesting a significant difference. Therefore, without quantitative analysis, individual studies were observed, with the exception of Yunhua Cui [30], and the remaining report suggested that acupuncture-related therapies improved serum TSH levels better in patients with HT than in controls, but the exact improvement and efficacy is uncertain at this time (Figure 6).
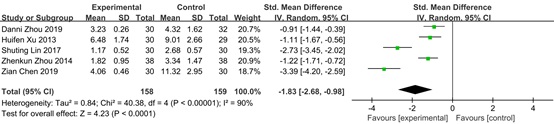 Figure 6: Forest plot of TSH levels after treatment.
Figure 6: Forest plot of TSH levels after treatment.
FT3 levels: Six studies [28-31,33,34] used serum FT3 levels as the primary outcome indicator and two studies [30,33] reported no statistically significant differences in serum FT3 levels before and after treatment, therefore, a test of heterogeneity was performed on the post-treatment serum FT3 levels of the remaining four studies [28,29,31,34] and the results showed that I2=77%, P=0.005, large variability, sensitivity analysis using the stepwise exclusion literature method found that after excluding the study of Zian Chen [34], the results of the test of variability showed I2=46%, P=0.16, suggesting good homogeneity, the random effect model was selected and the combined effect size, SMD=0.69, 95% CI (0.15,1.22), the combined effect size located to the right of the equivalence line, showed positive results, all of which suggest that acupuncture-related therapies were more effective in improving serum FT3 levels in HT patients than in controls (Figure 7).
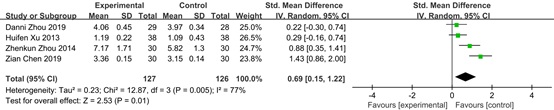 Figure 7: Forest plot of FT3 levels after treatment.
Figure 7: Forest plot of FT3 levels after treatment.
FT4 levels: All studies used pre- and post-treatment serum FT4 levels as the primary outcome indicator. 1 study [30] reported no statistically significant difference in pre- and post-treatment serum FT4 levels. A test for heterogeneity in post-treatment serum FT4 levels from the remaining 5 studies [28,29,31-34] showed I2=93%, P<0.001, with significant heterogeneity, looking at each study and comparing The treatment protocol, duration of treatment and frequency of treatment were compared across studies and it was found that the reason for the variability may be related to the duration of treatment.
Therefore, a subgroup analysis of post-treatment serum FT4 levels was performed according to the duration of treatment. 2 studies [28,34] had a duration of treatment ≤ 10 days, and the heterogeneity test for these two studies was I2=91%, P<0.001, suggesting large variability. The random effect model was chosen and the results showed SMD=0.93, 95% CI (0.48,1.38), and the above the results suggest that acupuncture-related therapy improved serum FT4 levels better than the control group in patients with ≤10 days of treatment; 2 studies [29,31] with >10 days and ≤28 days of treatment were tested for heterogeneity and the results showed I2=89%, P=0.003, suggesting large variability, and the results of the random effect model were chosen to show SMD=1.72, 95% CI (-1.79, 5.22), the above results suggest that at sessions >10 days and ≤28 days, acupuncture-related therapies was not statistically different from that in control group; 2 studies [32,33] with sessions = 12 weeks were tested for differences, the results showed I2=0%, P=0.96, suggesting homogeneity was good and the random effect model was chosen, the results showed SMD=1.57, 95% CI (0.71,2.44). In the overall analysis, the improvement effect of the experimental group on the level of serum FT4 was better than that of the control group SMD=0.94, 95% CI (0.47,1.42) (Figure 8).
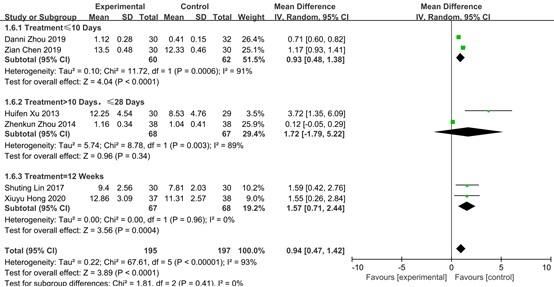 Figure 8: Forest plot for subgroup analysis of FT4 levels after treatment.
Figure 8: Forest plot for subgroup analysis of FT4 levels after treatment.
Discussion
Hashimoto's thyroiditis: Hashimoto's thyroiditis is the most common autoimmune thyroid disease and one of the most common endocrine disorders [35]. It is common in women, with a slow onset and often no specific discomfort at the beginning. However, the incidence of Cushing's syndrome alone can be as high as 60% after long-term use of hormonal drugs [36], posing a major safety risk. In contrast, TCM-related therapies represented by acupuncture have the advantages of high safety, low adverse effects and side effects, and more and more studies have confirmed that acupuncture-related therapies have bi-directional, specific and holistic regulatory effects on the immune system [37], and are therefore widely used in the treatment of immune system diseases including Hashimoto's thyroiditis.
Limitations of this study: This study has certain limitations: (i) the total sample size was small and the evidence was insufficient; (ii) the quality of the included literature was not high, 1/3 of the studies were randomised, but the exact method was not specified, the allocation scheme was only used in 1 study using a randomised group allocation ordinal list, opaque envelope concealed grouping, and only 1 study mentioned single-blinding for performers, subjects and outcome evaluators, but none of them were explicitly blinded; (iii) the included literature were all in Chinese; (iv) Diagnostic criteria for Hashimoto's thyroiditis were not fully standardised and there was an unknown risk of bias. (v) The selection of acupuncture-related therapies, acupuncture points, manipulation, duration and frequency of treatment varied widely between trials, with varying clinical efficacy.
In the future, clinical observation should pay attention to methodology, randomization and concealed grouping protocols, etc. Blinded methods are difficult to implement in clinical practice. There is a wide variety of acupuncture-related therapies and techniques, so it is worthwhile to explore effective therapies and standardized methods of operation to facilitate learning and transmission and research promotion.
Study findings: Acupuncture-related therapy was superior to the alternative therapy group in terms of improving the symptoms of Hashimoto's thyroiditis and related indicators (serum TPO-Ab, TG-Ab, TSH, FT3, FT4 levels). The subgroup analysis of post-treatment serum TPO-Ab and TG0-Ab levels showed that different treatment frequencies improved the serum TPO-Ab and TG0-Ab levels differently: compared to the 2-day treatment frequency, the 1-day treatment frequency of acupuncture-related therapy improved the serum TPO-Ab and TG0-Ab levels better. However, the majority of these studies have methodological flaws and the level of evidence is low, so the conclusions need to be further validated.
References
- Gao Y, Liu M, Xiu RJ (2013) Advances in the immunological pathogenesis of Hashimoto's thyroiditis. Internal Medicine Theory and Practice 8: 392-396.
- Guoyu Z, Huina W, Panpan G, Ling C, Hong W, et al. (2020) Research progress in the pathogenesis of Hashimoto's thyroiditis and its pathogenesis. Journal of Xinxiang Medical College 37: 984-989.
- Hiromatsu Y, Satoh H, Amino N (2013) Hashimoto's Thyroiditis: History and Future Outlook. Hormones 12: 12-18.
- Yixue G, Min Z, Liang H, Wei L, Yuanyuan H et al. (2019) Epidemiology of Antibody-Positive Autoimmune Encephalitis in Southwest China: A Multicenter Study. Frontiers in Immunology 10: 2611.
- Ran Z, Fengzhen Z, Chuanqiang F, Guangping G (2016) Advances in the study of Hashimoto's thyroiditis in Chinese and Western medicine. World abstract of the latest medical information 16: 91-92.
- Wang P, Jianfeng W, Shanxin L, Wang J (2015) Research progress on the pathogenesis and treatment of Hashimoto's thyroiditis. Pharmacological Research 34: 599-603.
- Guo L, Rongjuan X, Fangfang G, Hong L (2016) Advances in Chinese and Western medicine treatment of Hashimoto's thyroiditis. Journal of Modern Traditional Chinese and Western Medicine 25: 333-335.
- Fangyuan L, Xiaoling L, Yuanyuan Q, Yan L, Zhengjie Y, et al. (2016) Research progress of acupuncture in the treatment of Hashimoto's thyroiditis[J]. Asia-Pacific Traditional Medicine 12: 51-53.
- Julian PTH, James T, Jacqueline C (2019) Cochrane Handbook for Systematic Reviews of Interventions. America:John Wiley & Sons, Ltd, USA.
- Zhou D, Hong YL, Wang YC, Qi FJ (2019) Clinical study analysis of 62 cases of Hashimoto's thyroiditis treated by acupuncture combined with pushing the bridge and bow technique from liver, spleen and kidney theory [C] Chinese Acupuncture and Moxibustion Society. New era, new thinking, new leap, new development-2019 Annual Meeting of the Chinese Acupuncture and Moxibustion Society and 40th Anniversary Review Proceedings. Chinese Acupuncture and Moxibustion Society: Chinese Acupuncture and Moxibustion Society 2019: 6.
- Zhenkun Z, Gu S, Xu C (2014) Clinical observation of 38 cases of Hashimoto's thyroid nodules treated with the peri-acupuncture method. Chinese Traditional Medicine Science and Technology 21: 194-224.
- Yunhua C, Feng J, Wu H, Liu H, Hu Z, et al. (2020) Efficacy of interdigitated medicinal cake moxibustion in the treatment of Hashimoto's thyroiditis with spleen and kidney yang deficiency. Shanghai Journal of Acupuncture and Moxibustion 39: 1483-1490.
- Xu H (2013) Treatment of chronic lymphocytic thyroiditis with levothyroxine sodium in interdigitated cake moxibustion. Zhejiang Journal of Integrative Medicine 23: 459-461.
- Shuting L (2017) Clinical observation on the treatment of Hashimoto's thyroiditis with hypothyroidism by combining warm acupuncture and moxibustion with Raitis. Fujian:Fujian University of Traditional Chinese Medicine.
- Xiuyu H, Zhang X (2020) Clinical study of acupuncture combined with western medicine in the treatment of Hashimoto's thyroiditis with hypothyroidism. Chinese and foreign medical research 18: 19-22.
- Clinical observation and research on the treatment of Hashimoto's thyroiditis by acupuncture combined with Tui Na. Wuhan: Hubei University of Traditional Chinese Medicine.
- Lv S Y, Wan C, Jin YT, Huang W, Zhou ZY (2019) Clinical study on the combination of acupuncture and medicine in the treatment of Hashimoto's thyroiditis. Chinese Society of Acupuncture and Moxibustion. New thinking, new thinking, new leap, new development in a new era - 2019 Chinese Acupuncture and Moxibustion Society Annual Meeting and 40th Anniversary Review Proceedings. Chinese Society of Acupuncture and Moxibustion: Chinese Society of Acupuncture and Moxibustion 2019: 4.
- Zeng YC, Huang SY, Wu D (2021) Effectiveness analysis of clinical pharmacists' participation in pharmacological monitoring of patients with long-term glucocorticoid use. Chinese contemporary medicine 28: 17-20.
- Wang P, Wang L (2020) Research progress and ideas related to the regulation of immunity by acupuncture and moxibustion. Tianjin TCM 37: 1316-1320.
- Liu Z, Guo R (2018) Ultrasound elastography for the diagnosis and staging of Hashimoto's thyroiditis. Imaging Research and Medical Applications 2: 138-140.
- Lun Y (2015) Diagnostic application of color ultrasound combined with ultrasound elastography in patients with diffuse goiter and Hashimoto's thyroiditis. Chinese National Health Medicine 27: 35-36.
- Wang E, Qi R, Han L, Yang L (2020) Clinical study on the adjuvant treatment of Hashimoto's thyroiditis with Xia Ku Cao capsule. New Chinese Medicine 52: 91-94.
- Sin Q-H, Liu M-Z, Sun D, Qiu J-H, Lei T (2019) Exploring the efficacy of selenium supplementation in the treatment of chronic lymphocytic thyroiditis with normal thyroid function. Journal of Medical Research 48: 69-72.
- Liu Y, Zhao J, Zhu M-L, Wu H-G, Ji J, et al. (2019) Systematic evaluation and meta-analysis of moxibustion in the treatment of Hashimoto's thyroiditis. World Science and Technology - Modernization of Chinese Medicine 21: 1573-1582.
- Du G, Xu C, Xu Y (2021) Progress of clinical research on Chinese and Western medicine in Hashimoto's thyroiditis. Journal of Hainan Medical College 27: 1109-1115.
- Shi M, Wang Y (2017) An analysis of Professor Wang Yue's ideas on the treatment of Hashimoto's thyroiditis from the liver and spleen theory. Journal of Zhejiang University of Traditional Chinese Medicine 41: 891-894.
- Xiong F, Zhao W, Song K, Zhang (2021) A reticulated Meta-analysis of the effects of acupuncture-related therapies and SSRIs on the long-term efficacy of post-stroke depression. Journal of Hainan Medical College 27: 1328-1335.
- Wang YJ, Yang YP, Wen YY, Li EJ, Chen S (2020) Correlation analysis of needle retention time and efficacy of acupuncture for facial muscle spasm. Jiangsu Traditional Chinese Medicine 52: 66-69.
- Wang J, Wang J, Zhang J, Ou L, Yang T, et al. (2018) Systematic evaluation of the effect of oral ulcer containing tablets in the treatment of recurrent aphthousulcers. Chinese Journal of Clinical Health Care 21: 752-756.
- Li Y, Song D, Han X, Xiao LY, Wang R, et al. (2021) Meta-analysis of the effects of intensive glucose-lowering therapy with insulin on ventricular remodeling and serum inflammatory factors in patients with AMI with hyperglycemia. Medical Information, 34: 110-115.
- Zhang MT, Tan K, Hu S, Liao LY, Shi WY, et al. (2021) Meta-analysis of acupuncture to improve the depressive state and daily living ability of depressed patients after stroke. Shanghai Journal of Traditional Chinese Medicine 55: 13-19.
- Zhang Y, Zhao J, Ren C, He Z, Liang C (2021) Meta-analysis of the efficacy of Musk Tongxin Dripping Pill combined with conventional drugs in the treatment of chronic heart failure. Journal of Difficult Diseases 20: 508-514.
- Zhang M, Liu H, Guo Y, Shi Y (2020) Meta-analysis of clinical efficacy and safety of leigongtang polysaccharide in the treatment of diabetic nephropathy. Medical Review 26: 1828-1836.
- Huang D, Chen Y, Pang B, Lin X (2019) Meta-analysis of the clinical efficacy and safety of Panaxia alba and Atractylodesmacrocephala soup in the treatment of acute cerebral infarction[J]. Journal of Integrated Cardiovascular and Cerebrovascular Diseases in Chinese and Western Medicine 17: 3089-3097.
- Zhang Y, Wu S, Yue G, Bo Y, Ma H, et al. (2017) Meta-analysis of postoperative radiotherapy versus surgery alone for mid- to late-stage resectable esophageal cancer. China Medicine Herald 14: 94-98.
- Guan QY, Xu EP, Wang YAO, Fan XUN, He JM (2020) Meta-analysis of a randomized controlled clinical trial study on the treatment of chronic heart failure with Wu Ling Tang. World Science and Technology - Modernization of Chinese Medicine 22: 4103-4110.
- Ou B (2017) Clinical efficacy of paclitaxel combined with nedaplatin in the treatment of intermediate and advanced cervical cancer with concurrent radiotherapy and consolidation chemotherapy. Electronic Journal of Modern Medicine and Health Research 1: 73.
Citation: Si W (2022) Meta-analysis of Acupuncture-Related Therapy Versus Western Drug Replacement Therapy in the Treatment of Hashimoto's Thyroiditis. J Altern Complement Integr Med 8: 290.
Copyright: © 2022 Weichen Si, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

