
MMRC (Alhydran®), an Interesting Treatment Option for a Disrupted Skin Barrier
*Corresponding Author(s):
Van Leen MWFElderly Care Physician, Helmbloem 15, 3068AC Rotterdam, Netherlands
Tel:+0031 654695451,
Email:martin_van_leen@kpnmail.nl
Abstract
Skin aging, scar formation and some types of eczema are associated with dysregulation of the intracellular water content of the epidermis. One of the main reasons for this is a disruption of the skin barrier function which subsequently leads to an increased Trans Epidermal Water Loss (TEWL). This often results in a dry, fragile, and itchy skin, requiring rehydration and restoration of the barrier function. Based on the currently available literature, there is no clear evidence about the most optimal treatment to achieve these goals and a myriad of indifferent creams are advised in (inter) national guidelines. Since 2005 a Medical Moisture Retention Cream (MMRC) Alhydran® is used in many health care settings worldwide for patients with various pathologies associated with an impaired barrier function of the skin. This article reports specifically about the available literature on MMRC and explains how its use may result in less itching and a better hydration status of the skin.
Keywords
Disrupted skin barrier; Dry skin; Indifferent cream; Itching; Loss; Natural moisturizing factor
INTRODUCTION
The skin is the largest human organ with a surface area of around 2 m2. It has 2 main functional layers: the epidermis and dermis. The main functions of the skin are protection, thermal regulation, sensation, absorption, excretion and endocrine production [1]. The main focus of this article is on the vital barrier function of the epidermis as it is crucial for optimal functioning of the skin. The skin barrier consists of a physical barrier (stratum corneum epidermis), a biochemical barrier (pH gradient, calcium gradient), the cutaneous immune system and a barrier function via regulation of the hydration of the skin. Related to the preservation of a good water balance in the skin, specifically the physical barrier and the hydration regulation barrier need attention.
The outermost layer of the skin, the stratum corneum, is functioning as the skin’s main barrier and consists of 15-20 layers of dead skin cells (corneocytes), water and a lipid matrix [2,3]. Every 24 hours the top layer is replaced by the underlying layer to maintain optimal skin integrity. The corneocytes and intercellular lipids are held in a matrix, built up like a brick wall, in which corneocytes are seen as the bricks and the lipids as the mortar. This skin layer structure regulates the continuing process of water movement in/out the skin (= trans epidermal water loss/TEWL)) and prevents overhydration and dehydration [2,3]. Usually, there is a balance in water movement, which is preserved by a well-functioning skin barrier. A compromised skin barrier frequently results in symptoms like severe itching, redness of the skin, but also in a dry skin, skin defects and pain. Because of these symptoms, adequate treatment to restore the barrier function is strongly recommended [4,5].
During lifetime, the epidermis is able to resist multiple influences of solids, liquids, gases, attacks of viruses, bacteria, fungi and other microbes [4]. However, there are several age-related histological skin changes influencing skin composition and quality. These involve loss of subcutaneous fat, decrease of collagen and elastin formation with loss of dermal thickness, decrease of number and function of sweat glands, decreased sebum production, flattening of the dermal-epidermal ridges, increase of skin surface pH, increase of transepidermal water loss and reduced skin moisture [4-7].
One of the additional but equally important mechanisms to control TEWL is the ability to produce a chemical protective coating called Natural Moisturizing Factor (NMF) responsible for preserving adequate hydration of the stratum corneum [8]. Proper hydration of the stratum corneum is crucial for a healthy skin in 3 different ways: [9] 1. It maintains plasticity of the skin, protecting it from damage; 2. It allows hydrolytic enzymes to function in the process of desquamation; 3. It contributes to optimum stratum corneum barrier function. NMF is composed primarily of free amino acids, various derivatives of these amino acids such as pyrrolidone carboxylic acid, urocanic acid (a natural absorber of Ultraviolet [UV] light) and inorganic salts, sugars, as well as lactic acid and urea. Inorganic salts identified, include chlorides, phosphates, and citrates of sodium, potassium, calcium, and magnesium [10]. NMF is packaged within the corneocytes and its components are highly efficient humectants that attract and bind water from the atmosphere, drawing it into the corneocytes.
As mentioned above and shown in figure 1, a normal skin is able to resist effects of possibly threatening external stimuli, like UV-rays and irritants like soap. A damaged skin barrier possibly will lead to excess loss of water because of pathophysiological changes in the structure of the skin.
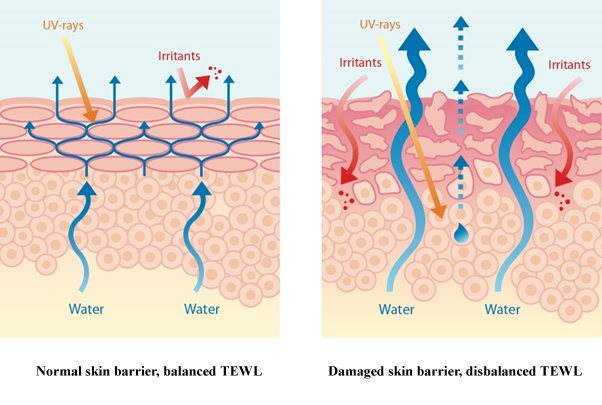 Figure 1: Healthy skin - disrupted skin.
Figure 1: Healthy skin - disrupted skin.
Disruption of the skin barrier, problems to restore the skin barrier due to age-related changes as well as skin diseases, may result in excessive water loss, deficient/slow lipid production, a dryer skin and a higher pH, additionally resulting in a higher risk of infections [9-13]. It is universally known that the skin barrier is functionally and pathologically involved in several dry skin diseases like psoriasis, atopic and contact dermatitis and hypostatic dermatitis [14].
Next to these diseases, disruption of the skin barrier often occurs in case of delayed post traumatic wound healing. In such cases there is an increased risk of unfavourable hypertrophic scar formation. The hypothesized mechanism behind this hypertrophic scar formation has been explained by Mustoe [15]. He states that the impaired barrier function of the skin results in dehydration of the epidermis which will trigger keratinocytes in the basal layer to produce cytokines that will stimulate fibroblasts in the dermis for proliferation and increased collagen production. This increased collagen production will lead to disfiguring and function-limiting hypertrophic scars.
CURRENTLY ADVISED TREATMENTS FOR ECZEMA AND/OR DRY SKIN
With a normal skin barrier function, there is a well-balanced TEWL resulting in an optimal skin condition so that there are no complaints such as dry skin, itching or pain which negatively affect the Quality of Life (QoL). Skin barrier damage mostly can be prevented by common daily skin care. In general, avoiding skin contact with aggressive solids (soap, washing cremes) and liquids is essential to reduce excess trans epidermal water loss and to keep an optimal skin pH between 4.6 and 5.6 [16]. Next to normal daily skin care, currently various topical treatments, are used to re-establish a normal skin barrier function in the case of skin damage/diseases [17]. The treatments can be found in guidelines for treatment of eczema as well as guidelines for the prevention and treatment of scars [18-21].
These guidelines in general advise local treatment for skin barrier dysfunction with indifferent moisturizers (without pharmacological ingredients, for example corticosteroids). Humectants, occlusives and emollients are the components of a good moisturizer but many moisturizers do not contain all three components [22]. Among the effective humectants used in moisturizers are propylene glycol, urea, hyaluronic acid and sorbitol - substances that naturally attract water. When used in humid conditions, humectants pull water from the environment to the skin. In dry environments (<50% humidity), humectants also draw moisture from the deeper layer of the skin (the dermis) to the outermost layer (the epidermis). However, all additional hydration that humectants bring to the epidermis may easily evaporate. This is where occlusives have an important role. Common occlusives include petrolatum, mineral oil, dimethicone caprylic/capric triglyceride and beeswax. These substances are hydrophobic (repel water) and, as such, create a barrier through which water loss is significantly decreased. By applying a moisturizer with occlusives to the skin, the skin retains its internal water content and with certain occlusives on the skin, the rate of TEWL can decrease by up to 98%. Emollients include isopropyl palmitate, lanolin, coconut oil and jojoba seed oil. These substances help keeping the skin smooth, flexible and lubricated. Emollient constituents, found naturally in the skin’s oils, such as lipids and fatty acids, play an important role in the skin’s architecture. In moisturizers, they improve the feel and comfort of the skin while largely reducing water loss by formation of an external protective film.
The use of indifferent moisturizing agents increases the moisture content of the skin and reduces itching and irritation [20]. However, it is unknown which specific indifferent part of a moisturizer is most effective and currently the experience of the prescriber and the preference of the patient play an important role in the ultimate choice. The mostly used products are: cetomacrogol cream, lanette cream, vaseline cetomacrogol cream, vaseline lanette cream, cooling ointment (= unguentum leniens), cetomacrogol ointment, lanette ointment or paraffin / vaseline in equal parts.
If treatment with these agents is insufficient, the use of topical corticosteroids often is advised. Corticosteroids suppress the inflammatory response and combat the itchiness. Corticosteroids are divided into 4 classes of increasing strength. It is unclear which product is most effective per class, but class 4 corticosteroid is generally not advised because the risk of secondary epidermal and dermal damage is high. In case of insufficient treatment outcome after corticosteroid application, referral to a dermatologist is advised.
CURRENT STATE OF THE ART OF SCAR MANAGEMENT
Scar treatment guidelines describe the importance of prevention and treatment of hypertrophic scars with an impaired skin barrier function associated with increased TEWL. Treatment recommendations focus on the use of pressure garments in combination with silicones (sheets and fluid silicone gels) and moisturizers as well as UV protection [20,21]. However, correction of the disrupted moisture balance is the main point of focus. Scar management in all its aspects needs to be evaluated on a regular basis until complete scar maturation, after which the treatment can be terminated. However, hydration by means of moisturizers should be continued, sometimes lifelong.
The basic treatment by using moisturizers as initial therapy once epithelialization has been completed, is based on the hypothesis that hydration of the epidermis and restoration of the skin water barrier will restore the balance of the cytokine profile of keratinocytes and fibroblasts in the skin. As such this will add to the prevention and treatment of additional abnormal scarring, especially in patients at high risk of excessive scar formation [21,22]. Klotz et al., published in 2017 a survey report about the use of different moisturizers in Australia, Canada and the USA [23]. In total 29 products were prescribed. The survey revealed that the use of a certain moisturizer by the respondents was mainly based on the choice of the previous specialist in their service and the patient’s feedback. The conclusions of this article were that the ideal moisturizer should be conducive to scar maturation, be low irritant, prevent skin drying and negative effects to skin barrier function, and minimize abundant Trans Epidermal Water Loss (TEWL). Despite this, there is scarce evidence for the use of moisturizers and further research is necessary [24].
MEDICAL MOISTURE RETENTION CREAM (MMRC, ALHYDRAN®)
In 2005, Medical Moisture Retention Cream (MMRC, Alhydran®) was first introduced as a promising product for restoring a well-balanced TEWL and an improved hydration status of the skin [25]. MMRC was at that moment specifically used for the prevention and treatment of hypertrophic scars in burn patients.
PRODUCT INFORMATION
MMRC is oil in water emulsion which contains freshly processed Aruba Aloe Vera gel, oils and other fatty ingredients. The possible working mechanism of this cream is the moisturizing effect of the Aloe Vera gel combined with an adequate occlusive effect caused by the fatty ingredients. Nowadays, MMRC is a moisturiser with evidence from in vivo studies about its effects on the skin barrier function and skin hydration status used in many different pathologies.
EXPERIENCES WITH MMRC
The most important studies on MMRC were gathered via a regular literature search and from documented congress presentations/posters. In the next table and paragraphs the main findings are shown.
ARTICLES
Hoeksema et al., published in Burns (2013) a prospective, open controlled, comparative trial of which the objective was to compare the occlusive and hydrating properties of MMRC, three fluid silicone gels and four silicone sheets [26]. Tape stripped skin was used as a standardized scar like model on both forearms of 40 healthy volunteers. At different time points, Trans Epidermal Water Loss (TEWL) as well as the hydration state of the stratum corneum were measured and compared with intact skin and a scar-like control over a 3-4 h period. Objective measurements were performed with the Tewameter TM 3001 for TEWL and the Corneometer CM8251 for skin hydration, both devices from Courage & Khazaka electronic GmbH, Germany [26]. Measurements showed that the Hydrating Gel-Cream (MMRC) could provide the same occlusive and hydrating properties as fluid silicon gels. MMRC provided good occlusion and hydration for a period of at least 4 hours. Excessive TEWL decreased within one hour of application and maintained stable for more than 4 hours. In the second part of the study, the results confirmed that MMRC decreased the TEWL values and provided a well-balanced hydration state of the scar model to near normal values. This in contrast to silicone sheets causing a practically complete occlusion which easily can lead to skin maceration.
In February 2017 Rondas and Schols published a multiple case study on MMRC in 18 patients with venous eczema [27]. In total 18 patients with moderate hypostatic eczema were included in this study. Indications for use of MMRC were: dry, itching and/or a flaky skin. In 17 patients experts evaluated the overall effect of MMRC as positive, assumably attributed to the correction of the TEWL balance. The conclusion was that the use of MMRC in patients having an itchy, scaly, and dry skin due to underlying chronic venous insufficiency, may decrease the topical use of corticosteroids.
POSTERS AND ORAL PRESENTATIONS AT INTERNATIONAL CONGRESSES
In 2007 Monstrey et al., presented a poster with the subject: two years of experience with a new product based on Aloe Vera for hydration of burn scars (MMRC), which was accepted by the 12th congress of the European Burns Association (EBA) Budapest, Hungary 12-15 September [25] MMRC was used in 50% of their burn patients. All patients (children and adults) had skin grafts or burns that healed conservatively with a healing time of >18 days, which is a clear indication for a high risk of developing hypertrophic scars. They saw no allergic reactions on MMRC, a good aesthetic outcome(measured with the Vancouver Scar Scale) and less itching experienced by >90% of the patients.
In 2008 Van Kempen et al., performed a pilot study with 51patients in which they found that MMRC could impact the itching intensity after burns [28]. The study indicated that MMRC decreases the itching intensity (measured by Visual Analogue Thermometer or the Numeric Rating Scale) after one week application. A further reduction was seen after one month and remained stable after 3 months. This reduction in itching intensity contributed also to the improvement of quality of life. Ziegenthaler et al., (2010) published a poster about their clinical treatment observation study “The effect of scar treatment products on unpleasant physical manifestations in patients suffering from extensive burn scarring” [29]. The study was done in 15 patients participating in an in-patient rehabilitation programme. The patients who continued to experience itching and a sensation of tightness exceeding 50% on a VAS scale after initial wound care by SR Unguentum Cordes (the then standardly used moisturizer) were switched to MMRC. MMRC appeared to be able to minimize manifestations such as itching and the sensation of tightness. No adverse events were reported and the product could be combined with the administration of textile-based compression therapy.
The same author presented at the European Burn Association 2011 (EBA 2011) a study in 75 patients. The influence of scarring on Quality of Life and the therapeutic influence of MMRC in the early stage of scar maturation was analysed [30]. In this study the Pationnaire®-questionnaire with a new skin module was compared to the SF-36v2® Health survey while investigating the effects of MMRC. The study showed a reduction in redness and skin tension. Also, a reduction in itching and dryness of the skin was noted. The general quality of life experience increased, and no adverse events were experienced. Furthermore, MMRC was successfully used to reduce the subjective and unpleasant side effects of burn scars, such as redness and skin tension, while it could be used together with (textile garments) pressure therapy without problems.
Giovannini et al., (2011) presented a poster at the (EBA 2011) about their experience regarding the application of MMRC in the treatment of pathologic scars in thirteen patients (with a total of 21 scars) who were treated with cryoshape therapy and initial therapy with Vaseline gauze and hydrocolloid ointments [31]. Two weeks after the cryoshape therapy additional application of MMRC was started. All patients experienced improvement of their scar aspects, pain and itching. No intolerance or allergic reactions on MMRC occurred. The author concluded that cryoshape and MMRC showed good synergy in the management of pathological scars. Hoeksema et al., (2013) presented at the 15th European Burns Association congress in Vienna, Austria about the results of their study published in Burns in 2013 with the title: Scar management by means of occlusion and hydration: A comparative study of silicones versus a hydrating gel cream (Alhydran).
CASE REPORTS
Ashman et al performed in 2013 a case study, investigating whether psychological wellbeing can be enhanced by improving the appearance of scar tissue post injury [32]. A girl (7 years old) sustained a traumatic injury to her right shin. The scars which resulted from this injury resulted in the child refusing to wear dresses and shorts throughout the summer. Dual therapy of a silicone gel sheet to reduce hyper epithelialization and MMRC to preserve the skin water balance was initiated in November 2013. Within 6 weeks improvement of the scar (i.e., thickness and scar appearance) was seen and after 5 months the scar significantly decreased in size and the overall appearance was much more acceptable for the child. She was happy that the scar was fading so she could wear nice dresses again. The conclusion of the case study was that scar management should be initiated immediately after wound closure and be continued until the scar no longer causes physical or psychological problems.
Rijkenberg presented a case study regarding the use of MMRC in the treatment of burn scars following a chemical explosion, at the European Burn Association 2015 [33]. A 58-year old male patient was injured by a fire which resulted from a chemical explosion. The fire caused flame burns to the skin on his face and hands. The patient complained of an extremely dry an itching skin. Furthermore his hands were highly oedematous. Post-burn scar therapy consisted of (twice-weekly) manual lymphatic drainage, bandaging and endermotherapy followed by application of silicon sheets. Moreover, the patient applied MMRC 4 to 6 times per day as a very thin layer. MMRC was also applied before and after endermotherapy treatment. MMRC made the skin of face and hands more flexible and reduced itching.
DISCUSSION
The skin may undergo changes due to ageing, diseases, and injuries, which easily can result in disruption of the skin barrier. A disrupted skin barrier will result in excessive trans epidermal water loss and a dryer skin, leading to symptoms of severe itching, redness of the skin and additionally this can also trigger eczema and stagnation of wound healing. Currently, the best way to treat a disrupted skin barrier is not known due to a lack of good scientific evidence. However, there is general consensus that a disrupted skin barrier should be restored to obtain a well-balanced hydration state of the skin. There have been no randomised controlled trials conducted with moisturizers and there are also no in vivo tests performed for most of the used moisturizers. MMRC (Alhydran®) is the only moisturizer with published in vivo tests on different pathologies.
The available published abstracts and papers of these studies all show relevant improvements, indicated by the prevention and reduction of hypertrophic scarring, increase of elasticity of the skin and reduction of itching. All these advantages may increase the Quality of Life (QoL) for patients considerably.
A limitation might be that currently only a few high quality studies are available about MMRC (Alhydran®) (Table 1). However, the comparative study of MMRC versus silicone fluid gels and sheets is mentioned by Klotz as the only high quality study on moisturizers currently available [23,24]. Due to the promising results obtained so far, a randomized controlled and double blinded study comparing MMRC versus other moisturizers would be appropriate and recommended.
|
|
Author(s) |
Type publication |
Main findings |
Published / Presented (year) |
|
1 |
Hoeksema H, de Vos M, Verbelen J, Pirayesh A, Monstrey S [26] |
Published article |
MMRC has the same occlusive and hydrating properties as fluid silicon gels in patients with burn wounds. MMRC reached a well-balanced hydration state of the scar. |
Burns, 2013 |
|
2 |
Rondas AALM, Schols JMGA [27] |
Published article |
Use of MMRC in patients having an itchy, scaly, dry skin due to underlying venous insufficiency, may decrease the use of topical steroids. |
Journal of Gerontology and Geriatric Research, 2017 |
|
3 |
Monstrey S, Pirayesh A, Lambrecht E, Lauwaert S, Verbelen J, Hoeksema H [25] |
Published poster of clinical study |
MMRC use in burn patients resulted in better aesthetic outcome and less itching. No allergic reactions. |
Abstract book EBA 2007 |
|
4 |
Van Kempen HJ, Dokter J, Oen IMMH [28] |
Published poster of clinical study |
MMRC decreased itching intensity in 51 patients with burn wounds, which contributed to improvement of quality of life. |
Abstract book EBA 2007 |
|
5 |
Ziegenthaler H [29] |
Published poster of clinical study |
MMRC was able to minimize itching and the sensation of tightness in 15 patients with burn wounds. No adverse reactions were noticed. MMRC could be combined with textile-based compression therapy. |
Abstract book DAV 2010 |
|
6 |
Ziegenthaler H [30] |
Published poster of clinical study |
MMRC reduced redness, skin tension, itching and dryness in 75 patients with burn wounds. MMRC improved the quality of life. No adverse events and it could be combined with textile-based compression therapy. |
Abstract book EBA 2011 |
|
7 |
Giovanni U [31] |
Published poster of clinical study |
Patients with pathological scars after breast surgery (5), abdominal surgery (2), ear surgery (2), lip surgery (1), sternotomy (1) and a burn injury (1) experienced improvement of scar aspects, pain and itching. No intolerance or allergy. MMRC and cryoshape therapy showed good synergy. |
Abstract book EBA 2011 |
|
8 |
Ashman S, Kray SJ, Tyne & Wear [32] |
Published poster of clinical case study |
MMRC improved the scar (a.o. thickness, scar appearance, size) of a burn wound of a 7-year old patient. This improved her psychological well-being. |
Abstract book EWMA 2014 |
|
9 |
Rijkenberg R [33] |
Published poster of clinical case study |
MMRC made the skin of face and hands of a burn patient more flexible and reduced itching. |
Abstract book EBA 2015 |
Table 1: Available data on MMRC in patients with burns, scars and dry skin.
CONCLUSION
This article shows from available evidence that MMRC (Alhydran®) is a moisturizer which increases skin hydration and reduces abundant TEWL and that these properties may contribute to preservation of an adequate skin barrier function and finally will improve Quality of Life in patients with a disturbed skin barrier function in different pathologies.
CONFLICTS OF INTEREST
Authors did not receive a financial compensation or report any COI.
REFERENCES
- Tortora GJ, Derrickson BH (2011) Principles of Anatomy and Physiology, 13th Edition. John Wiley & Sons, Chichester, UK.
- Beeckman D (2015) Incontinence-associated dermatitis: moving prevention forward. Wound International, London, UK.
- van Smeden J, Bouwstra JA (2016) Stratum Corneum Lipids: Their Role for the Skin Barrier Function in Healthy Subjects and Atopic Dermatitis Patients. Curr Probl Dermatol 49: 8-26.
- Prokosch E, Brash J (2012) Abnormal epidermal barrier in the pathogenesis of contact dermatitis. Clin Dermatol 30: 335-344.
- Eberting CL (2014) Repairing a Compromised Skin Barrier in Dermatitis: Leveraging the Skin’s Ability to Heal Itself. J Allergy Ther 5: 187.
- Kaminer MS, Gilchrest BA (1995) The many faces of acne. J Am Acad Dermatol 32: 6-14.
- Proksch E, Brandner JM, Jensen JM (2008) The skin: An indispensable barrier. Exp Dermatol 17: 1063-1072.
- Bieber T (2010) Atopic dermatitis. Ann Dermatol 22: 125-137.
- Fowler J (2012) Understanding the Role of Natural Moisturizing Factor in Skin Hydration. Practical Dermatology.
- Malajian D, Belsito DV (2013) Cutaneous delayed-type hypersensitivity in patients with atopic dermatitis. J Am Acad Dermatol 69: 232-237.
- Honari G, Maibach H (2014) Skin Structure and Function. Applied Dermatotoxicology.
- Jennemann R, Rabionet M, Gorgas K, Epstein S, Dalpke A, et al. (2012) Loss of ceramide synthase 3 causes lethal skin barrier disruption. Hum Mol Genet 21: 586-608.
- Blaess M, Deigner H-P (2019) Derailed Ceramide Metabolism in Atopic Dermatitis (AD): A Causal Starting Point for a Personalized (Basic) Therapy. Int J Mol Sci 20: 3967.
- Madison KC (2003) Barrier function of the skin: "la raison d'être" of the epidermis. J Invest Dermatol 121: 231-241.
- Mustoe TA (2008) Evolution of silicone therapy and mechanism of action in scar management. Aesthetic Plast Surg 32: 82-92.
- Fonacier LS, Aquino MR (2010) The role of contact allergy in atopic dermatitis. Immunol Allergy Clin North Am 30: 337-350.
- Shaughnessy CN, Malajian D, Belsito DV (2014) Cutaneous delayed-type hypersensitivity in patients with atopic dermatitis: Reactivity to topical preservatives. J Am Acad Dermatol 70: 102-107.
- de Vries CJ, de Witt-de Jong AW, Dirven-Meijer PC, Burgers JS, Opstelten W (2014) [The Dutch College of General Practitioners practice guideline 'Eczema']. Ned Tijdschr Geneeskd 158: 8009.
- Wollenberg A, Barbarot S, Bieber T, Christen-Zaech S, Deleuran M, et al. (2018) Consensus-based European guidelines for treatment of atopic eczema (atopic dermatitis) in adults and children: part I. J Eur Acad Dermatol Venereol 32: 657-682.
- Middelkoop E, Monstrey S (2011) Scar management: Practical guidelines. Maca-Cloetens, Belgium.
- Monstrey S, Middelkoop E, Vranckx JJ, Bassetto F, Ziegler UE, et al. (2014) Updated scar management practical guidelines: non-invasive and invasive measures. J Plast Reconstr Aesthet Surg 67: 1017-1025.
- Chamlin SL, Kao J, Frieden IJ, Sheu MY, Fowler AJ, et al. (2002) Ceramide-dominant barrier repair lipids alleviate childhood atopic dermatitis: Changes in barrier function provide a sensitive indicator of disease activity. J Am Acad Dermatol 47: 198-208.
- Klotz T, Kurmis R, Munn Z, Heath K, Greenwood J (2017) Moisturisers in scar management following burn: A survey report. Burns 43: 965-972.
- Klotz T, Munn Z, Aromataris E, Greenwood J (2017) The effect of moisturizers or creams on scars: A systematic review protocol. JBI Database System Rev Implement Rep 15: 15-19.
- Monstrey S, Pirayesh A, Lambrecht E, Lauwaert S, Verbelen J, et al. (2007) Two years of experience with a new product based on aloe vera for hydration of burn scars. Clinical study presented at the Burn Centre, University Hospital Gent, Gent, Belgium.
- Hoeksema H, De Vos M, Verbelen J, Pirayesh A, Monstrey S (2013) Scar management by means of occlusion and hydration: A comparative study of silicones versus a hydrating gel-cream. Burns 39: 1437-1448.
- Rondas AALM, Schols JMGA (2017) Application of Medical Moisture Retention Cream (ALHYDRAN®), a New Option in the Treatment of Venous Eczema. J Gerontol Geriatr Res 6.
- van Kempen HJ, Dokter J, Oen IMMH ‘Itching, is there a remedy?’ a pilot study with a rehydration gel-cream in burnpatients. Clinical study presented at the European Burn Association (EBA), Budapest, Hungary, 2007, and the International Society for Burn Injuries (ISBI), Montreal, Canada, 2008.
- Ziegenthaler H (2010) Effect of scar treatment products on unpleasant physical manifestations in patients suffering from extensive burn scarring. Clinical study presented at the German-speaking Working Group for Burn Treatment (DAV).
- Ziegenthaler H (2011) Scars after large surface thermal burns - registration of quality of life and therapeutic influence of ALHYDRAN. Clinical study presented at the European Burn Association (EBA).
- Giovannini U (2011) Application of Alhydranin the treatment of pathologic scars after cryoshape. Clinical study presented at the European Burn Association (EBA).
- Ashman S, Kray SJ, Tyne & Wear (2014) Psychological wellbeing - scar. Clinical study presented at the European Wound Management Association (EWMA).
- Rijkenberg R (2015) Use of ALHYDRAN cream in the treatment of burn scars following a chemical explosion - a case study. Clinical study presented at the European Burn Assosiation (EBA).
Citation: van Leen MWF, Hoeksema H, Schols JMGA (2021) MMRC (Alhydran®), an Interesting Treatment Option for a Disrupted Skin Barrier. J Gerontol Geriatr Med 7: 083.
Copyright: © 2021 van Leen MWF, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

