
Much More Than a Dental Problem!
*Corresponding Author(s):
Tânia MendoDepartment Of Pediatrics, Hospital José Joaquim Fernandes, Unidade Local De Saúde Do Baixo Alentejo, Beja, Portugal
Tel:+351 284310200,
Email:mendotania.tfdsm@gmail.com
Abstract
A teenager presents to the emergency department with a jaw mass after 3 months of multiple unsuccessful courses of antibiotics. On physical exam, a mandibular mass was evident with no other significant changes. CT scan showed a soft tissue mass suggestive of a slow-growing tumor and biopsy revealed an ameloblastoma (plexiform type). Surgical excision was performed with later reconstruction and full recovery was achieved six months later.
Jaw masses which fail to respond to antibiotic therapy should trigger imaging investigation, as neoplasms in early stages might be confused with dental abscesses, delaying adequate treatment.
CASE REPORT
A 17-year-old male teenager, previously healthy, with a smoking habit for the past 5 years, presents to the emergency department with a jaw mass starting 3 months before, associated with a progressive dysphagia for solids, but no history of fever or trouble breathing. He had already been treated twice with antibiotics admitting a dental abscess, with no success. The physical examination revealed a painful mandibular mass of stone consistency on the left side, measuring approximately 7 cm, with no inflammatory signs or adenopathies (Figure 1). He also had poor oral hygiene with multiple dental caries.

Figure 1: Teenager with the mandibular mass.
Initial ultrasound showed a deep bulky non-pure liquid collection, compatible with an abscess but CT scan eventually revealed a soft tissue mass in the left hemimandible measuring 60x60x40 cm, bone expansion with cortical reduction, without periosteal reaction, suggestive of slow-growing tumor (Figure 2). Incisional biopsy disclosed an ameloblastoma (plexiform type). Left hemimandibulectomy with condyle conservation and reconstruction with microanastomosed free flap of peronium was perfomed. Full recovery with physical therapy was achieved six months after.
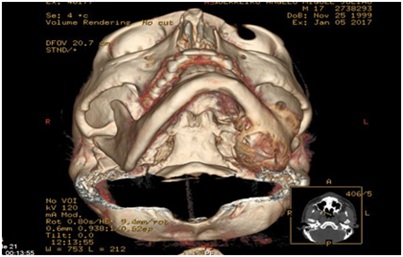
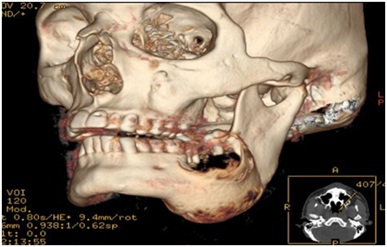 Figure 2: CT scans showing the mandibular tumor.
Figure 2: CT scans showing the mandibular tumor.
DISCUSSION
Initial stages of jaw tumors usually present with a swelling or mass which can lead to being easily mistaken by infections and treated accordingly at first. Following unresponsive antibiotic therapy, additional investigation with imaging is set in motion, revealing a radiolucent or radiopaque lesion in the jaw and prompting a tissue diagnosis in order to correctly assess the best treatment [1]. A slow growing mandibular mass without gross elevation of the inflammatory parameters should lead to suspect a neoplasm since odontogenic abscesses have a much more exuberant course.
Primary jaw neoplasms are broadly classified into odontogenic and nonodontogenic groups [2]. The incidence of nonodontogenic tumors is twice that of odontogenic ones.
The odontogenic tumors are rare, constituting < 1% of oral tumors and they are classified according to their epithelial, mesenchyme and mixed origin [3]. The unicystic ameloblastoma is a benign odontogenic tumor most frequently found in adolescents but the ameloblastoma (plexiform, desmoplasic, granular, acanthomathous and basaloid) is most common diagnosed in the fourth and fifth decades of live [3]. They are both of epithelial origin but different entities with different incidences and prognosis. Ameloblastoma, although rare, benign and a slow growing tumor is locally aggressive and highly recurrent. Incisional biopsy is the gold standard for histopathologic diagnosis, after which radical surgical intervention with at least 10mm of margin is required for eradication of disease. After the resection, advanced reconstructive procedures are needed to restore the function and form of the jaws [4]. Regarding children, craniofacial growth must be taken into account for the surgical excision and later reconstruction.
CONCLUSION
Jaw masses which fail to respond to antibiotic therapy should trigger imaging investigation, as neoplasms in early stages might be confused with dental abscesses, delaying adequate treatment. This delay often leads to a much more difficult resection and complex reconstruction techniques due to the size of the tumor.
AUTHOR DISCLOSURE
Drs Mendo, Borges, Mateus and Seves have disclosed no financial relationships relevant to this article. This commentary does not contain a discussion of an unapproved/investigative use of a commercial product/device.
REFERENCES
- Saxena S, Kumar S, Pundir S (2012) Pediatric jaw tumors: Our experience. J Oral Maxillofac Pathol 16: 27-30.
- Kaban LB, Steinberg B, Troulis MJ (2004) Pediatric oral and maxillofacial surgery, (2nd edn). Philadelphia: Saunders, Pennsylvania, United States. Pg no: 212-245.
- El-Naggar AK, Chan JKC, Grandis JR, Takata T, Slootwe PJ (2017) WHO classification of head and neck tumours. Fourth edition. International agency for research of cancer. Pg no: 9.
- Perry KS, Tkaczuk AT, Caccamese JF, Ord RA, Pereira KD (2015) Tumors of the pediatric maxillofacial skeleton: A 20-year clinical study. JAMA Otolaryngol Head Neck Surg 141: 40-44.
Citation: Mendo T, Borges C, Mateus C, Seves G (2020) Much More Than a Dental Problem! J Neonatol Clin Pediatr 7: 044.
Copyright: © 2020 Tânia Mendo, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

