
Multiple Phases of the Decline of Platelet Recruitment after Interventional Injury of Angioplasty and Coronary Artery Bypass Graft Surgery in the Animal Model
*Corresponding Author(s):
Mrinal Kanti DewanjeeRetired Professor, Department Of Radiology, Pathology, Mayo Clinic, Rochester, Minnesota 55905 And Emeritus Special Volunteer, NEI, NIH, Bethesda, Maryland 88902, United States
Email:mrde20841@verizon.net
Although the platelet thrombus in the coronary, cerebral and peripheral artery systems is the number one killer, there is no clinically relevant platelet biomarker for this devastating pathology, since the discovery of blood circulation in a closed by William Harvey (1628, De Motu Cordis) and the triple synergistic effects of I. Hypercoagulability of blood viscosity, II. Blood flow stasis-flow disturbance and III. Arterial wall injury from the loss of endothelial cells as in Rudolf Virchow’s Triad resulting in the deep vein thrombosis (DVT) and arterial platelet thrombus formation in 1856. Out of ~60,000 miles of arteries, veins and capillary network in the human circulatory system, the coronary artery system of narrow arteries (~2-5 mm ID) with multiple branching, twisting and higher shear force is the most vulnerable ~25 cm component. Clinicians still use the International Normalized Ratio (INR) involving the extrinsic and common coagulation pathway for the effectiveness of drug therapy in the affected patients. In the absence of any critical biomarker of thrombogenicity during almost 120 years for a thrombotic heart attack and stroke, I developed the first parameter of regional platelet density (RPD) in the adherent platelet thrombus (APT) in 1978 in the canine model coronary of left anterior descending (LAD) artery bypass graft surgery. In 1976, when I joined as the first Bengali Staff Consultant, Associate Professor of Pathology and Director of Radiopharmaceutical Laboratory at Mayo Clinic with an assembly 780 staff consultants, it was the right place at the right time with 275 consultants in the cardiovascular diseases, to solve this perennial puzzle of slippery pathology of arterial platelet thrombus. The cardiovascular surgical research lab with the excellent staff members, equipment for monitoring, anesthesia for open heart surgery and the Institute Hills Farm, a few miles away for the recuperation after critical surgery of large animal models provided an ideal facility.
From the platelet counts per ml of radioactive blood and area of conduit-injury (cm2) and APT radioactivity, I developed an algebraic equation for converting the APT into total number of platelets and normalized this value per unit 2 (remove 2) area, an ideal and universal index of thrombogenicity for biomaterials in cardiovascular prostheses and ranking of all anti-platelet drugs, aspirin (Inhibitor of Cycloxinase1 preventing synthesis of Thromboxane A2), Clopidogril, precursor of Plavix (P2Y12, Adenosine Diphosphate (ADP) receptor blocker), Persantine, (Phosphodiesterase inhibitor), Ibuprofen, Prostacyclin, etc. routinely today. Injury and occlusion level are so intense that we have to use two anti-platelet blockers simultaneously for maintaining patency post angioplasty in the porcine model (Plavix and aspirin) and CABG surgery (Persantine and aspirin) in the canine model. We also provided the latest optimized values of platelet survival times (Exponential, Linear and MultiHit models) in the canine, porcine and human platelets in healthy volunteers at Mayo Clinic and continuously supported by the Mayo Foundation.
The rate of Reduction of Platelet Recruitment (RPR) is an index of progression of wound-healing after the essential interventional procedure of angioplasty and CABG for recanalizing or bypassing the segment of occluded artery and effectiveness of antiplatelet drug therapy in the animal models. After the analysis of regional platelet density (RPD: millions of platelets/cm2) in an adherent thrombus after Coronary Artery Bypass Surgery (CABG) and angioplasty for retaining the myocardial reperfusion, we observed that the RPR occurs in two to three phases with definite half-life values. The areas of injury from angioplasty and the anastomosis in CABG surgery are the specific sites for platelet recruitments for thrombus formation. The Regional Platelet Density (RPD) at proximal and distal anastomoses (PA and DA) showed three distinct values of declining radioactivity with half-lives of (30 ± 5), (50 ± 10) and (500 ± 50) hours, a tri-exponential curve. The mid-graft segments showed a bi-exponential curve with half-life values of (15 ± 5) and (150 ± 15) hours. Comparative thrombogenicity measurement of platelets from canine, porcine and human blood, suggested that canine platelets are 3-times more thrombogenic, porcine platelets are 1.5-times more than human platelets [8]. I also estimated that 50-150 million platelets could occlude the human coronary artery system (2-4 mm, ID), which might be partially occluded by crystals of cholesterol and hydroxyapatite in the ruptured cholesterol plaque. These RPR values might be 2-3-times longer in the human patients due to lower level of platelet reactivity y, longer half-life of human platelets: Exponential model-human (5.4 ± 0.7) days, pigs (50 ± 2) and dogs (35 ±3) hours and slower healing time. Due to invasive nature of the direct sampling for regional radioactivity and specific injured areas, these measurements could not be performed in the human patients [1,6,13,14].
One of our concerns was the reproducibility of retention of platelet aggregates of different sizes and the process of continuous embolization of radioactive thrombi. However, I focused on the thrombus-directed dissection of the 2-3 mm segments of proximal and distal anastomoses, where the RPD was much higher and suturing injury. For angioplasty, we cut the central single segment of highest level of injury and highest level of radioactivity and suturing injury. For angioplasty, we cut the central single segment of highest level of injury and highest level of radioactivity. We observed that at 24 hours, there was some degree of equilibrium, where the retained thrombus-adherent radioactivity had lower values of standard deviation. In vitro flow chamber studies suggested that the SD values were much lower at later periods. Hence, we euthanized the animals for both CABG and angioplasty at 24 hours after injection of 300-400 microcuries of 111In-tagged platelets. Autologous platelets of the dogs were labeled with 111In-(tropolone)3 according to the method of Dewanjee et al. [1-3]. Five animals were included in each group at 24 hours, 3-, 7-, 30- and 90 days for the CABG group. Before euthanasia with IV barbiturate solution, we heparinized the animals at 4 mg/kg for the reduction of post-mortem thrombus formation. The harvested CABG angioplasty segment was rinsed with saline from loosely bound radioactivity. The area of five segments was measured by spreading the segments on the graph paper (Keuffel & Esser Co.) with 2-dimensional linear grids. The total number of squares and total area were evaluated with a microscope. The window of gamma counter spectrometer was adjusted to cover both the 174-keV and 247-keV sum peaks of the 111In radioisotope. After measuring the radioactivity with a calibrated gamma counter (Beckman Inc. CA), we calculated the radioactivity (counts/min). Using the algebraic equation, we converted the radioactivity into the number of platelets for each segment and blood sample before euthanasia. This platelet number (million) value was normalized per unit area (cm2). The details of these measurements are described by Dewanjee, et al. [3-13,16].
Equations For The Half-life Values Of Declining Rate Of Platelet Recruitment (PR) On The Segments Of Injured Artery And Saphenous Vein Post-intervention: CABG Surgery Vs. Angioplasty
In the multi-radionuclide decays, we used the curve-stripping method and the semi-log plot for the estimation of half-lives of their decays of multiple radionuclides. As in the radioactive decays, the platelet recruitment on the segments of injured wall is a random process and the decline of platelet recruitment is proportional to the total number of recruited platelets, RPDs. Hence, I used the following equations for the calculation of multiple phases of declining rate of average platelet recruitments with time post-surgery time t0,
-d(RP)n/dt = (λn)xRPD, d(RP)t = d(RP)0xe-λt and (t1/2)n = 0.693/λn
where λn is the slope-constant for each phase PR declining rate for the half-life values (t1/2)n of declines of platelet recruitments.
I used the Excel spreadsheet for the preliminary analysis of RPD database and (t1/2)n values. Finally, I requested my colleague, Dr. Ratan Debnath, a computer scientist at NASA for the semi-logarithm color plot of my RPD database saved in a aged notebook in my personal golden archive as shown in Figure 2, where the logarithm of regional platelet density was plotted in the ordinate, Y-axis and the time after surgical injury in the X-axis [6,7]. I was gratified to find the dual and triple phases of PR in the superficial injury and triple phase of PR in the deep-wall injury of anastomosis in both proximal and distal anastomoses or medial tear in angioplasty. These RPD values for focal segment angioplasty are similar to that of PA and DA sites with a tri-exponential curve (Figures 1&2). The equation describing the calculation of regional platelet density was detailed and the decrease of logarithm of RPD values with time post CABG surgery in the control and Persantine (55 mg)-aspirin (325 mg) therapy groups was shown in Figure 1.
The platelet thrombus kills annually about 20 million victims worldwide by damaging the heart muscle. The clinicians never describe the pathology of killer thrombi in terms of number of platelets, although we published the original article in Circulation 1964. The editorial board delayed the printing for prolonged revisions. Finally, I described the uncertainty principle that we could not measure without some disturbance of platelet function. I am giving the clinicians a lifeline for the direct extrapolated values of 50-150 million activated platelets that could occlude the human coronary artery system (2-4 mm, ID), rather than hiding behind the INR values above 2.5 for avoiding thromboembolic events in future after angioplasty and CABG surgery.
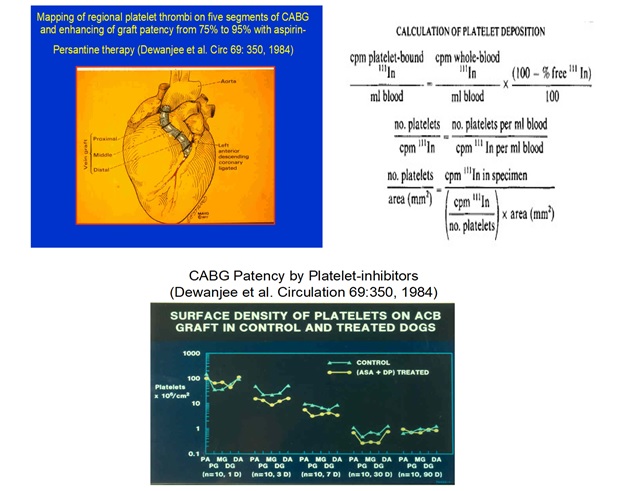 Figure 1: The CABG surgery in the canine model, the Algebraic equations for the calculation of regional platelet density and the chronological loss of platelet recruitment with time after intervention [3,16] in the control and aspirin-Persantine treated dogs. Effect of treatment significantly decreased the thrombus level till 30 days post CABG. No difference on platelet density was observed after the wound-healing phase at 90 days, when the inner lumen was completely re-endothelialized and dual anti-platelet therapy may not be needed.
Figure 1: The CABG surgery in the canine model, the Algebraic equations for the calculation of regional platelet density and the chronological loss of platelet recruitment with time after intervention [3,16] in the control and aspirin-Persantine treated dogs. Effect of treatment significantly decreased the thrombus level till 30 days post CABG. No difference on platelet density was observed after the wound-healing phase at 90 days, when the inner lumen was completely re-endothelialized and dual anti-platelet therapy may not be needed.
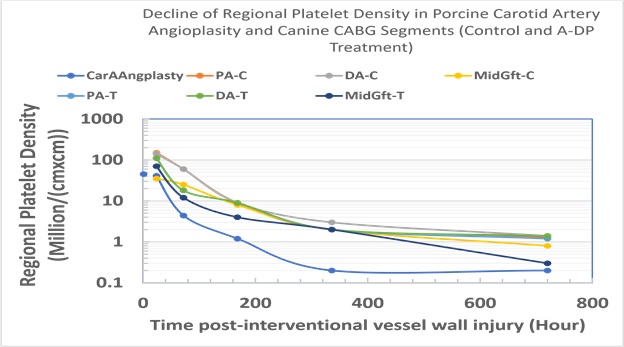 Figure 2: The curve-stripping method along with the semi-log plot for the estimation of half-life of reduction of platelet recruitment at the sites of interventional injury of vessels post angioplasty and CABG surgery. Three half-life values of reduction of platelet recruitments (RPR) were observed for segments angioplasty with occasional medial rupture injury values and at the anastomoses of distal and proximal anastomoses of CABG surgery. Two half-life values of decline of RPR were measured at the mid-segments of CABG surgery, where severe loss endothelial cells from saphenous vein during harvesting and suturing injury with six stitches of thinner prolene-sutures.
Figure 2: The curve-stripping method along with the semi-log plot for the estimation of half-life of reduction of platelet recruitment at the sites of interventional injury of vessels post angioplasty and CABG surgery. Three half-life values of reduction of platelet recruitments (RPR) were observed for segments angioplasty with occasional medial rupture injury values and at the anastomoses of distal and proximal anastomoses of CABG surgery. Two half-life values of decline of RPR were measured at the mid-segments of CABG surgery, where severe loss endothelial cells from saphenous vein during harvesting and suturing injury with six stitches of thinner prolene-sutures.
Summary
Our studies on regional platelet recruitment (RPR) in the acute phase of 600 hours after interventional injury post Angioplasty and CABG surgery in the animal models indicated that RPR decreased continuously with time as the wound-healing progressed from the loss of endothelial cells and the rupture of coronary artery after angioplasty. A new technique was developed by plotting the logarithm of absolute value regional platelet density on the sites of anastomoses of distal and proximal anastomoses of saphenous vein (SV) to aorta at PA and SV to coronary artery at DA and serious focal injury at the site of angioplasty. Dual and triple phase of decline of RPR were calculated for serious and moderate level of wall injuries. Considering the possibility of platelet thrombus formation on injured wall, dual anti-platelet medications are recommended in the acute phase. From several canine surgical models 50-70, 80-100, About 50-70, 80-100, and 140-150 million platelets could occlude the 2-, 3-, and 4-mm lumen of the coronary artery system. Considering the similarity of interaction of integrin GPIIb-IIIa of activated platelets with deendothelialized collagen surface, with certain lower intensity of platelet reactivity and platelet survival time in canine, porcine and human, for the first time the clinicians, cardiovascular surgeons and cardiologists could use these real values of the thrombo-kinetics and decline of platelet recruitment half-live values after some degree of extrapolation to human interventional injury sites. Even now, clinicians refer to the INR values of prothrombin time ratio involving the extrinsic and common pathway for the effectiveness of anti-platelet or Coumadin therapy for the inhibition of thromboembolic complications in a patient with a mechanical heart valve or other cardiovascular prostheses. For the clinical evaluation of anti-platelet drugs in human patients with synthetic vascular grafts, I obtained several INDs from FDA after carrying out the radiation dosimetry studies and human imaging with my mentor, colleague with a brilliant mind, James S. Robertson [14,15]. Jim used to call me the Book-keeper of platelets and generously checked my equations and methods of evaluations.
Acknowledgement
These challenging experiments were only possible from the unique combination of skilled dedicated staff, analytical machines, imaging machines, animal facilities and immense prolonged funding at Mayo Clinic, Commercial industries and NIH. The animal care, laboratory medicine and radiation safety committees permitted the use of large amount of radioactive tracers at millicurie level for understanding the mechanism of platelet thrombus formation with 111In-tagged platelets and 125Iodine-tagged fibrinogen, quantitative measurement of their half-life values, fibrin/platelet ratios, total consumption of platelets after open-thorax surgery using heart-lung machines for CABG surgery and heart valve implantations, and platelet counts with radioactive blood with the Coulter counter. An experimental gamma camera fitted with the medium energy parallel-hole collimator from Searle, Inc. and X-ray machine facilitated the imaging of live animals and distributions of radioactivity of organs after euthanasia at all time periods. Dr. Dwight McGoon and medical and surgical staff believed in my equations and principle of in vivo qualitative and in vitro quantitative measurements. Dr. McGoon asked for my autograph on the NYAS review article, I provided for his comments [9].
We appreciated the assistance of James A. Rosemark, O. Arlan Hildestat and John C Ritter. Paul E. Zollman, VMD, Veterinarian Extraordinaire, took great care of animals after major surgeries. However, several dogs after CABG surgery died from arrythmia induced by exposure to cold weather during transportation from Medical Science building to Institute Hills Farm. In 1976, VD Fuster, MD, asked for my assistance in the book-keeping of platelets in animal models and the patients at Mayo Clinic, offered me the NHLBI funds and suggested the study of the measurement of platelet thrombus on CABG segments in the canine model. I still wonder, why Valentin, the Smart Cardiologist did not ever refer to our unique publication related to the original article in Circulation, 1984 in any of his publications, Wikipedia and Lecturers of CEO of Mount Sinai Fuster Heart Center, AHA President and the acceptance speech of Spanish Duke-Marquee???. Michael P Kaye, MD and his skilled surgical residents, Mamuro Tago, Miguel Josa, Peter Steele, Jules YT Lam, Eduardo Solis, carried out the single LAD vessel-CABG surgery in the Cardiovascular Surgical Research laboratory. Peter Steele and James Chesebro carried out the evaluation of the parameters of optimization of angioplasty in the porcine model. Generous funding was provided by the Mayo Foundation and NHLBI Grant-HL24602.
Dedication to Animals-Small and Large
In addition, I want to dedicate my publication of collective wisdom to the hundreds of small and large animals, euthanized for understanding the mechanism, pathology, drug therapy, animal models: mice, rats, rabbits, monkeys, dogs, pigs and cows at Brigham and Children's Hospital, Tufts-New England Medical Center, Mayo Clinic, University of Miami, School of Medicine, Florida, Urbana-Champaign@UIUC, Illinois, CBER, FDA and finally NEI, NIH, Bethesda, Maryland during the prolonged pains-taking and costly studies from 1971-till 2005. I was grateful for the 25-year funding from NHLBI. Once we developed the tools and technologies, the drug and device corporations provided kilogram of drugs, Persantine (Behringer-Ingelheim, Inc.), Ibuprofen, Amino-diphosphonate (Henkel, Inc.). Baxter Inc. provided the costly circuits of heart-lung machines and Shiley, Inc. provided the mechanical and tissue heart valves gratis for several decades.
References
- Dewanjee MK (2021) Measuring and Imaging the Arterial Platelet Thrombus: Saving Lives by Rapid Intervention with Drugs, Devices and Genetics, in Heart Attack and Stroke: Saving Lives with Drugs, Devices and Genetics, Sole Author, 1-554 pages, iUniverse, Bloomington, Indiana, USA. Chapter 6. Labeling of Platelet Survival Times in Human Healthy Volunteers with three Tracers: 51Cr-, 111In-oxine and In-111 tropolone tagged platelets using the Linear, Exponential and Multi-Hit Models. pp 139-143. A twenty-five-year study at Mayo Clinic.
- Dewanjee MK, Rao SA, Didisheim P (1981) Indium-111 tro-po-lone, a new high-affinity platelet label. Preparation and evaluation of labeling parameters. J Nucl Med 22: 981-987.
- Dewanjee MK, Tago M, Josa M, Fuster V, Kaye MP (1984) Quantification of platelet retention in aortocoronary femoral vein bypass graft in dogs treated with dipyridamole and aspirin. Circulation 69: 350-356. First paper describing the measurement of the unique and universal biomarker of regional platelet density on CABG segments in 1978 that revolutionized the Thrombometry in the Cardiovascular Medicine. My Eureka moment!!!.
- Steele P, Chesebro JH, Stanson AW, Dewanjee MK, Fuster V, et al. (1985) Balloon angioplasty. Natural history of the pathophysiological response to injury in a pig model. Circulation Research 57: 105-112.
- Dewanjee MK, Fuster VD, Kaye MP, Rosemark JA, Chesebro JH, et al. (1982) Evaluation of platelet-inhibitor drugs in a canine bilateral femoral graft implant model. Trans ASAIO 28: 504-509.
- Lam JYT, Chesebro JH, Steele PM, Dewanjee MK, Badimon L, et al. (1986) Deep arterial injury during experimental angioplasty: Relationship to a positive platelet scintigram, Quantitative platelet deposition and mural thrombus. J Am Coll Cardiol 8: 1380-1386.
- Solis E, Hollier LH, Plate G, Dewanjee MK, Kaye MP (1986). Early and late comparison of umbilical vein and PTFE grafts in control and piroxicam-treated dogs. International Angiology 5: 73-78.
- McCarthy PM, Schaff HV, Bank H, Dewanjee MK (1988). Cryopreserved internal mammary artery bypass: Studies of platelet and fibrinogen deposition and graft patency. Surgical Forum XXXIX : 333-334.
- Dewanjee MK (1987). Methods of Assessment of Thrombosis in vivo. Ann N Y Acad Sci 516: 541-571.
- Dietrich WD, Dewanjee S, Prado R, Watson BD, Dewanjee MK (1993). Transient platelet accumulation in the rat brain after common carotid artery thrombosis: An 111In-labeled platelet study. Stroke 24: 1534-1540.
- Dewanjee MK, Kapadvanjwala M, Zilleruelo G, et al (1992) Quantitation of comparative thrombogenicity of dog, pig and human platelets in a hemodialyzer. ASAIO JOURNAL 88-90.
- Dewanjee MK, Kapadvanjwala M, Cavagnaro CF, et al. In vitro and in vivo evaluation of the comparative thrombogenicity of cellulose acetate hemodialyzers with radiolabeled platelets (1994). ASAIO J 40: 49-55.
- Didisheim P, Dewanjee MK, Frisk CS, Kaye MP, Fass D (1984). Animal models for predicting clinical performance of biomaterials for cardiovascular use. Contemporary Biomaterials. Material and Host Response, Clinical Applications JW Boretos, M Eden (Eds.), New Technology and Legal Aspects, Noyes Publications, Park Ridge, NJ, USA, pp. 132-179.
- Robertson JS, Ezekowitz MD, Dewanjee MK, Lotter MG, Watson EE (1992). Radiation absorbed dose estimates for radioindium labeled autologous platelets. Accepted for publication. JOURNAL OF NUCLEAR MEDICINE 33: 777-780 (MIRD Dose Estimate No. 15).
- Dewanjee MK, Wahner WH, Dunn WL, Robertson JS, Offord KP, Fuster VD, Chesebro JH (1986). Comparison of three platelet markers for measurement of platelet survival time in healthy volunteers. Mayo Clinic Proceedings 61: 327-336.
- Dewanjee MK. Wound-Healing in the Saphenous Vein Coronary Bypass Graft in the Canine Model: Endothelial Cell Loss, Platelet Thrombus Formation, its Inhibition with Aspirin-Persantine Therapy and Cholesterol Influx in the Acute and Chronic Phase. J Angiol Vasc Surg 5: 037, 2020. (DOI:10.24966/AVS-7397/100037.)
Citation: Dewanjee MK (2025) Multiple Phases of the Decline of Platelet Recruitment after Interventional Injury of Angioplasty and Coronary Artery Bypass Graft Surgery in the Animal Model. J Angiol Vasc Surg 10: 132.
Copyright: © 2025 Mrinal Kanti Dewanjee, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

