
Neuropsychological Assessment and Determination of Activities of Daily Living, the Role of Memory and Spatial Tasks in Mild Cognitive Impairment
*Corresponding Author(s):
Rogério Paulo Dos Santos HenriquesDepartamento De Desporto E Saúde, Escola De Saúde E Desenvolvimento Humano, Universidade De Évora, Largo Dos Colegiais, Évora, Portugal
Tel:+00351 914318089,
Email:rogeriopaulohenriques@gmail.com
Abstract
Objectives: The aim of this study was to explore the relationship between performance in neurocognitive variables and daily functioning in older adults with Mild Cognitive Impairment (MCI).
Methods: A sample of 157 participants with MCI aged 60-90 completed a battery of tests, including the Dementia Rating Scale (DRS), Rey-Osterrieth Complex Figure (ROCF), Trail Making Test (TMT) and scales for assessing basic (b-ADL) and instrumental Activities of Daily Living (i-ADL). T-tests and logistic regression were used for data analysis.
Results: Scores on the DRS-Attention (DRS-A) increased the probability of the participants being dependent (OR: 2.4) according to the b-ADL. Scores on the DRS-Memory (DRS-M) (OR: 2.8), ROCF Reproduction (OR: 3.0) and TMT-A (OR: 4.4) increased the probability of the participants being dependent according to the i-ADL. A final model was created including these three tests, which indicated that the DRS-M was the most relevant, increasing the probability of being dependent according to the i-ADL (OR: 3.0).
Conclusion: Our study shows that memory and visuospatial tasks predict being dependent according to the i-ADL and that attention predicts being dependent according to the b-ADL. Additionally, the i-ADL seems to be more sensitive to the effects of cognitive decline. These results point to the need to invest in programs that prevent attention, memory, processing speed and visuospatial decline with effects on performance in everyday functioning.
Keywords
Attention; Daily functioning; Memory; Mild cognitive impairment; Visuospatial tasks
Introduction
Research on the decline in performance of Activities of Daily Living (ADL) has increased in recent years due to population aging. Additionally, difficulties in instrumental ADL (i-ADL) seem to be associated with Mild Cognitive Impairment (MCI) [1]. Cognitive impairment appears in the literature to be associated with MCI and is related to i-ADL [2]. The use of technology [3], medication management, telephone use, consultation management, finding things at home, and financial management [4] are among the most severely affected i-ADLs in patients with MCI. The magnitude of the defect in ADL seems to be more severe in those abilities that depend on memory [5]. The incidence rate of MCI with and without memory impairment is 3.8% and 3.9%, respectively [6]. Other studies report that these values can vary between 5.0% and 36.7%, and increase with the age of the population [7]. Memory assessment, namely delayed recall, has emerged as a good neuropsychological predictor of MCI [8].
Visuospatial skills are also associated with changes in cognitive measures in advanced age [9]. Spatial ability is essential for functional independence and has emerged as an important factor in the diagnosis of MCI. The performance in visuomotor and graphomotor tasks remains preserved in normal aging, although the time of accomplishment increases [10]. In this way, impairment of visuospatial skills is a potential diagnostic and prognostic indicator for neurological degeneration [11]. It could be possible to anticipate rehabilitative interventions for people with MCI if we have a better understanding of their neuropsychological profile and daily functioning [12]. Additionally, we can create more effective rehabilitation approaches by being informed by the neuropsychological assessment results. For practitioners, it is relevant to identify a reduced battery of neuropsychological tests that can predict ADL difficulties. We suggest, therefore, the hypothesis that the application of the Dementia Rating Scale (DRS), in conjunction with others of wide application, namely the Rey-Osterrieth Complex Figure (ROCF) and Trail Making Test (TMT), can predict the daily functioning level of elderly adults with MCI. The DRS [13,14], TMT [15] and ROCF [16] have been indicated as screening tools for indicating the need for a thorough assessment of cognitive state and ADL in elderly people with neurocognitive disorders. On the other hand, TMT and ROCF measure specific neuropsychological skills and are common clinical instruments in full neuropsychological batteries in order to provide information regarding executive function and visuoconstructional abilities. To our knowledge, there is no information on how the combination of these three tests can be reported for basic (b-ADL) and i-ADL. Therefore, the aim of this study is to explore the relationship between daily functioning and performance on the DRS-2, TMT and ROCF in older adults with MCI. Specifically, it examines how these tests contribute to the prediction of dependence as assessed by the b-ADL and i-ADL.
Materials and Methods
A total of 157 participants were selected [1] following the inclusion criteria: adults over 60 years old, average values between questionable and mild impairment (154 participants: score 0.5; 3 participants: score 1.0) on the Clinical Dementia Rating, and being diagnosed with MCI according to the criteria presented in the DSM-5. The study was approved by the Ethics Committee of the University of Évora (ref: 12271) and followed the Declaration of Helsinki. All participants signed the informed consent form. The collection of cognitive and functional data was carried out over two sessions, with a duration of about one hour each. In the first session, all participants completed the Katz index [17] (b-ADL) and the Lawton-Brody scale [18] (i-ADL) in the presence of a caregiver who assisted. The Katz index evaluates six activities considered basic in everyday life: washing, dressing, using the toilet, mobility, being continent and eating. A score of 6 indicates independence and higher values indicate dependence. The i-ADL assesses the level of independence of the elderly person regarding instrumental activities and comprises eight tasks: ability to use the phone, shopping, food preparation, housekeeping, laundry, mode of transportation, responsibility for own medication and the ability to handle finances. A score of 8 indicates independence, and higher scores reflect poorer performance.
In the second session, all participants completed the DRS, ROCF and TMT; only the interviewer was present. The DRS [19] consists of five subscales: Attention (DRS-A), Initiation/Perseveration (DRS-IP), Construction (DRS-Const), Conceptualisation (DRS-C) and Memory (DRS-M). The ROCF allows the assessment of perceptual activity and visual memory [20]. The application takes place firstly in the presence of the figure. Soon after, with an interval of time not exceeding 3 minutes, a reproduction is made from memory. The total score is calculated as the sum of the points achieved by the subject. The TMT has two parts: TMT-A, which measures attention, visual perception, and visuo-motor speed and information processing; and TMT-B, which evaluates working memory and executive functions [21]. The result is calculated as the number of seconds required to complete the task. Higher scores reflect better performance on the DRS and ROCF and poorer performance in the TMT.
Normality of the data was analysed using the Kolmogorov-Smirnov test. Initially, a descriptive analysis of demographic and clinical characteristics was carried out. Logistic regressions were computed to examine which neuropsychological variables contribute significantly to b-ADL and i-ADL scores. We developed four linear regression models, and for each model, b-ADL and i-ADL were considered separately as dependent variables. The independent variables were all scales of DRS (model-1); performance in ROCF scales (model-2); performance in TMT scales (model-3) and a final model (model-4) in which all the significant variables detected in the previous models were included. For b-ADL, model 4 was not used because there was only one scale with predictive value. Statistical analyses were performed using the statistical package SPSSv.24 (IBM, New York, USA). For all tests, the significance level was set at p < 0.05.
Results
Demographic and clinical data from the participants are summarised in table 1. The sample was drawn from a rural population where the level of education was low.
|
|
Mean±Standard Deviation |
|
Gender (male/female) |
50/107 |
|
Age (years) |
73.66 ± 7.57 |
|
Schooling (years) |
5.84 ± 3.27 |
|
CDR |
0.51 ± 0.07 |
|
b-ADL Katz Index |
6.42 ± 0.96 |
|
i-ADL Lawton & Brody Scale |
10.71 ± 2.61 |
Table 1: Demographic and clinical characteristics.
CDR: Clinical Dementia Rating Scale; basic activities of daily living Katz Index; instrumental activities of daily living Lawton & Brody Scale.
For the b-ADL, the most strongly impaired subdomains were transferring (seven participants with mild and two with a moderate level of dependence) and continence (34 mild, two moderate). For the i-ADL, 29.9% of people reported having mild and 1.3% moderate difficulty in using the telephone; shopping (38.9% mild, 1.3% moderate); food preparation (34.4% mild, 5.7% moderate); housekeeping (27.4% mild, 5.1% moderate and 0.6% severe); laundry (24.2% mild, 0.6% moderate); mode of transportation (27.4% mild, 1.9% moderate and 0.6% severe); responsibility for own medications (47.8% mild) and ability to handle finances (4.5% mild). To assess the significance of neuropsychological variables on the probability of being dependent in daily functioning, binary logistic regressions were performed using the Enter method. Regarding b-ADL (Table 2), we found the following statistics describing the models: model-1 [X2 (6)=7.437; p = 0.279, R2 Nagelkerke=0.068]; model-2 [X2 (2)=2.106; p = 0.349, R2 Nagelkerke=0.022]; and model-3 [X2 (2)=0.432; p = 0.806, R2 Nagelkerke=0.006].
|
|
|
Beta |
OR |
CI 95% |
P value |
||
|
Model 1 |
DRS-A DRS-IP DRS-Const DRS-C DRS-M DRS-T |
0.914 0.473 0.482 0.199 0.584 -0.598 |
2.493 1.605 1.620 1.220 1.792 0.550 |
1.082-5.743 0.677-3.804 0.636-4.126 0.506-2.942 0.704-4.562 0.189-1.602 |
0.032 0.283 0.312 0.658 0.221 0.273 |
|
|
|
Model 2 |
ROCF Reproduction |
0.527 |
1.694 |
0.540-5.316 |
0.366 |
|
|
|
|
ROCF Memory |
0.419 |
1.521 |
0.368-6.289 |
0.563 |
|
|
|
Model 3 |
TMT-A TMT-B |
0.179 -0.301 |
1.196 0.740 |
0.460-3.111 0.292-1.876 |
0.713 0.526 |
|
|
Table 2: Logistic regression analysis applied in order to estimate the effect of neuropsychological aspects on b-ADL Katz Index.
DRS-A: Dementia Rating Scale Attention; DRS-IP: Dementia Rating Scale Initiation/Perseveration; DRS-Const: Dementia Rating Scale Construction; DRS-C: Dementia Rating Scale Conceptualization; DRS-M: Dementia Rating Scale Memory; DRS-T: Dementia Rating Scale Total; ROCF: Rey-Osterrieth Complex Figure; TMT: Trail Making Test.
The statistics regarding i-ADL are shown in table 3: model-1 [X2 (6)=21.663; p = 0.001, R2 Nagelkerke=0.199]; model-2 [X2 (2)=8.874; p = 0.012, R2 Nagelkerke=0.093]; model-3 [X2 (2)=9.403; p = 0.009, R2 Nagelkerke=0.116]; and model-4 [X2 (3)=18.935; p < 0.001, R2 Nagelkerke=0.205].
|
|
|
Beta |
OR |
CI 95% |
P value |
||
|
Model 1 |
DRS-A DRS-IP DRS-Const DRS-C DRS-M DRS-T |
0.300 0.351 2.033 0.695 1.048 0.121 |
1.350 1.420 7.637 2.004 2.851 1.128 |
0.462-3.942 0.509-3.963 0.957-60.967 0.634-6.336 1.067-7.618 0.333-3.819 |
0.583 0.503 0.055 0.236 0.037 0.846 |
|
|
|
Model 2 |
ROCF Reproduction |
1.114 |
3.047 |
1.140-8.142 |
0.026 |
|
|
|
|
ROCF Memory |
0.487 |
1.627 |
0.508-5.212 |
0.412 |
|
|
|
Model 3 |
TMT-A TMT-B |
1.485 0.241 |
4.414 1.272 |
1.361-14.318 0.505-3.203 |
0.013 0.610 |
|
|
|
Model 4 |
DRS-M |
1.119 |
3.063 |
1.241-7.559 |
0.015 |
|
|
|
ROCF Reproduction |
0.831 |
2.296 |
0.853-6.184 |
0.100 |
|
||
|
TMT-A |
0.983 |
2.672 |
0.942-7.582 |
0.065 |
|
||
Table 3: Logistic regression analysis applied in order to estimate the effect of neuropsychological aspects on i-ADL Lawton & Brody Scale.
DRS-A: Dementia Rating Scale Attention; DRS-IP: Dementia Rating Scale Initiation/Perseveration; DRS-Const: Dementia Rating Scale Construction; DRS-C: Dementia Rating Scale Conceptualization; DRS-M: Dementia Rating Scale Memory; DRS-T: Dementia Rating Scale Total; ROCF: Rey–Osterrieth Complex Figure; TMT: Trail Making Test.
Discussion
The main goal of this study was to examine neurocognitive tests that predict dependence as assessed by the b-ADL and i-ADL. To estimate the relationship between neuropsychological aspects and the b-ADL scores, we developed three models. DRS-A (predictive model-1) was the only test that increased the probability of being dependent according to the b-ADL. An individual with an attention deficit is nearly 2.5 times more likely to be dependent according to the b-ADL than those with no attention deficit according to the DRS-A. This test includes repetition of a series of numbers, execution of instructions, counting, verbal recognition and visual correspondence. The DRS-A requires the use of perceptual functions, namely hearing and vision. It is known that these functions are affected by the aging process. Attention is fundamental for selecting the relevant auditory and visual information, and its decrement could lead to difficulties in performing basic daily tasks.
We developed four models to estimate the effect of neuropsychological variables on i-ADL. Regarding the DRS, DRS-M significantly increased, almost three-fold, the probability of being dependent according to the i-ADL. This test proposes tasks of evocation and verbal and visual recognition. According to our findings, evocation memory, being a task proceeded by distracting tasks, presents a high level of impairment, and was important to predict the ability to perform complex daily activities in individuals with MCI. ROCF reproduction significantly increased the probability of being dependent according to the i-ADL. An individual with a deficit in visuographic reproduction has a three-fold greater risk of being dependent according to the i-ADL compared to those who performed well in this test. This is a test that requires, in addition to the perceptive and integrative aspects of the figure, global and local reproduction strategies. Regarding the TMT, TMT-A significantly increased the probability of being dependent according to the i-ADL. An individual with lower scores on TMT-A had an approximately four times higher risk of being dependent according to the i-ADL compared to those who show adequate performance in this test, which measures attention, visual perception, visuo-motor speed, and processing speed. According to our results, the ability to switch between sequences in a complex process involved in executive functions, assessed by TMT-B, did not seem to show a relationship with the i-ADL score. These findings are in line with some studies that suggest that planning or problem solving abilities do not seem to show a relationship with the i-ADL score [22]. Others, however, demonstrated that subjects with higher executive dysfunction tend to have more limitations in ADLs [15].
According to the literature, short-term verbal memory has emerged as the most relevant cognitive domain predicting i-ADL score [8]. In the present study, we found that difficulties in visual-graphic Reproduction (ROCF Reproduction) and visual exploration/sequencing (TMT-A) are also associated with some variation in i-ADL score. Memory [14] and visuographic tasks [16] that incorporate different processes at once, are needed to perform daily tasks like shopping, food preparation, housekeeping, self-managing medication and handling finances. There are also some studies showing that visuospatial skills are relevant for functional independence [10]. One should highlight that TMT-A, ROCF Reproduction, DRS-M and DRS-A could be important in the diagnostic and prognostic determination of MCI and in the selection of prevention or intervention techniques in cognitive decline with age. We created a fourth statistical model, which considered the three previous significant factors, and concluded that the DRS-M was the only one that significantly increased the probability of being dependent according to the i-ADL. This model shows that an individual with memory impairment has a three times higher risk of being dependent according to the i-ADL compared to those who perform well in the DRS-M assessment. This is not particularly surprising considering that most of the participants with MCI (67.5%) had mild to moderate memory impairment. The fourth logistic model had high sensitivity, correctly classifying 94.2% of the subjects who were considered dependent according to the i-ADL. The discriminating capacity (Figure 1) was acceptable (AUC=0.739; p < 0.001).
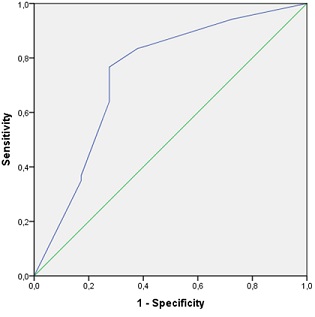 Figure 1: Area under the ROC curve, for Dementia Rating Scale Memory (DRS-M) as predictor of on instrumental Activities of Daily Living (i-ADL) Lawton & Brody Scale.
Figure 1: Area under the ROC curve, for Dementia Rating Scale Memory (DRS-M) as predictor of on instrumental Activities of Daily Living (i-ADL) Lawton & Brody Scale.
In the present study, the subdomains of i-ADL with the highest deficits were responsibility for own medication, shopping and preparing meals, which represent activities that require memory. The functional abilities that depend on memory are more impaired in patients with MCI. According to our findings, evocation memory, being preceded by distracting tasks, presents a high level of impairment and is important for predicting the performance of complex daily activities in individuals with MCI. Performance on tasks requiring free recall, following distractor trials, provided the best predictor of the ability to perform complex daily activities in individuals with MCI. These results are in line with other studies that refer to memory impairment as relevant for the diagnosis and determination of prognosis of MCI [23].
The strengths of this study include the large sample size and the administration of a neuropsychological screening with adequate predictive value. Nevertheless, the present study also included limitations, such as the absence of other groups of the population (e.g., with dementia, or without cognitive impairment) or the use of a scale of advanced ADL. The inclusion of these elements in future studies could strengthen the analysis of the predictive power of neuropsychological assessment on functional decline.
Conclusion
Memory and visuospatial tasks seem to contribute to the prediction of dependence according to the i-ADL. Attention deficits predict dependence according to the b-ADL. The i-ADL is more sensitive to the effects of cognitive decline. These results point to the need for interventions focused on attention, memory, and visuospatial decline to prevent decrements in the performance of tasks in everyday functioning.
Declaration of Competing Interest
None.
Funding Sources
None.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, [R H], upon reasonable request.
References
- Santos Henriques RPD, Tomas-Carus P, Filipe Marmeleira JF (2023) Association Between Neuropsychological Functions and Activities of Daily Living in People with Mild Cognitive Impairment. Exp Aging Res 49: 457-471.
- Reppermund S, Sachdev PS, Crawford J, Kochan NA, Slavin MJ, et al. (2011) The relationship of neuropsychological function to instrumental activities of daily living in mild cognitive impairment. Int J Geriatr Psychiatry 26: 843-852.
- Schmidt LI, Wahl HW (2019) Predictors of Performance in Everyday Technology Tasks in Older Adults with and Without Mild Cognitive Impairment. Gerontologist 59: 90-100.
- Jekel K, Damian M, Wattmo C, Hausner L, Bullock R, et al. (2015) Mild cognitive impairment and deficits in instrumental activities of daily living: A systematic review. Alzheimers Res Ther 7: 17.
- Farias ST, Mungas D, Reed BR, Harvey D, Cahn-Weiner D, et al. (2006) MCI is associated with deficits in everyday functioning. Alzheimer Dis Assoc Disord 20: 217-223.
- Katz MJ, Lipton RB, Hall CB, Zimmerman ME, Sanders AE, et al. (2012) Age-specific and sex-specific prevalence and incidence of mild cognitive impairment, dementia, and alzheimer dementia in blacks and whites: A report from the Einstein aging study. Alzheimer Dis Assoc Disord 26: 335-343.
- Sachdev PS, Lipnicki DM, Kochan NA, Crawford JD, Thalamuthu A, et al. (2015) The prevalence of mild cognitive impairment in diverse geographical and ethnocultural regions: The COSMIC Collaboration. PLoS One 10:
- Gainotti G, Quaranta D, Vita MG, Marra C (2014) Neuropsychological predictors of conversion from mild cognitive impairment to Alzheimer’s disease. J Alzheimers Dis 38: 481-495.
- Gazova I, Vlcek K, Laczó J, Nedelska Z, Hyncicova E, et al. (2012) Spatial navigation-A unique window into physiological and pathological aging. Front Aging Neurosci 4: 16.
- de Bruin, N., Bryant DC, MacLean JN, Gonzalez CLR (2016) Assessing visuospatial abilities in healthy aging: A novel visuomotor task. Front Aging Neurosci 8: 7.
- Salimi S, Irish M, Foxe D, Hodges JR, Piguet O, et al. (2018) Can visuospatial measures improve the diagnosis of Alzheimer’s disease? Alzheimers Dement (Amst) 10: 66-74.
- Tulliani N, Bissett M, Bye R, Chaudhary K, Fahey P, et al. (2019) The efficacy of cognitive interventions on the performance of instrumental activities of daily living in individuals with mild cognitive impairment or mild dementia: protocol for a systematic review and meta-analysis. Syst Rev 8: 222.
- Nadler JD, Richardson ED, Malloy PF, Marran ME, Hosteller Brinson ME (1993) The ability of the Dementia Rating Scale to predict everyday functioning. Arch Clin Neuropsychol 8: 449-460.
- Greenaway MC, Duncan NL, Hanna S, Smith GE (2012) Predicting functional ability in mild cognitive impairment with the Dementia Rating Scale-2. Int Psychogeriatr 24: 987-993.
- Cornelis E, Gorus E, Van Schelvergem N, De Vriendt P (2019) The relationship between basic, instrumental, and advanced activities of daily living and executive functioning in geriatric patients with neurocognitive disorders. Int J Geriatr Psychiatry 34: 889-899.
- Isella V, Traficante D, Tagliabue CF, Mapelli C, Ferri F, et al. (2013) A retrospective survey on rotated drawing in persons with mild cognitive impairment or degenerative dementia. Clin Neuropsychol 27: 1300-1315.
- Shelkey M, Wallace M (1999) Katz Index of Independence in Activities of Daily Living. Journal of Gerontological Nursing 25: 8-9.
- Lawton MP, Brody EM (1969) Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist 9: 179-186.
- Jurica P, Leitten C, Mattis S (2001) Dementia Rating Scale-2: Professional manual. Psychological Assessment Resources, California, USA.
- Kasai M, Meguro K, Hashimoto R, Ishizaki J, Yamadori A, et al. (2006) Non-verbal learning is impaired in very mild Alzheimer’s disease (CDR 0.5): Normative data from the learning version of the Rey-Osterrieth Complex Figure Test. Psychiatry Clin Neurosci 60: 139-146.
- Lezak MD, Howieson DB, Loring DW (2004) Neuropsychological Assessment (4thedn). O. U. Press, USA.
- Amanzio M, Palermo S, Zucca M, Rosato R, Rubino E, et al. (2018) Neuropsychological correlates of instrumental activities of daily living in neurocognitive disorders: A possible role for executive dysfunction and mood changes. Int Psychogeriatr 30: 1871-1881.
- Petersen RC (2016) Mild Cognitive Impairment. Continuum (Minneap Minn) 22: 404-418.
Citation: dos Santos Henriques RP, Tomas-Carus P, Marmeleira JFF (2023) Neuropsychological Assessment and Determination of Activities of Daily Living, the Role of Memory and Spatial Tasks in Mild Cognitive Impairment. J Gerontol Geriatr Med 9: 187.
Copyright: © 2023 Rogério Paulo dos Santos Henriques, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

