Journal of Medicine Study & Research Category: Medical
Type: Research Article
New Technique for Pelvic Floor Measurement - Transperineal Dynamic Ultrasound Measurement Method to Detection and Quantification of Rectocele, Cystocele, Enterocele and Perineal Descensus
*Corresponding Author(s):
Kowallik MJInstitution Of Magen Darm Zentrum Wiener Platz, Genovevastr 9, 51065 Köln, Germany
Tel:+49 22196444655,
Fax:+49 032122066201
Email:mkowallik@web.de
Received Date: Jun 24, 2018
Accepted Date: Jul 16, 2018
Published Date: Jul 30, 2018
Abstract
The pelvic floor is a complex area, exhibiting diverse pathologies. Among the so-called emptying disorders is the Obstructive Defecation Syndrome (ODS). The diagnosis of the pelvic floor presents us with major challenges, as the anatomy of the region is complicated and the physiology is often difficult to understand. Previous investigation methods have included MR-defecography, classic defecography, uro-gynecological examinations, proctological examinations, scores etc. Ultrasound examination of the pelvic floor is unlikely to be sufficiently established for some time. The examiner’s interpretation dependency and the lack of anatomical landmarks are challenging, which detracts from the significance of the investigation.
The aim of this descriptive measurement study is to develop and describe a unique and reliable method for the assessment and quantification of all pelvic floor changes from the group of obstructive defecation disorders. This method should be applied to all affected patients regardless of their age, size, weight, whether they suffer from minor diseases, and/or after surgery, and should deliver reliable and unique data. It should provide a diagnosis without any interpretation from the examiner.
Material and method: After anamnesis with detection of clear symptoms of obstructive defecation syndrome (incomplete evacuation, constipation, foreign body sensation etc.,) and clinical examination a consent to perform a pelvic floor sonography was obtained from all patients. To describe the measurement points we perform the examination for this study in primarily 25 women presenting obstructive defecation syndrome. In all examined patients, eight clearly defined measuring points were developed which can be found reliable at transperineal sonographic represented pelvic floor. These serve as a basis for the distance measurements in either a supine or a sitting position. The examinations were performed with an ultrasound scanner BK ProFocus ultra view, first supine and then in a sitting position. This resulted in selected measurement points and distances that were found in all the patients, and in both positions. Conversion of the absolute values as percentage changes allows for reliable diagnosis. Our study shows, in conclusion, that the new method of Transperineal Ultrasound Measurement on the Pelvic Floor (TUMPF) allows a reliable and unambiguous diagnosis in either the supine or the sitting position, whereby dependence on the ultrasound examiner can be avoided.
The aim of this descriptive measurement study is to develop and describe a unique and reliable method for the assessment and quantification of all pelvic floor changes from the group of obstructive defecation disorders. This method should be applied to all affected patients regardless of their age, size, weight, whether they suffer from minor diseases, and/or after surgery, and should deliver reliable and unique data. It should provide a diagnosis without any interpretation from the examiner.
Material and method: After anamnesis with detection of clear symptoms of obstructive defecation syndrome (incomplete evacuation, constipation, foreign body sensation etc.,) and clinical examination a consent to perform a pelvic floor sonography was obtained from all patients. To describe the measurement points we perform the examination for this study in primarily 25 women presenting obstructive defecation syndrome. In all examined patients, eight clearly defined measuring points were developed which can be found reliable at transperineal sonographic represented pelvic floor. These serve as a basis for the distance measurements in either a supine or a sitting position. The examinations were performed with an ultrasound scanner BK ProFocus ultra view, first supine and then in a sitting position. This resulted in selected measurement points and distances that were found in all the patients, and in both positions. Conversion of the absolute values as percentage changes allows for reliable diagnosis. Our study shows, in conclusion, that the new method of Transperineal Ultrasound Measurement on the Pelvic Floor (TUMPF) allows a reliable and unambiguous diagnosis in either the supine or the sitting position, whereby dependence on the ultrasound examiner can be avoided.
STATEMENT
The aim is to develop a unique and reliable sonographic method for the assessment and quantification of all pelvic floor changes from the group of obstructive defecation disorders. This method applied to all affected patients regardless of their age, size, weight etc., should deliver reliable and unique data.
INTRODUCTION
The pelvic floor is a complex area, exhibiting diverse pathologies [1,2]. Within the so-called emptying disorders can be found the obstructive defecation syndromes. The causes of this type of syndrome include the deterioration of the structures holding the pelvic organs physiologically in their positions [3,4]. Previous investigation methods include MR, classic defecography, uro-gynecological, proctological examinations, scores etc., [5-9].
The diagnosis of each faculty differs fundamentally from the others, and even within the same pathological area there are different ideas about diagnostic methods and treatments. The results are classified with the Pelvic Organ Prolapse Quantification (POP-Q), as well as classified into different levels [6,10]. This is a rational approach, but has the disadvantage that only the gynecological pathologies are considered. The front compartment (urologic) is occasionally considered, but the rear compartment (proctologic) is practically never considered. POP-Q considered only the excess of the descent of the uterus, the bladder is not directly, the descent of the rear compartment not sufficiently assessed [10]. Therapy proposals often do not involve combined pathological changes, which occur mostly on the pelvic floor [11]. The resulting therapy does not therefore address the complexity of the condition.
We realized, over time, that isolated changes in the pelvic floor rarely occur even when a global and standard examination was deemed necessary [12,13]. Accurate knowledge of all anatomical and physiological changes is essential for an optimal and personalized treatment strategy [11].
In many studies the examination position of the pelvic floor is seen as controversial. There are numerous works in which the supine or even the left lateral examination position is chosen. The guidelines for uro-gynecology justify the horizontal examination position, with its improved practicality for the examiner, although this is controversial. Some investigations reject the supine examination position, because it is not physiologically and gravity is disregarded, which in turn distorts the results [9,14-18].
This controversy could be eliminated by performing the examination in a unit that includes both positions. To obtain reliable examination results, first the supine position and then the sitting physiological position should be selected [17]. Both sets of results should be checked against not only what revealed the pathologies, but should also include the influence of gravity acting on the patient (and the pelvic floor) during the examination.
Pelvic floor examination using ultrasound has not until now been sufficiently established. Although a good correlation of ultrasound and proctologic measurements has been secured the lack of the ultrasound marker and examiner dependency are the most critical drawbacks [19,20]. The entire pelvic floor can be simply and reliably examined non-invasively by the transperineal pelvic floor 3D sonography assessment [19-24]. All three compartments are dynamically assessed at the same time, increasing the validity [17,25,26]. The study of a single compartment, however, seems to be insufficient for a firm diagnosis [27].
Due to the lack of standardized processes and sizes, the relevance of pelvic floor ultrasound treatment has not been sufficiently considered, although it is a direct method, simulating almost unchanged all the sequences of a defecation [28]. The necessity of a reproducible method delivering accurate, ubiquitous and comparable results at any time of the assessment is clear.
Despite the high level of availability and the increasing dissemination of transperineal sonography, relevant measuring points at the transperineal image of the pelvic floor are still missing (the pubis is the one bony structure that retains the position during movement, such as Valsalva) [29,30]. This however leaves too much scope for interpretation. It leaves the assessment examiner dependent and does not allow any clear quantification of the organ descend, even if it is very clearly visible. The previous measuring points at the transperineal representation were Bladder Symphysis Distance (BSD), anorectal angle, alpha, beta, gamma angle, hiatus size etc., [8,30-33].
These readings attempt to establish some order in the sonographic view of the pelvic floor. The classic angles and distances can change (such as the valsalva maneuver, squeeze, etc.), and they are measured. They have however no unique expressiveness and do not describe any quantification of the pathological change. The corresponding image must be interpreted freely.
The diagnosis of each faculty differs fundamentally from the others, and even within the same pathological area there are different ideas about diagnostic methods and treatments. The results are classified with the Pelvic Organ Prolapse Quantification (POP-Q), as well as classified into different levels [6,10]. This is a rational approach, but has the disadvantage that only the gynecological pathologies are considered. The front compartment (urologic) is occasionally considered, but the rear compartment (proctologic) is practically never considered. POP-Q considered only the excess of the descent of the uterus, the bladder is not directly, the descent of the rear compartment not sufficiently assessed [10]. Therapy proposals often do not involve combined pathological changes, which occur mostly on the pelvic floor [11]. The resulting therapy does not therefore address the complexity of the condition.
We realized, over time, that isolated changes in the pelvic floor rarely occur even when a global and standard examination was deemed necessary [12,13]. Accurate knowledge of all anatomical and physiological changes is essential for an optimal and personalized treatment strategy [11].
In many studies the examination position of the pelvic floor is seen as controversial. There are numerous works in which the supine or even the left lateral examination position is chosen. The guidelines for uro-gynecology justify the horizontal examination position, with its improved practicality for the examiner, although this is controversial. Some investigations reject the supine examination position, because it is not physiologically and gravity is disregarded, which in turn distorts the results [9,14-18].
This controversy could be eliminated by performing the examination in a unit that includes both positions. To obtain reliable examination results, first the supine position and then the sitting physiological position should be selected [17]. Both sets of results should be checked against not only what revealed the pathologies, but should also include the influence of gravity acting on the patient (and the pelvic floor) during the examination.
Pelvic floor examination using ultrasound has not until now been sufficiently established. Although a good correlation of ultrasound and proctologic measurements has been secured the lack of the ultrasound marker and examiner dependency are the most critical drawbacks [19,20]. The entire pelvic floor can be simply and reliably examined non-invasively by the transperineal pelvic floor 3D sonography assessment [19-24]. All three compartments are dynamically assessed at the same time, increasing the validity [17,25,26]. The study of a single compartment, however, seems to be insufficient for a firm diagnosis [27].
Due to the lack of standardized processes and sizes, the relevance of pelvic floor ultrasound treatment has not been sufficiently considered, although it is a direct method, simulating almost unchanged all the sequences of a defecation [28]. The necessity of a reproducible method delivering accurate, ubiquitous and comparable results at any time of the assessment is clear.
Despite the high level of availability and the increasing dissemination of transperineal sonography, relevant measuring points at the transperineal image of the pelvic floor are still missing (the pubis is the one bony structure that retains the position during movement, such as Valsalva) [29,30]. This however leaves too much scope for interpretation. It leaves the assessment examiner dependent and does not allow any clear quantification of the organ descend, even if it is very clearly visible. The previous measuring points at the transperineal representation were Bladder Symphysis Distance (BSD), anorectal angle, alpha, beta, gamma angle, hiatus size etc., [8,30-33].
These readings attempt to establish some order in the sonographic view of the pelvic floor. The classic angles and distances can change (such as the valsalva maneuver, squeeze, etc.), and they are measured. They have however no unique expressiveness and do not describe any quantification of the pathological change. The corresponding image must be interpreted freely.
MATERIAL AND METHOD
The observation of the change of the absolute values (bladder symphysis distance etc.) in reference to pubic symphysis is not sufficient for the evaluation of the expression of the pelvic organ descent. The relative changes in the organ position in relation to the normal state, which means the during valsalva provoked percentage change in the position to the baseline, seems much more important. The bench mark values are determined in the rest/supine position. In this way comparability for all issues is attained, regardless of the present pathology. The measuring method is lean on the existing Pelvic Organ Prolapse Quantification (POPQ) classification.
There are seven important factors for this measuring method:
• Reproducibility
• Can be applied to all patients (regardless of age, weight, height, pre-existing conditions, treatment etc.)
• Can be performed either pre- or post-procedure
• The values obtained are unique, fully reproducible, ubiquitous and comparable
• The determination of the value measured does not depend on the examiner (i.e., there is no room for misinterpretation)
• All three compartments can be simultaneously assessed; the isolated evaluation of several pathologies is blocked, and this which improves diagnostic safety
• Examination time is not significantly extended - the entire assessment requires approximately 15-20 minutes
There are seven important factors for this measuring method:
• Reproducibility
• Can be applied to all patients (regardless of age, weight, height, pre-existing conditions, treatment etc.)
• Can be performed either pre- or post-procedure
• The values obtained are unique, fully reproducible, ubiquitous and comparable
• The determination of the value measured does not depend on the examiner (i.e., there is no room for misinterpretation)
• All three compartments can be simultaneously assessed; the isolated evaluation of several pathologies is blocked, and this which improves diagnostic safety
• Examination time is not significantly extended - the entire assessment requires approximately 15-20 minutes
The measuring points of the pelvic floor (transperineal view)
The method of measurement is based on the determination of eight points (measured in both the supine and the sitting positions, including the Valsalva). The change of one position to another and the value of this change is documented. The percentage change in the location of these points (organs) then leads to the diagnosis.
The measuring points must be clearly definable, and should be easily tracked by any movement of the pelvic floor (valsalva or squeeze, etc.)
The following marks have been selected (Figure 1):
The method of measurement is based on the determination of eight points (measured in both the supine and the sitting positions, including the Valsalva). The change of one position to another and the value of this change is documented. The percentage change in the location of these points (organs) then leads to the diagnosis.
The measuring points must be clearly definable, and should be easily tracked by any movement of the pelvic floor (valsalva or squeeze, etc.)
The following marks have been selected (Figure 1):
1. Symphysis pubis
2. Interior of ostium urethrae
3. External ostium urethrae
4. Cervix
5. Posterior rectal wall - height of symphysis pubis
6. Anterior rectal wall - height of cervix
7. Anterior rectal wall - height of symphysis pubis
8. Anterior rectal wall - height of internal ostium urethrae
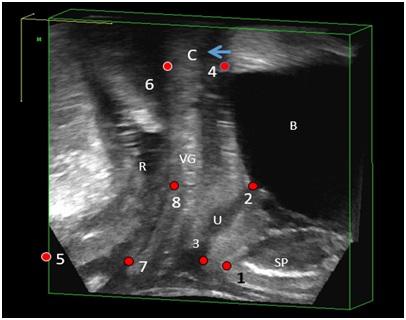
Figure 1: Clearly defined measuring points at the transperineal image of the pelvic floor.
1-Symphysis pubis; 2-Internal ostium urethrae; 3-External ostium urethrae; 4/C-cervix; 5-Posterior rectal wall - height symphysis pubis; 6-Anterior rectal wall - height cervix; 7-Anterior rectal wall - height symphysis pubis; 8-Anterior rectal wall - height internal ostium urethrae; B-Bladder; VG – Vagina; C-Cervix (height vesical roof, arrow), SP-Symphysis pubis; R-rectum
Measurement of individual distances
The following distances were measured at rest and then at the Valsalva, and received the following designations:
Front compartment (Figure 2):
1. The symphysis pubis - inside the Urethraostium (bladder symphyis distance) - 1
2. The inner ostium urethrae – the outer Ostium urethrae - 1a
3. The symphysis pubis - the bladder roof (regardless of the bladder filling) or (the cervix - if visible - is preferable) - 2
4. The bladder roof/cervix - the internal ostium urethrae - 2a
These measured values are used as a template for the other measurements and are transferred into the middle and posterior compartments (Table 1).
The following distances were measured at rest and then at the Valsalva, and received the following designations:
Front compartment (Figure 2):
1. The symphysis pubis - inside the Urethraostium (bladder symphyis distance) - 1
2. The inner ostium urethrae – the outer Ostium urethrae - 1a
3. The symphysis pubis - the bladder roof (regardless of the bladder filling) or (the cervix - if visible - is preferable) - 2
4. The bladder roof/cervix - the internal ostium urethrae - 2a
These measured values are used as a template for the other measurements and are transferred into the middle and posterior compartments (Table 1).
| Compartments | Measurement name | Proceed |
| Front compartment | ||
| 1 | Measurement | |
| 1a | Measurement | |
| 2 | Measurement | |
| 2a | Measurement | |
| Middle compartment | ||
| 3 | Adoption of value of 1 | |
| 3a | Measurement | |
| 4 | Adoption of value 2 | |
| 4a | Measurement | |
| Dorsal compartment | ||
| 5 | adoption value of 1 | |
| 5a | Measurement | |
| 6 | Adoption of value 2 | |
| 6a | Measurement | |
The values 1, 1a, 2, and 2a are determined. Output values are 1 and 2 and are the basis for the other measurements, which are then transferred to 3, 4, 5 and 6. This is based on a virtual value as a ‘template’ for measurement of the rest. The change is then measured in the Valsalva (sitting position).
Middle compartment (Figure 2):
5. The outer introitus vaginae (at symphysis pubis) - value 1 is adopted - 3
6. From there the distance to the outer introitus vaginae - 3a
7. The outer introitus median (at symphysis pubis) - value 2 is adopted - 4
8. From there the distance to the outer introitus measured - 4a
Dorsal compartment (Figure 2):
9. The posterior rectal wall (hight symphysis pubis) - value 1 is adopted - 5
10. The longest distance to the anterior rectal wall (the height above the external sphincter) measured - 5a
11. The posterior rectal wall (the height of the symphysis pubis) - the value of 2 is adopted - 6
12. The longest distance to the anterior rectal wall is measured from that point (the height above external the sphincter) - 6a
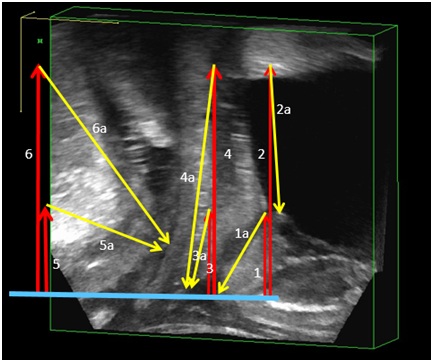
Figure 2: The distances shown in the pelvic floor measurement first in rest (supine position) then Valsalva (in sitting position).
Following distances are determined: 1-Symphysis pubis - inner urethra ostium (BSD); 1a-Inner urethra ostium - outer ostium urethrae; 2-Symphysis pubis - bladder roof (regardless of the bladder filling) or (height cervix - if it is visible - preferable); 2a-Bladder roof/cervix - internal ostium urethrae. The values 1 and 2 as a template for all further measurements will be taken in 3,4,5 and 6, while the values 3a, 4a, 5a, 6a must be measured in rest and Valsalva.
The measurements for the determination of Enterocele (Figure 3):
13. The anterior rectal wall - the height of the cervix (bladder roof) - d
14. The anterior rectal wall - the interior of the ostium urethrae - e
15. The anterior rectal wall - the height of the symphysis pubis - f
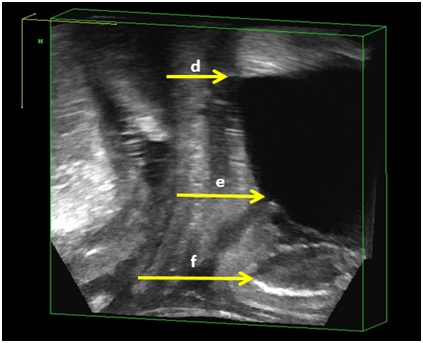
Figure 3: Detection of Enterocele - the defined distances d, e and f must be determined in rest (supine examination position) and during Valsalva (seated examination position).
This value d is the distance between - anterior rectal wall - height cervix (bladder roof). Distance e - between the anterior rectal wall - internal ostium urethrae, and distance f - between the anterior rectal wall and symphysis pubis. The enlargements of the distances to more than 50% show the presence of an Enterocele.
Middle compartment (Figure 2):
5. The outer introitus vaginae (at symphysis pubis) - value 1 is adopted - 3
6. From there the distance to the outer introitus vaginae - 3a
7. The outer introitus median (at symphysis pubis) - value 2 is adopted - 4
8. From there the distance to the outer introitus measured - 4a
Dorsal compartment (Figure 2):
9. The posterior rectal wall (hight symphysis pubis) - value 1 is adopted - 5
10. The longest distance to the anterior rectal wall (the height above the external sphincter) measured - 5a
11. The posterior rectal wall (the height of the symphysis pubis) - the value of 2 is adopted - 6
12. The longest distance to the anterior rectal wall is measured from that point (the height above external the sphincter) - 6a
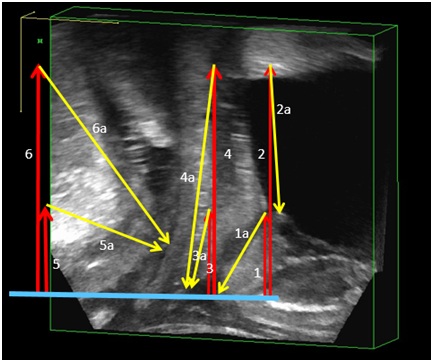
Figure 2: The distances shown in the pelvic floor measurement first in rest (supine position) then Valsalva (in sitting position).
Following distances are determined: 1-Symphysis pubis - inner urethra ostium (BSD); 1a-Inner urethra ostium - outer ostium urethrae; 2-Symphysis pubis - bladder roof (regardless of the bladder filling) or (height cervix - if it is visible - preferable); 2a-Bladder roof/cervix - internal ostium urethrae. The values 1 and 2 as a template for all further measurements will be taken in 3,4,5 and 6, while the values 3a, 4a, 5a, 6a must be measured in rest and Valsalva.
The measurements for the determination of Enterocele (Figure 3):
13. The anterior rectal wall - the height of the cervix (bladder roof) - d
14. The anterior rectal wall - the interior of the ostium urethrae - e
15. The anterior rectal wall - the height of the symphysis pubis - f
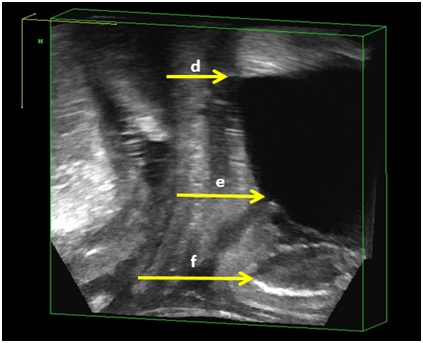
Figure 3: Detection of Enterocele - the defined distances d, e and f must be determined in rest (supine examination position) and during Valsalva (seated examination position).
This value d is the distance between - anterior rectal wall - height cervix (bladder roof). Distance e - between the anterior rectal wall - internal ostium urethrae, and distance f - between the anterior rectal wall and symphysis pubis. The enlargements of the distances to more than 50% show the presence of an Enterocele.
Evaluation
The values obtained in the supine position (without the Valsalva) are entered in a corresponding table. Afterwards the patient in the sitting position is prompted to execute the Valsalva maneuver, and the same points are measured and entered in the same table.
The values are then compared. The difference is first represented as an absolute number and also as a percentage variation. To increase the accuracy of the figures of the respective compartments (for example, 2 and 2a, or 4 and 4a), they are combined to form an arithmetic mean. This improves the accuracy and corrects any measurement outliers.
The values for the Enterocele in the tables are entered in the next step. Here, the differences in the percentage variation of the absolute numbers are also converted.
The values are then compared. The difference is first represented as an absolute number and also as a percentage variation. To increase the accuracy of the figures of the respective compartments (for example, 2 and 2a, or 4 and 4a), they are combined to form an arithmetic mean. This improves the accuracy and corrects any measurement outliers.
The values for the Enterocele in the tables are entered in the next step. Here, the differences in the percentage variation of the absolute numbers are also converted.
RESULTS
The investigation results show the percentage change in the position of clearly defined measuring points in all pelvic floor organs (bladder, uterus, rectum) due to the Valsalva in the sitting position (Figure 4). The evaluation is based on the previous pelvic organ prolapse classification.
This means in detail: A change in the position of, for example, the bladder (determined by a change in the position of the internal and external urethra, etc.). Less than 30% to the initial value means a bladder descensus of Iº.
A change in the position of the bladder by more than 30% but less than 60% of the initial value means a bladder descensus of IIº.
A change of more than 90% to the initial value means a bladder descensus of IIIº.
The approach in evaluation of the middle and the dorsal compartment is here the same (Figures 4 and 5).
This means in detail: A change in the position of, for example, the bladder (determined by a change in the position of the internal and external urethra, etc.). Less than 30% to the initial value means a bladder descensus of Iº.
A change in the position of the bladder by more than 30% but less than 60% of the initial value means a bladder descensus of IIº.
A change of more than 90% to the initial value means a bladder descensus of IIIº.
The approach in evaluation of the middle and the dorsal compartment is here the same (Figures 4 and 5).
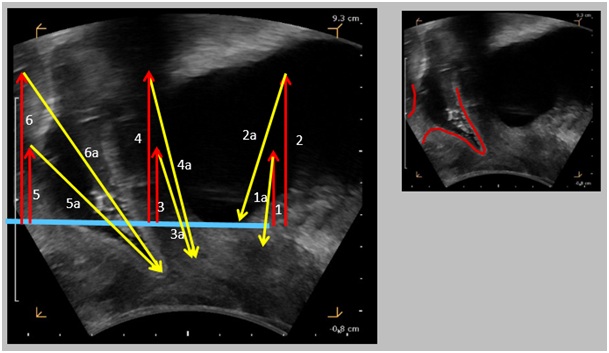
Figure 4: The change in the position of the organs in the Valsalva maneuver (examination sitting position) can be quantified by the renewed determination of the measured values.
The individual compartments are represented at the same time, so that both individual and combined pathologies are detected. Not the absolute values, but the percentage changes of the measured values are critical for the diagnosis. The evaluation is standardized through clearly defined limits (discrepancy less than 30% - grade I, grade II, 30-60% more than 90% discrepancy III).
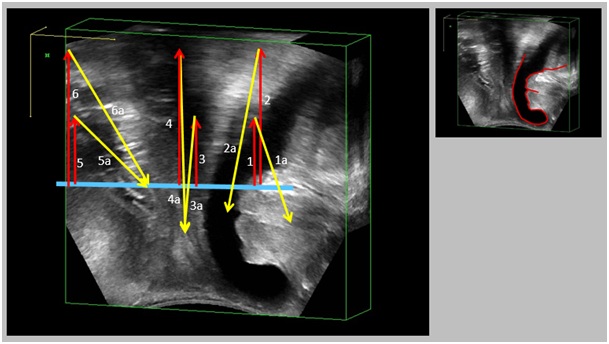
Figure 5: The position change of the organs during the Valsalva maneuver (sitting position) shows an isolated Zystocele IIIº, as well as descensus vaginae IIº.
The percentage increase in the measured values for the bladder is more than 90% grade IIIº, and for the middle compartment between 30% and 60% - level II. The rear compartment is not affected in this example.
Cystocele
For anterior compartment measurements it is important to measure the distance (1a, 2a) between the internal and external ostium of the urethra to determine the maximum bladder expansion (Figure 5).
Descensus vaginae
The determination of vaginal descenus (with measurements of 3a and 4a) should include the distal visible vaginal tissue. Here identification can be difficult, due to compression of the soft tissue by the transducer (Figures 4 and 5).
Rectocele
The measurement of the extension of the rectocele (5a, 6a) has the endpoint with regard to the rectum anterior wall just above the front edge of the Musculus Sphincter Ani Externus (MSAE). Here the farthest distance should be chosen. During the Valsalva this point is detached according to the shape of the rectocele (Figure 4).
Perineal descensus
The shape of the descensus perinei (levels I, II and III) can be calculated from the previous values.
Enterocele
The evaluation of the Enterocele shows a peculiarity. Changing all three output values determined by more than 50% secures an Enterocele IIIº. (The anterior rectal wall - the height of the cervix/bladder roof - value is d) if the change is more than 50% - an Enterocele Iº. A change of the two upper output values (the anterior rectal wall - the height of the cervix/bladder roof value is d and the anterior rectal wall - ostium urethrae - e) is more than 50% - an Enterocele IIº. An Enterocele is excluded in all other cases/configurations (Figure 3).
CONCLUSION
Offering a high level of acceptance and validity, ultrasound should be established as a standard testing method for assessing the pelvic floor [2,5,32,34,35]. It is a highly relevant screening examination for women with defecation irregularities and can be used both before and after surgery of the pelvic floor [36]. We use this tool to evaluate our procedures performed in our patients, what in the future may provide changes in the assessment of pelvic floor disorders [37]. This new measurement method for evaluation of the pelvic floor (TUMPF) can help to standardize sonographic diagnosis and to establish clearly defined parameters (until now a major deficiency) for the assessment and quantification of pathology on pelvic floor. Through this unique and comparable pathology quantification, the existing pelvic organ prolapse quantification classification can now be used in the field of ultrasound. This simple, fast and reliable examination method can be used to provide a clear picture of pathological changes and to provide quantification of the degree of each pathology both before and after therapy [18]. This could also improve communication between the various disciplines [34]. Through consistent and correct use of this method the correlation between clinical symptoms and pathology can be helpfully clarified, which in turn promises significant improvement in the therapy outcome [26]. This method is simple (examination time aproximately 20 minutes), easy to perform, standardized and allows to the surgeon to choose the right individual and comparable treatment option for all pelvic floor compartments in each patient, independently of any previous interpretation of the examiner. This in the long term could provide an improvement of the treatment effectiveness in all involved faculties and help to identify unique corresponding procedures for all emptying disorders.
REFERENCES
- Chamié LP, Ribeiro DMFR, Caiado AHM, Warmbrand G, Serafini PC (2018) Translabial US and Dynamic MR Imaging of the Pelvic Floor: Normal Anatomy and Dysfunction. Radiographics 38: 287-308.
- Murad-Regadas SM, Pinheiro Regadas FS, Rodrigues LV, da Silva Vilarinho A, Buchen G, et al. (2016) Correlation Between Echodefecography and 3-Dimensional Vaginal Ultrasonography in the Detection of Perineal Descent in Women With Constipation Symptoms. Dis Colon Rectum 59: 1191-1199.
- Kepenekci I, Keskinkilic B, Akinsu F, Cakir P, Elhan AH, et al. (2011) Prevalence of pelvic floor disorders in the female population and the impact of age, mode of delivery, and parity. Dis Colon Rectum 54: 85-94.
- Persu C, Chapple CR, Cauni V, Gutue S, Geavlete P (2011) Pelvic Organ Prolapse Quantification System (POP-Q) - a new era in pelvic prolapse staging. J Med Life 4: 75-81.
- Beer-Gabel M, Carter D (2015) Comparison of dynamic transperineal ultrasound and defecography for the evaluation of pelvic floor disorders. Int J Colorectal Dis 30: 835-841.
- Harvie HS, Lee DD, Andy UU, Shea JA, Arya LA (2018) Validity of utility measures for women with pelvic organ prolapsed. Am J Obstet Gynecol 218: 118-119.
- Lalwani N, Moshiri M, Lee JH, Bhargava P, Dighe MK (2013) Magnetic resonance imaging of pelvic floor dysfunction. Radiol Clin North Am 51: 1127-1139.
- Sultan AH, Monga A, Lee J, Emmanuel A, Norton C, et al. (2017) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female anorectal dysfunction. Int Urogynecol J 28: 5-31.
- Ribas Y, Hotouras A, Chan CL, Clavé P (2014) Imaging of pelvic floor disorders: are we underestimating gravity? Dis Colon Rectum 57: 1242-1244.
- Lermann JH , Renner SP, Winkler M, Müller A, Hildebrandt T, et al. (2010) Genitalvorfall: Symptomatik, Diagnostik und Therapie. Frauenheilkunde up2date 4: 111-133.
- Hausammann R, Steffen T, Weishaupt D, Beutner U, Hetzer FH (2009) Rectocele and intussusception: is there any coherence in symptoms or additional pelvic floor disorders? Tech Coloproctol 13: 17-25.
- Maglinte DD, Bartram CI, Hale DA, Park J, Kohli MD, et al. (2011) Functional imaging of the pelvic floor. Radiology 258: 23-39.
- Silva AC, Maglinte DD (2013) Pelvic floor disorders: what's the best test? Abdom Imaging 38: 1391-1408.
- Frawley HC, Galea MP, Phillips BA, Sherburn M, Bø K (2016) Effect of test position on pelvic floor muscle assessment. Int Urogynecol J Pelvic Floor Dysfunct 17: 365-371.
- Iacobellis F, Brillantino A, Renzi A, Monaco L, Serra N, et al. (2016) MR Imaging in Diagnosis of Pelvic Floor Descent: Supine versus Sitting Position. Gastroenterology Research and Practice 2016: 6594152.
- Lam TC, Islam N, Lubowski DZ, King DW (1993) Does squatting reduce pelvic floor descent during defaecation? Aust N Z J Surg 63: 172-174.
- Martellucci J, Brusciano L (2016) The Dynamic Transperineal Ultrasound Era of the Evaluation of Obstructed Defecation Syndrome. Dis Colon Rectum 59: 800-803.
- Vellucci F, Regini C, Barbanti C, Luisi S (2017) Pelvic floor evaluation with transperineal ultrasound: a new approach. Minerva Ginecol 70: 58-68.
- Beer-Gabel M, Teshler M, Barzilai N, Lurie Y, Malnick S, et al. (2002 ) Dynamic transperineal ultrasound in the diagnosis of pelvic floor disorders: pilot study. Dis Colon Rectum 45: 239-245.
- Murad-Regadas SM, Regadas Filho FS, Regadas FS, Rodrigues LV, de J R Pereira J, et al. (2014) Use of dynamic 3-dimensional transvaginal and transrectal ultrasonography to assess posterior pelvic floor dysfunction related to obstructed defecation. Dis Colon Rectum 57: 228-236.
- Lone F, Sultan AH, Stankiewicz A, Thakar R (2016) Interobserver agreement of multicompartment ultrasound in the assessment of pelvic floor anatomy. Br J Radiol 89: 20150704.
- Santoro GA, Wieczorek AP, Dietz HP, Mellgren A, Sultan AH, et al. (2011) State of the art: an integrated approach to pelvic floor ultrasonography. Ultrasound Obstet Gynecol 37: 381-396.
- Savoye-Collet C, Koning E, Dacher JN (2008) Radiologic evaluation of pelvic floor disorders. Gastroenterol Clin North Am 37: 553-567.
- Stone DE, Quiroz LH (2016) Ultrasound Imaging of the Pelvic Floor. Obstet Gynecol Clin North Am 43: 141-153.
- Palmerola R, Firoozi F, Baxter C (2017) Pelvic Floor Ultrasound. In: Fulgham P, Gilbert B (eds.). Practical Urological Ultrasound - Current Clinical Urology. Humana Press, New York, USA.
- Valsky DV, Yagel S (2007) Three-dimensional transperineal ultrasonography of the pelvic floor: improving visualization for new clinical applications and better functional assessment. J Ultrasound Med 26: 1373-1387.
- Law PA, Danin JC, Lamb GM, Regan L, Darzi A, et al. (2001) Dynamic imaging of the pelvic floor using an open-configuration magnetic resonance scanner. J Magn Reson Imaging 13: 923-929.
- Taylor SA (2009) Imaging pelvic floor dysfunction. Best Pract Res Clin Gastroenterol 23: 487-503.
- Salsi G, Cataneo I, Dodaro G, Rizzo N, Pilu G, et al. (2017) Three-dimensional/four-dimensional transperineal ultrasound: clinical utility and future prospects. Int J Womens Health 9: 643-656.
- Santoro GA, Wieczorek AP, Stankiewicz A, Wo?niak MM, Bogusiewicz M, et al. (2009) High-resolution three-dimensional endovaginal ultrasonography in the assessment of pelvic floor anatomy: a preliminary study. Int Urogynecol J Pelvic Floor Dysfunct 20: 1213-1222
- Tan L, Shek KL, Atan IK, Rojas RG, Dietz HP (2015) The repeatability of sonographic measures of functional pelvic floor anatomy. Int Urogynecol J 26: 1667-1672.
- Unger CA, Weinstein MM, Pretorius DH (2011) Pelvic floor imaging. Obstet Gynecol Clin North Am 38: 23-43.
- Xu CY, Ding SQ, Xue YH, Ding YJ (2013) Dynamic three-dimensional ultrasound in the diagnosis of pelvic floor dyssynergia. Zhonghua Wei Chang Wai Ke Za Zhi 16: 429-433.
- Dietz HP (2011) Female pelvic floor dysfunction-an imaging perspective. Nat Rev Gastroenterol Hepatol 9: 113-121.
- van Gruting IMA, Stankiewicz A, Kluivers K, De Bin R, Blake H, et al. (2017) Accuracy of Four Imaging Techniques for Diagnosis of Posterior Pelvic Floor Disorders. Obstet Gynecol 130: 1017-1024.
- Hainsworth AJ, Solanki D, Hamad A, Morris SJ, Schizas AM, et al. (2017) Integrated total pelvic floor ultrasound in pelvic floor defaecatory dysfunction. Colorectal Dis 19: O54-O65.
- Vitton V, Vignally P, Barthet M, Cohen V, Durieux O, et al. (2011) Dynamic anal endosonography and MRI defecography in diagnosis of pelvic floor disorders: comparison with conventional defecography. Dis Colon Rectum 54: 1398-1404.
Citation: Kowallik MJ, Prohm P, Kuruc T, Pi?at J, Lo Nigro MC, et al. (2018) New Technique for Pelvic Floor Measurement - Transperineal Dynamic Ultrasound Measurement Method to Detection and Quantification of Rectocele, Cystocele, Enterocele and Perineal Descensus. J Med Stud Res 1: 003.
Copyright: © 2018 Kowallik MJ, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
© 2026, Copyrights Herald Scholarly Open Access. All Rights Reserved!