
Occipito-Cervical Fixation Surgical Experience
*Corresponding Author(s):
Ramadan ShamseldeinDepartment Of Neurosurgery, Shebin Elkom Teaching Hospital, Al Minufiyah, Egypt
Tel:+20 1001251003,
Email:ramadangalal77@gmail.com
Abstract
Occipito-cervical lesions not uncommonbut usually fatal conditions. Pain, limitation of movements, and weakness, were the main complaints of patients with upper cervical lesions. Internal fixation and fusion almost is a successful way for treatment by different means. CT scan is the imaging modality of choice for evaluation.
Aim
To present our surgical experience in occipito-cervical fixation using both lateral mass screws and subaxial cervical pedicle screws in different cases.
Patients and Methods
We operated 14 patients, 11 with traumatic and 3 with pathologically diagnosed occipitocervical instability. From December 2016 to June 2019. Patients presented with neck pain, limitation of neck movement, and neurological deficits. The patients investigated by standard plain X ray cervical spine, CT scan and MRI cervical spine pre-operatively, and they operated thorough posterior occipito-cervical fixation rod system utilizing lateral mass screws in majority of cases and pedicle screws in some others.
Results
The mean age of the studied cases was 39.7 years; trauma was the cause of instability in 11 patients, one with rheumatoid arthritis and two with neoplastic lesions. The mean follow up period 15 months. We used screw rod system in posterior cranio-cervical fixation with iliac bone graft and or bone substitutes utilizing lateral mass screws in majority of cases and subaxial pedicle screws in some cases without operative or post-operative complications. All our patients were improved neurologically post-operatively and no hard were failure during the follow up period.
Conclusion
Craniocervical instability rare and, may be fatal condition. Posterior occipito-cervical fixation when indicated can be done by various techniques. The screw rod system was the most upgraded used technique with immediate rigid fixation. Subaxial cervical pedicle screw can be utilized in certain situations with caution after thorough understanding of patient CT. Surgery in this area was possible with confident results.
Keywords
INTRODUCTION
There are different means to mark the instability at the level of occipitoatlantal or atlantoaxial joints. Plain radiography is usually the first-line imaging modality. Findings related to occipitoatlantal translation, lateral atlas displacement, or atlantoaxial translation can raise suspicions of instability [5]. Computed Tomography (CT) improves definition of these articulations and can also detect rotational subluxation. Magnetic Resonance Imaging (MRI) can help determine ligamentous injury, especially of the transverse atlantal ligament [6].
The first preliminary report on successful use of a screw rod stabilizing system posteriorly applied to the occipito-cervical junction was in 1996 by Jeanneret et al., [7].
In many studies, the clinical utility, safety, and effectiveness of hook-and-screw-rod and screw-and-rod instrumentation for posterior craniocervical fixation were evaluated. There is no superior definite method for occipito-cervical fusion in case of an unstable Cranio Cervical Junction (CCJ) almost all are controversial since the immediate desired rigid stabilization increasing surgical complexity and risk [8]. Sub axial cervical pedicle screw fixation is analternate techniqueto lateral mass screw fixation. Although it's biomechanically superior to lateral mass screw, but data about best entry point, trajectory and safety are limited, so it's not used routinely from C3-C6.The indication of pedicle screw fixationis limited to certain conditions where rigid internal fixation cannot be achieved with conventional techniques [9].
Pre-operative planning is essential and familiarity with different surgical techniques and implants allows the surgeon to choose the correct fixation method, giving the patients the best chance to heal [10].
PATIENTS AND METHODS
Operative steps
Follow up
Results
|
Frankel grade No. of cases |
Preop. |
Postop. |
|
A=complete paralysis |
- |
- |
|
B= sensory function only below the injury level |
- |
- |
|
C=incomplete motor function below injury level |
7 |
- |
|
D=fair to good motor function below injury level |
6 |
- |
|
E= normal function |
1 |
12 |
|
14 |
No of cases |
|
39.7 |
mean |
|
67 |
maximum |
|
16 |
minimum |
|
15.12 |
St. deviation |
|
Male |
Female |
|
11 |
3 |
|
78.60% |
21.40% |
|
Type of lesion |
No |
|
traumatic |
11 |
|
Rheumatoid |
1 |
|
neoplastic |
2 |
|
infectious |
non |
|
Mood of trauma |
No |
|
Road traffic accidents |
4 |
|
Falling from height |
4 |
|
Diving injury |
2 |
|
Firearm injury |
1 |
In two cases with neoplastic lesion C2 bypassed and instead C3 and C4 pedicle screws inserted to get more firm stabilization with the occiput.
As regard to the radiological finding of these cases: Two patients had destructive neoplastic lesion in C2 body. One of them left pedicle involved with evident cord compression, proved post-operatively plasmacytoma, while the other the right pedicle involved and proved postoperative histopathological diagnosis lung metastasis. One patient diagnosed pre-operatively as rheumatoid arthritis presented by well-formed pannus and ventral cord compression. The remaining 11 traumatic patients radiologically diagnosed as 7 cases with Type II odontoid fracture and 3 cases burst fracture C1 and one case fire arm injury with complex fracture of C1 with C2. These patients operated through posterior occipito-cervical fixation using screws-rod systems. Post-operatively all cases were followed for stability of the hard ware fixation system and efficacy of bone fusion in regular visit. There was no hard ware failure of the used screws rood system with accepted bony fusion in 10 traumatic cases, poor fusion in rheumatoid arthritis case and no observed fusion in the neoplastic case during the short period of follow up. There were no intra-operative or post-operative complications, no significant operative blood loss (Case 1 and 2).
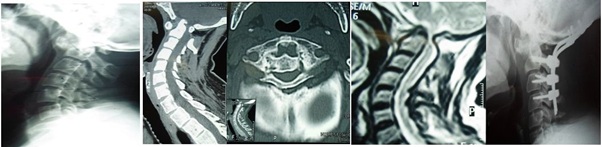 Case 1: Male patient 43ys falling injury. plain X-ray of cervical spine lateral view with anterior and upward displacement of the dens, sagittal reconstruction CT scan with evident upward migration and posterior displacement of the dens, axial CT scan cut opposite C1 with narrowed anteroposterior diameter, MRI sagital view with marked upper cervical spinal cord compression and post operative plain X-ray of OC fixation BY screw rod system included the occiput and C2 C3 and C4 with laminectomy C1 and foramen magnum decompression.
Case 1: Male patient 43ys falling injury. plain X-ray of cervical spine lateral view with anterior and upward displacement of the dens, sagittal reconstruction CT scan with evident upward migration and posterior displacement of the dens, axial CT scan cut opposite C1 with narrowed anteroposterior diameter, MRI sagital view with marked upper cervical spinal cord compression and post operative plain X-ray of OC fixation BY screw rod system included the occiput and C2 C3 and C4 with laminectomy C1 and foramen magnum decompression.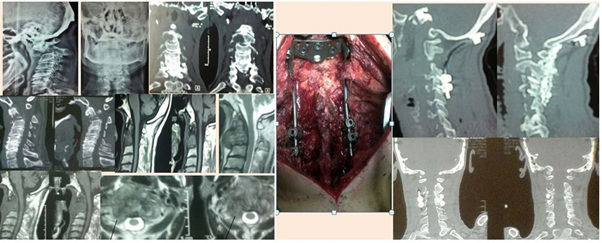 Case 2: Male patient 64years old presented with neck pain, dysphagia and Right upper limb monoparesis. Plain radiography show C2 disturbed anatomy and instability, CT show detailed bony lesion destruction of C2 and MRI show anterior retropharyngeal and right posterior neural encroachment. Operated posterior craniocervical fixation and right transpedicular intralesional decompression. The pathology was large cell lung carcinoma metastasis.
Case 2: Male patient 64years old presented with neck pain, dysphagia and Right upper limb monoparesis. Plain radiography show C2 disturbed anatomy and instability, CT show detailed bony lesion destruction of C2 and MRI show anterior retropharyngeal and right posterior neural encroachment. Operated posterior craniocervical fixation and right transpedicular intralesional decompression. The pathology was large cell lung carcinoma metastasis.DISCUSSION
Although pedicle screws biomechanically superior to lateral mass screw, data about best entry point, trajectory and safety are limited, so it's not used routinely from C3-C6, and its indication is limited to certain conditions where rigid internal fixation cannot be achieved with conventional techniques [9]. So in this series cervical pedicle screws were utilized at C3 and C4 levels in tow patients, suffering neoplastic lesion at C2, to get more firm stabilization with the occiput.
As regard to our patient’s number (14) was small like other series [4,11,14,15] and males were dominant in all series. The main age (39.7 years) of our patients was younger than in other series. The clinical presentation of our patients was of no difference of other series due to rarity of the cases. We used Frankle grading scale in clinical evaluation in agree with others as Ihab et al., 2011, but another authers use Nurick scale [14] or Japanias orthopedic association score [4]. The indications for posterior occipito-cervical fixation were the same with all authors with different concepts about the used construct, with priority to the screw rod systems for fixation. In our series there were no intra-operative, post-operative complications nor surgery related deaths. This agreed of George et al 2011 series, and with both series of Yu et al., 2009, and Vinu et al., 2016, except for single case post-operative infection in each series. Hirch et al., 2014, also recorded one case of failed fusion related to post-operative infection. Byung et al 2010, reported one case of vertebral artery injury during the operation, and Ihab et al., 2011, reported 3 cases with post-operative transient neurological deterioration, two cases had superficial wound infection and CSF leak occurred in one case. Byung et al., 2010 also reported one patient died 2 months after surgery because pneumonia and sepsis. Bony fusion along short time of follow up (about fourteen months) was achieved in 10 patients who were similar or nearly equal to other series.
CONCLUSION
CONFLICT OF INTEREST STATEMENT
REFERENCES
- Gopal VV (2016) Atlantoaxial fixation-Anterior or posterior approach, critical review. The Journal of Spinal surgery 3: 51-54.
- Saxena A (2017) Cranio-Cervical Trauma Eidemiology, Classification, Diagnosis and Management. J Spine Neurosurgery 6: 5.
- Powers B, Miller MD, Kramer RS, Martinez S, Gehweiler JA Jr (1979) Traumatic anterior atlanto-occipital dislocation. Neurosurgery 4: 12-17.
- Kim BS, Yoo DS, Phil WH, Huh PW Cho KS, et al. (2010) Atlantoaxial Transpedicular Screw Fixation for the Management of Traumatic Upper Cervical Spine Instability. J Korean Neurotraumatol Soc 6: 143-149.
- Greene KA, Dickman CA, Marciano FF, Drabier JB, Hadley MN, et al. (1997) Acute axis fractures. Analysis of management and outcome in 340 consecutive cases. Spine 22: 1843-1852.
- Dickman CA, Greene KA, Sonntag VK (1996) Injuries involving the transverse atlantal ligament: classification and treatment guidelines based upon experience with 39 injuries. Neurosurgery 38: 44-50.
- Jeanneret B (1996) Posterior rod system of the cervical spine: A new implant allowing optimal screw insertion. Eur Spine J 5: 350-356.
- Menezes AH (1991) Complications of surgery at the craniovertebral junction--avoidance and management. Pediatr Neurosurg 17: 254-266.
- Rongming Xu, Ebraheim NA, Skie M (2008) Pedicle screw fixation in the lower cervical spine: Case series. The American Journal of Orthopedics 403-408.
- Allen RT, Decker R, Hong JT, Sasso R (2015) Complications of occipito cervical fixation. Seminars in Spine Surgery 21: 167-176.
- Kuroki H (2014) Management of Atlantoaxial Instability - Surgical Strategy Based on Biomechanical Viewpoints. J Neurosurgery and spine 2: 1-5.
- Ihab Z, Wael F (2011) Occipito cervical fixation in the management of craniocervical instabilities. Alexandria Journal of Medicine 47: 185-192.
- Currier BL, Papagelopoulos PJ, Neale PG, Andreshak JL, Hokari Y,et al. (2003) Biomechanical evaluation of new posterior occipitocervical instrumentation system. Clin Orthop Relat Res 411: 103-115.
- Hsu YH, Liang ML, Yen YS, Cheng H, Huang CI, et al. (2009) Use of Screw-Rod System in Occipitocervical Fixation. J Chin Med Assoc 72: 20-28.
- Sapkas G, Papadakis SA, Segkos D, Kateros K, Tsakotos G, et al. (2011) Posterior instrumentation for occipitocervical fusion. Open Orthop J 5: 209-218.
Citation: Shamseldien R, Hendam H (2019) Occipito-Cervical Fixation Surgical Experience. J Surg Curr Trend Innov 3: 022.
Copyright: © 2019 Ramadan Shamseldein, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

