
Optimising Distal Femoral Fractures in Older Adults: An MDT and Orthogeriatric Model
*Corresponding Author(s):
Christian ChessRoyal United Hospital, Bath, United Kingdom
Tel:+44 07733185574,
Email:c.chess@nhs.net
Abstract
Background: Fragility Distal Femoral Fractures (DFFs) in older adults are associated with high morbidity (64%) and one-year mortality (26-35%), outcomes comparable to hip fractures. Historically, they have lacked the structured orthogeriatric pathways, national audit, and financial incentives that have transformed hip-fracture care.
Aim: To present an evidence-based, multidisciplinary pathway for DFF management aligned with the 2021/22 extension of the Best Practice Tariff (BPT) and National Hip Fracture Database (NHFD) to distal femoral fractures.
Pathway summary: From admission, early orthogeriatric co-management and comprehensive geriatric assessment (within 72 hours) drive pre-operative optimisation: patient blood management with tranexamic acid, anaemia correction, multicomponent delirium-prevention bundle, and surgery within 48 hours by a frailty-experienced team. Implant selection (retrograde nailing, locking plates, nail-plate hybrids, or distal femoral replacement) prioritises constructs enabling immediate weight-bearing as tolerated. Postoperative care mandates day-one mobilisation, daily orthogeriatric review, prompt anti-osteoporotic therapy initiation and Fracture Liaison Service referral. Discharge includes a falls-prevention and sarcopenia-management plan with community rehabilitation linkage.
Conclusion: This integrated, audited pathway - mirroring proven hip-fracture standards - targets the key modifiable drivers of adverse outcomes. Widespread adoption will reduce variation, lower mortality and institutionalisation rates, while delivering equitable, high-quality care for one of trauma surgery’s most vulnerable patient groups.
Keywords
Aged; Blood Transfusion/Methods; Delirium/Prevention & Control; Distal; Femoral Fractures; Osteoporosis/Drug Therapy; Weight-Bearing
Introduction
Distal Femoral Fractures (DFFs) are an often overlooked and under-appreciated source of morbidity and mortality in elderly patients. They present a high level of surgical complexity, with multiple treatment options available (nailing, plating, arthroplasty and combination), compounded by challenging perioperative optimisation and frequently inadequate system-level support.
The typical DFF patient is elderly, frail and multimorbid, presenting with osteoporosis, sarcopenia and managing significant polypharmacy alongside pre-existing functional dependency [1]. This profound vulnerability is starkly reflected in clinical outcomes: Loosen et al., [2] reported 64% perioperative morbidity and a 26-35% one-year mortality (median age 86.5) following treatment for DFFs, with 62% of previously independent, home-dwelling patients failing to return home and requiring long-term residential care. Clinically and demographically, DFFs mirror hip fractures, yet historically have lacked the same structured care pathways with orthogeriatric input, national audit, and aligned financial incentives, resulting in preventable disparities in outcomes [3,4]. Encouragingly, this landscape is changing. NHS England has extended the Best Practice Tariff (BPT) to distal femoral fractures, and the National Hip Fracture Database (NHFD) has begun explicit case capture of DFFs [5]. This article presents a Formalised Multidisciplinary Team (MDT) pathway for the assessment and management of fragility distal femoral fractures. By standardising care across pre-operative, intraoperative, and postoperative phases, the approach closes performance gaps, integrates medical and surgical optimisation, and delivers measurable improvements in clinical outcomes.
Pre Operative Optimisation
Pre-operative optimisation for distal femoral fractures should begin at admission and focus on high-impact interventions to reduce mortality and major complications. Orthogeriatric Co-Management (OGCM) paired with Comprehensive Geriatric Assessments (GCAs) provides the greatest leverage in elderly DFF management. Combining several key care elements including anaemia optimisation, nutrition plans, medication rationalisation and guide-based VTE prophylaxis, not only drastically lowers patient mortality [6,7], but reduces patient length of stay and improves discharge outcomes [8-10]. Additionally, OGCM input accelerates patient readiness for theatre, ensuring the < 48 hour time line is adhered to [11].
A structures Patient Blood Management (PBM) bundle that includes routine Tranexamic Acid (TXA), restrictive transfusion thresholds (Hb ≈70-80 g/L for orthopaedics/CVD), single-unit transfusions with reassessment, early iron therapy, and haemostasis checklists, helps reduce blood loss and transfusion requirements without increasing thromboembolic risk [6,12,13].
Thirdly, an early focus on delirium prevention through multi-component prevention bundles helps reduce delirium rates and associated downstream complications [14,15]. These bundles should concentrate on patient orientation, sensory aids, sleep hygiene measures, opioid-sparing analgesia and adequate hydration.
Finally, timely surgery-facilitated by this rapid optimisation and prioritised theatre access within 24-48 hours-is strongly associated with reduced mortality and shorter length of stay [9,16]. In hip fracture care, aggressive adherence to this target has been a key driver of improved outcomes since the NHFD’s inception. This sequence - OGCM/GCA > PMB Bundle > Delirium Bundle > Surgery within 24-48 hours - has revolutionised hip fracture management, and should be extended to the care of distal femoral fractures.
Intra-Operative
Optimising fixation choice in frail older adults with Distal Femoral Fractures (DFF)
The overarching aim in the surgical fixation of geriatric DFFs is to achieve a stable construct that permits early weight bearing. Early mobilisation correlates to better survival, complications and discharge destination. Construct selection should therefore be individualised to fracture pattern (AO/OTA), bone stock, pre-injury function and surgeon expertise. Locking plates remain a versatile option for intra-articular, metaphyseal comminution and periprosthetic patterns, and can be delivered through minimally invasive techniques (Figure 1). Reported union rates are high, though failures cluster with suboptimal bridge-plating technique and certain implant orientations can irritate soft tissues [17]. Locking technology is particularly useful in poor bone quality as it bypasses the weak bone-plate contact and reduces vascular disruption and so use in geriatric populations is numerous.
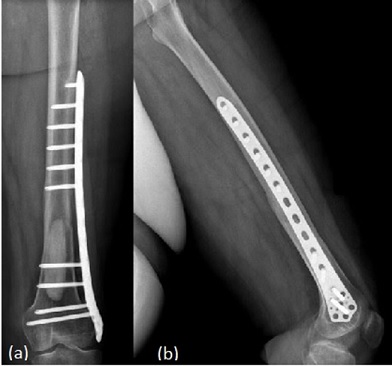 Figure 1: Radiograph of a left distal femoral plate fixation. (a) - Anterior View. (b) - Lateral View [18].
Figure 1: Radiograph of a left distal femoral plate fixation. (a) - Anterior View. (b) - Lateral View [18].
Retrograde Intramedullary (IM) nails are best suited to extra-articular supracondylar DFFs, particularly transverse or short oblique patterns (Figure 2). IM nails allow percutaneous insertion, reducing soft-tissue disruption, and load-sharing biomechanics favour faster rehabilitation. However, knee pain is a recognised complication and requires active physiotherapy to prevent it from developing. Contemporary data from comparative studies show that IM nails achieve outcomes equal to or superior to plating in many DFFs, particularly in frail patients with intact articular surfaces. This evidence supports the growing preference for IM nailing in these high-risk cohorts.
Across elderly DFFs, neither plating nor nailing is deemed universally superior. The choice should be guided by the degree of articular involvement, bone stock quality, existing arthroplasties and the priority of enabling early weight bearing. For extra-articular fractures with favourable canal geometry, intramedullary nailing is a preferred approach due to its percutaneous insertion and load-sharing properties. In contrast, locking plates predominate when the articular surface is involved and buttress support is required. Ultimately, the shared objective is an implant strategy that facilitates immediate or early full weight bearing within a structured MDT pathway.
 Figure 2: Radiograph of a left retrograde intramedullary nail fixation, lateral view [19].
Figure 2: Radiograph of a left retrograde intramedullary nail fixation, lateral view [19].
A third option is dual fixation through a nail-plate construct (Figure 3). This is gaining traction for complex AO-33C fractures, severe osteopenia, prior plate non-union, bicondylar/transcondylar patterns and select periprosthetic cases. By combining a retrograde IM nail with lateral plating or dual plating, these hybrid constructs enhance rotational axial stability, reduce non-union risk, and permit earlier, safer weight bearing. Contemporary reviews and case series detail evolving indications and surgical techniques.
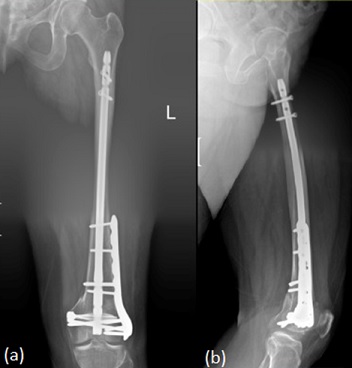 Figure 3: Radiograph of a left combined femoral intramedullary nail and plate fixation. (a) Anterior view. (b) Lateral View [20].
Figure 3: Radiograph of a left combined femoral intramedullary nail and plate fixation. (a) Anterior view. (b) Lateral View [20].
Distal Femoral Replacement (DFR) replaces the irreparably damaged distal femur with a prosthesis and is best reserved for fractures that cannot be reliably reconstructed (Figure 4). They are of particular use in those with severe comminution or in select periprosthetic injuries, especially in low-demand frail patients. Its key advantage lies in enabling immediate or early full weight bearing in these complex, unstable fracture patterns, thus avoiding prolonged restrictive mobilisation. However, DFR is a more extensive and costly operation with higher early complication rates and potential long term implant issues. When stable fixation remains feasible, it is generally preferred. Decisions should involve MDT discussion in experienced centres, with shared decision-making to align risks, benefits and patient goals.
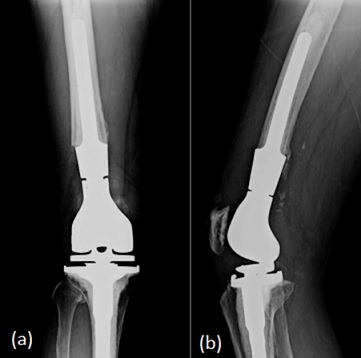 Figure 4: Radiograph of a right distal femoral replacement. (a) Anterior View. (b) Lateral View [21].
Figure 4: Radiograph of a right distal femoral replacement. (a) Anterior View. (b) Lateral View [21].
In frail elderly patients, there is no single operative technique that is universally superior. Instead, the implant strategy should match fracture biomechanics to the priority of early loading. Intramedullary nailing suits extra-articular patterns: locking plates address intra-articular or periprosthetic challenges requiring precise reduction, nail-plate hybrid constructs are valuable for complex C-type fractures or extreme osteopenia, and DFR is reserved for truly non-reconstructible injuries.
Post Surgery
Integrated orthogeriatric co-management and delirium prevention
As mentioned previously, Orthogeriatric co-management is the cornerstone of high-quality fragility fracture care. Integrating geriatric expertise from admission to systematically address the profound vulnerability of DFF patients. Daily multidisciplinary rounds - led by orthopaedic surgeons, geriatricians, physiotherapists, and occupational therapists - establish shared goals for patients and the MDT. In parallel, there should be an emphasis on optimising comorbidities, deprescribing high-risk medications, screening for delirium and dementia, and initiating fall prevention strategies [22].
This is echoed by the BOAST ‘Care of older/frail orthopaedic trauma patient’ guidance that advises all patients should undergo a comprehensive geriatric assessment, including falls, nutritional assessment and bone health reviews [23]. This model has consistently improved outcomes in hip fracture cohorts, reducing in-hospital mortality, one-year mortality, and post operation complications, while also enhancing medical optimisation and osteoporosis management [1,24,25].
Postoperative delirium is one of the commonest complications following hip fracture surgery, with reported incidences in high-risk cohorts approaching 70%. It is associated with longer hospital stays, poorer functional and cognitive recovery. Importantly, it results in substantially higher short- and long-term mortality, adding roughly 2–3 inpatient days and contributing to 30-day mortality rates of 7-10% [11,26]. Multicomponent non-pharmacological bundles reduce delirium, with odds ratios around 0.57 for multicomponent interventions and 0.71 for broader programmes, corresponding to roughly 30-40% lower odds of delirium. Opioid-sparing regional techniques such as fascia iliaca blocks significantly lower postoperative delirium risk in hip-surgery RCTs. Thus supporting their inclusion as core elements of OGCM delirium-prevention pathways [15,27,28].
The bundle is embedded in a pathway checklist, paired with routine risk stratification and daily 4AT screening to trigger targeted actions [29]. Adherence is monitored as a process measure (target >80%) and correlated with delirium incidence, length of stay, and discharge destination. Although DFF-specific trials are limited, the overlapping pathophysiology with hip fracture cohorts renders this orthogeriatric-aligned approach both evidence-based and essential [3]. Real-world implementation demonstrates the impact of embedding orthogeriatric co-management. The Southland (New Zealand) model combines daily orthopaedic rounds with twice-weekly geriatric review addressing falls risk, osteoporosis, polypharmacy, and nutrition, reduced complications by 12%, shortened time to discharge by 6.5 days, and delivered significant cost savings [22]. Similarly, Lisk et al., [30] reported a co-managed pathway yielding approximately £2.7 million in annual savings per 1,000 patients through reduced length of stay.
By ensuring early optimisation and proactive prevention, OGCM narrows the outcome gap in DFF care, enhancing safety, efficiency, timely discharge, functional recovery, and alleviating systemic financial pressures.
Postoperative Mobilisation and Rehabilitation
Postoperative rehabilitation is pivotal to recovery after distal femoral fracture surgery in frail older adults. Regardless of surgical technique, the primary objective is to enable full weight-bearing as early as safely feasible. Early mobilisation, ideally from day one, mitigates the risks associated with post op immobility, such as poor recovery, deep vein thrombosis and pulmonary embolisms. Furthermore, it is a core Enhanced Recovery After Surgery (ERAS) principle that reduces complications, shortens hospital stay, and accelerates recovery of walking capacity [31].
Most recent evidence supports Weight-Bearing As Tolerated (WBAT) when reduction is anatomic and fixation secure. A 2025 meta-analysis of DFF management found no increased revision or complication risk with early loading versus restriction, though heterogeneity and predominantly Level II-III evidence warrant cautious interpretation [32]. However, current practice remains variable: immediate WBAT is routine after retrograde nails or nail-plate constructs but less common after isolated lateral locking plates [33], despite consecutive studies of periprosthetic DFFs fixed using lateral locking plates confirming safe immediate and unrestricted WBAT when reduction and construct integrity were robust.
To reduce variation, the operation note must include an explicit weight-bearing instruction (e.g., unrestricted or time-limited protected weight bearing), linked to construct choice, reduction quality and with defined escalation triggers (pain, alignment loss, radiographic concern) per BOAST guidance. Rehabilitation commences immediately to prevent complications such as pressure injuries, venous thromboembolism, pneumonia, joint stiffness, and irreversible functional decline. Goals are defined at the outset and individualised to the patient, encompassing out-of-bed sitting, standing, safe transfers, progressive weight-bearing, and restoration of baseline function where achievable. Interventions integrate muscle strengthening, range-of-motion exercises and task-specific mobility training [34]. Progress is tracked against daily, patient-specific milestones with active input from the wider MDT. The Best Practice Tariff (BPT) criterion for neck-of-femur fractures - physiotherapy assessment within 24 hours - apply equally to DFFs.
At discharge, a comprehensive falls-prevention and sarcopenia management plan is instituted, including home exercise guidance, nutritional support, and arranged community rehabilitation services to sustain gains and reduce readmission risk.
Secondary Prevention
A distal femur fracture in an older adult should be treated as a sentinel osteoporotic event, signalling an exceptionally high risk of imminent further fractures unless addressed decisively [35]. In accordance with updated national guidance, every geriatric femoral fracture patient warrants prompt osteoporosis evaluation and treatment initiation. This begins with a formal fracture-risk assessment (typically FRAX) followed by immediate commencement of bone-protective therapy. The 2024-25 National Osteoporosis Guideline Group (NOGG) guideline explicitly advocates starting anti-osteoporotic medication immediately after any fragility fracture, recognising that re-fracture risk is highest in the early post-fracture period [36].
First-line agents are antiresorptive agents such as oral bisphosphonates, IV zoledronate, or denosumab if bisphosphonates are contraindicated. In very high-risk individuals (e.g. multiple vertebral fractures or recurrent break), anabolic therapies such as romosozumab or teriparatide may be warranted followed by antiresorptive maintenance [37,38]. Crucially, all patients must be referred to a Fracture Liaison Service (FLS) as part of secondary prevention. A coordinator-led FLS ensures timely evaluation of falls risk, secondary contributors, treatment initiation, and long-term adherence monitoring. The NOGG mandates that every fragility fracture patient has access to a multidisciplinary FLS, with robust evidence demonstrating substantial improvements in osteoporosis treatment uptake and adherence [35,36].
In summary, geriatric distal femoral fractures are red flag indicators of underlying osteoporosis. Optimal management must therefore integrate acute fracture care with immediate risk stratification, bone-directed pharmacotherapy, and seamless FLS referral, fully aligned with contemporary NOGG standards.
Best Practice Tariffs and Hip Fracture Database
Fragility distal femoral fractures in older adults are now incorporated into the UK Falls & Fragility Fracture Audit Programme. In 2021/22, the National Hip Fracture Database (NHFD) extended the Best Practice Tariff (BPT) for hip fractures to encompass the entire femur, including shaft and distal femur fractures [3,5]. This brings DFF management within the same audited, incentivised framework that has revolutionised hip fracture care: standardising time-to-surgery, orthogeriatric co-management, comprehensive assessments, early rehabilitation, and secondary prevention. Core BPT criteria - surgery within 36h, geriatrician input, multidisciplinary rehabilitation, and evaluations of falls and bone health - are directly linked to enhanced survival and reduced morbidity in hip fracture populations, with comparable gains anticipated for DFFs when consistently implemented [39,40].
This BPT expansion will drive systematic data collection, enabling departmental benchmarking and continuous quality improvement. Hospitals are required to report eligible DFF cases, track key performance indicators) and leverage feedback to address care deficiencies. Collectively, incorporation into national audits is expected to improve outcomes by expediting definitive surgery, embedding geriatric optimisation, promoting day-one physiotherapy, and ensuring prompt secondary prevention through Fracture Liaison Services. This will turn a historically neglected pathway into one with measurable and accountable quality [3,5].
Conclusion
Distal femoral fractures in frail older adults carry mortality and morbidity comparable to hip fractures, yet until recently they have been managed without the structured orthogeriatric pathways, national audit, or financial incentives that have transformed hip-fracture outcomes. The extension of the Best Practice Tariff and National Hip Fracture Database to include DFFs provides a pivotal opportunity to close this historic performance gap. The integrated multidisciplinary pathway presented - characterised by early orthogeriatric co-management, systematic pre-operative optimisation, surgical constructs that prioritise immediate weight-bearing, day-one mobilisation, and mandatory secondary fracture prevention—directly addresses the principal drivers of adverse outcome in this frail population. Real-world orthogeriatric models already demonstrate reduced complications, shorter length of stay, lower mortality, and substantial cost savings; the same benefits are now achievable for DFF patients.
With national audit now in place, hospitals can benchmark performance, reduce unwarranted variation, and drive continuous improvement using hip-fracture-aligned key performance indicators. Full adoption of this evidence-based, orthogeriatric-led approach will finally grant distal femoral fractures the same urgency, rigor, and accountability long afforded to hip fractures, delivering equitable, high-quality care and markedly better survival and functional recovery for one of the most vulnerable groups in trauma surgery.
Key points
- Distal femoral fractures are akin to hip fractures and should be managed in a similar manner
- Core Model: Orthogeriatric Co-Management (OGCM) from admission with CGA < 72h, comorbidity optimisation and deprescribing
- Pre-op: TXA, anaemia correction, delirium bundle, VTE prophylaxis, surgery < 24-48h
- Surgery: choose construct for immediate WBAT - IMN (extra-articular), locking plates (articular/periprosthetic), nail-plate (complex), DFR (unsalvageable) - and document an explicit postoperative WB order
- Use opioid-sparing multimodal analgesia with regional nerve blocks to support early mobilisation
- Rehab & Bone Health: Deliver day-one mobilisation with physio-led rehab, FRAX, start bone-health therapy with FLS referral
- New DFF inclusion in NHFD/BPT integrated audit, KPIs, quality improvement
Availability of Data and Materials
All the data and materials are included in this review article.
Author Contributions
The concept of this article was created by CC. Resources, analysis and data acquisition were done by LC and JC. Drafts were created by JC, LC and CC. Final revisions and oversight by CC. All authors participated equally and all hold accountability for its contents.
Ethics Approval and Consent to Participate
All images were obtained during routine hospital care. They are used in this publication with full written consent and at the free will of the patients concerned. Any external images have been fully referenced.
Acknowledgement
Not applicable.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Gao F, Liu G, Ge Y, Tan Z, Chen Y, et al. (2023) Orthogeriatric co-managements lower early mortality in long-lived elderly hip fracture: A post-hoc analysis of a prospective study. BMC Geriatr 23: 571.
- Loosen A, Fritz Y, Dietrich M (2019) Surgical Treatment of Distal Femur Fractures in Geriatric Patients. Geriatr Orthop Surg Rehabil 10: 2151459319860723.
- Chess C, Carpenter C, Muir D, Duncan J (2025) Management of Distal Femoral Fractures in the Elderly. Br J Hosp Med (Lond) 86: 1-14.
- Tahoun M, Collins T, Tahoun R, Kafagi AH, et al. (2024) Clinical Audit to Assess Orthogeriatrician Input to the Management of Elderly Trauma Patients. Cureus 16: 65173.
- National Hip Fracture Database, Royal College of Physicians (2023) 15 years of quality improvement: The 2023 National Hip Fracture Database report on 2022. FFFAP, London, UK.
- Liu T, Zhang X, Zhang J, Ye P, Yang M, et al. (2024) Effect of the orthogeriatric co-management on older hip fracture patients with multimorbidity: A post-hoc exploratory subgroup analysis of a non-randomised controlled trial. J Orthop Surg Res 19: 780.
- Vleeshouwers K, Beert J, Boonen A, Janssen DJA, Dejaeger M, et al. (2025) The effects of in-hospital orthogeriatric care on health-related quality of life: A systematic review and meta-analysis. Age Ageing 54: afaf106.
- Prestmo A, Hagen G, Sletvold O, Helbostad JL, Thingstad P, et al. (2015) Comprehensive geriatric care for patients with hip fractures: A prospective, randomised, controlled trial. Lancet 385:1623-1633.
- Oberai T, Laver K, Crotty M, Killington M, Jaarsma R (2018) Effectiveness of multicomponent interventions on incidence of delirium in hospitalized older patients with hip fracture: a systematic review. Int Psychogeriatr 30: 481-492.
- Puckeridge G, Terblanche M, Wallis M, Fung YL (2019) Blood management in hip fractures; are we leaving it too late? A retrospective observational study. BMC Geriatr 19: 79.
- Chen L, Zong W, Luo M, Yu H (2024) The impact of comprehensive geriatric assessment on postoperative outcomes in elderly surgery: A systematic review and meta-analysis. PLoS One 19: 0306308.
- Carson JL, Stanworth SJ, Guyatt G, Valentine S, Dennis J, et al. (2023) Red Blood Cell Transfusion: 2023 AABB International Guidelines. JAMA 330: 1892-1902.
- Centre for Perioperative Care (2022) Guideline for Management of Anaemia in the Perioperative Pathway. CPOC, London, UK.
- Lan S, Liang S, Wu H, Deng S, Sun K, et al. (2024) Strategies to prevent postoperative delirium: A comprehensive evaluation of anesthesia selection and drug intervention. Front. Psychiatry 15: 1518460.
- Veronese N, Solimando L, Bolzetta F, Maggi S, Fiedorowicz JG, et al. (2024) Interventions to prevent and treat delirium: An umbrella review of randomized controlled trials. Ageing Res Rev 97: 102313.
- Viamont-Guerra MR, Guimarães R, Bridges C, Antonioli E, Lenza M (2024) Ultra-early versus early surgery for hip fracture. Cochrane Database Syst Rev 6: CD015697.
- Bolhofner BR, Carmen B, Clifford P (1996) The results of open reduction and Internal fixation of distal femur fractures using a biologic (indirect) reduction technique. J Orthop Trauma 10: 372-377.
- Karaytug K, Alpan B, Bayram S, Valiyev N, Bilgiç B, et al. (2022) Long-term results of different surgical options in the management of solitary enchondroma. ANZ J Surg 92: 1809-1813.
- The Bone School (2025) Distal Femur Fractures. The Bone School.
- Garala K, Ramoutar D, Li J, Syed F, Arastu M, et al. (2022) Distal femoral fractures: A comparison between single lateral plate fixation and a combined femoral nail and plate fixation. Injury 53: 634-639.
- Christ AB, Hornicek FJ, Fabbri N (2021) Distal femoral replacement - Cemented or cementless? Current concepts and review of the literature. J Clin Orthop Trauma19: 11-16.
- Morris H, Cameron C, Vanderboor C, Nguyen A, Londahl M, et al. (2023) Hip fractures in the older adult: orthopaedic and geriatric shared care model in Southland, New Zealand-a 5-year follow-up study. BMJ Open Qual 12: 002242.
- British Orthopaedic Association (2019) BOASt - The Care of the Older or Frail Orthopaedic Trauma Patient. BOAST, London, UK.
- Henken E, König HH, Becker C, Büchele G, Friess T, et al. (2024) Health-economic evaluation of orthogeriatric co-management for patients with pelvic or vertebral fragility fractures. BMC Geriatr 24: 657.
- Eamer G, Saravana-Bawan B, van der Westhuizen B, Chambers T, Ohinmaa A, et al. (2017) Economic evaluations of comprehensive geriatric assessment in surgical patients: A systematic review. J Surg Res 218: 9-17.
- Jin Z, Hu J, Ma D (2020) Postoperative delirium: Perioperative assessment, risk reduction, and management. Br J Anaesth 125: 492-504.
- Kim YH, Kim NY, Ryu S (2022) Effects of non-pharmacological interventions for preventing delirium in general ward inpatients: A systematic review & meta-analysis of randomized controlled trials. PLoS One 17: 0268024.
- Duan R, Cao L, Zhang H, Li P, Wu X, et al. (2024) The effect of fascia iliaca compartment block on postoperative delirium in elder adults undergoing hip surgery: A systematic review and meta-analysis of randomized controlled trials. Int J Orthop Trauma Nurs 54: 101122.
- National Institute for Health and Care Excellence (NICE) (2023) Delirium: Prevention, diagnosis and management in hospital and long-term care (CG103). NICE, London, UK.
- Lisk R, Yeong K, Fluck D, Robin J, Fry CH, et al. (2023) An orthogeriatric service can reduce prolonged hospital length of stay in hospital for older adults admitted with hip fractures: a monocentric study. Aging Clin Exp Res 35: 3137-3146.
- Tazreean R, Nelson G, Twomey R (2022) Early mobilization in enhanced recovery after surgery pathways: Current evidence and recent advancements. J Comp Eff Res 11: 121-129.
- Aebischer AS, Gouk CJC, Steer R (2025) Early weight-bearing following distal femur fracture fixation - a systematic review and meta-analysis. ANZ J Surg 95: 1108-1114.
- Haller JM, Marchand LS, Higgins TF, O'Toole RV, Reider L (2024) Surgical management and weight-bearing recommendations for geriatric distal femur fractures. OTA Int 7:
- McDonough CM, Harris-Hayes M, Kristensen MT, Overgaard JA, Herring TB, et al. (2021) Physical Therapy Management of Older Adults With Hip Fracture. J Orthop Sports Phys Ther 51: CPG1-CPG81.
- Kerschan-Schindl K, Widhalm H, Pataraia A, Nicolakis P, Frossard M, et al. (2024) Sentinel fracture: the necessity of improved post-fracture care. Wiener Medizinische Wochenschrift 175: 3-10.
- National Osteoporosis Guideline Group (NOGG) (2024) Clinical guideline for the prevention and treatment of osteoporosis. NOGG, London, UK.
- Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, et al. (2014) Clinician’s Guide to Prevention and Treatment of Osteoporosis. Osteoporos Int 25: 2359-2381.
- Gregson CL, Armstrong DJ, Bowden J, Cooper C, Edwards J, et al. (2022) UK clinical guideline for the prevention and treatment of osteoporosis. Arch Osteoporos 17: 58.
- Griffin XL, Achten J, Parsons N, Costa ML, WHiTE collaborators (2021) Does performance-based remuneration improve outcomes in the treatment of hip fracture? Bone Joint J 103: 881-887.
- NICE (2019) 2019 surveillance of Hip fracture: management (NICE guideline CG124). NICE, London, UK.
Citation: Chess C, Crocker L, Cunliffe J (2025) Optimising Distal Femoral Fractures in Older Adults: An MDT and Orthogeriatric Model. HSOA J Gerontol Geriatr Med 11: 273.
Copyright: © 2025 Christian Chess, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

