
Painful Mass of the Neck coming down to Diagnosis of Takayasu’s Arteritis: A Case Report
*Corresponding Author(s):
Bahar Kayahan SirkeciDepartment Of Head And Neck Surgery, LIV Hospital Ear Nose Throat Disease, Yuksek Ihtisas University Medical Faculty, Ankara, Turkey
Tel:+90 5336576826,
Email:baharkayahan@hotmail.com
Abstract
Takayasu’s Arteritis, is a rare, chronic idiopathic vasculitis which affects the large vessels in the body and the patients are usually young women. The aorta and its main branches are the primary vessels affected, with the most typical features reflected as ischemia or aneurysm formation. With Takayasu'sArteritis being a rare condition and its acute phase presentation often similar to, diagnosis is often difficult.
Here is presented a case report of a young woman with Takayas’s Arteritis, who presented a painful, tender mass localized anterior aspect of sternocleido mastoid muscle. The patient was investigated with a number of imaging modalities and diagnosed with Takayasu's Arteritis, involving left common and internal carotid arteries. She was treated as per protocol for Takayasu's Arteritis.
This case report highlights that a differential diagnosis should never be dispelled based upon a "typical" history. The importance of modern day imaging techniques such as CT and MRI can often be paramount to confirming a diagnosis and the extent of the pathology.
Keywords
Carotidynia; Inflammatory disease; Lymphadenopathy; Takayasu’s arteritis
INTRODUCTION
Takayasu’s Arteritis (TA) is a chronic idiopathic vasculitis that variably involves the aorta and/or its main branches and the coronary and pulmonary arteries in 50-80%. Inflammation results in stenosis, occlusion or aneurysm formation [1-3]. Aneurysms may rarely progress to vascular rupture and death. TA is a difficult disease to deal with. First, early diagnosis is difficult and requires clinical awareness and suspicion. Second, and even more important, is the lack of standard and reliable parameters reflecting disease activity [4].
The incidence of TA is about 2/10,000 person-years, with ten-fold predominance in women, especially under age of 40. There is a marked ethnic preference, with high prevalence rates in Asian countries, while less common in Caucasian populations [1,2].
Here is reported a case of TA which presented with symptoms and signs of painful neck fullness, and got the TA diagnose with neck Ultrasound (US), Computerized Tomography (CT) and Magnetic Resonance Imaging (MRI).This case report highlights the importance of physical examination, clinic suspicion, differential diagnoses and the importance of modern day imaging in the diagnosis.
CASE PRESENTATION
A 38-year old female presented to our clinic with a history of left submandibular tenderness, pain with neck movement and dullness. The pain was of sudden onset, started two days ago. The pain was increasing especially elevating the head while moving it toward the contralateral side. She first appealed to her dentist to check if there was a problem regarding teeth, after examination the dentist consulted the patient our clinic in case of sialoadenitis or lymph adenopathy. During anamnesis the patient gave the information that she had leftsided tinnitus for a week ago and sometimes she felt her heartbeat in her left ear. Her physical examination was in normal ENT examination except for solid tenderness and fullness between left submandibular gland and anterior border of left sternocleidomastoid muscle. There was not any lymph node or well-bordered mass in this region. There is not any systemic disease or regular medication intake, in her family history there was hypertension only.
A neck ultrasound was carried out to investigate differential diagnoses. An increased wall thickness from the left carotid bulbus to left internal carotid artery was detected, causing a suspicion of dissection. And the pain was named as “carotidynia” from that moment. She immediately went under CT angiography, there was not any leakage through the carotid system but wall thickening, vertically 3cm, on the left carotid bulbus and distal of the left common carotid artery was detected, also there was contour irregularity on the left internal carotid artery origin which was accepted as an intra mural hematoma or inflammatory vasculitis process (Figure 1).
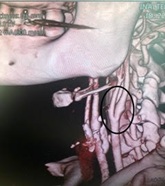
Figure 1: The wall thickening, on the left carotid bulbus and distal of the left common carotid artery, CT angiography.
The patient was consulted to rheumatology department, her blood tests were taken; Erythrocyte Sedimentation Rate (ESR) was 30mm, serum amyloid protein was 0.76 mg/dL; ENA panel, Anti dsDNA, Anticardiolipin antibody IgG and IgM, AntiBeta-2 antibody IgM and IgG, Anti CCP, ANA, p-ANCA and Lupus anticoagulant were negative, C-reactive Protein (CRP) and Rheumatoid Factor (RF) levels was in normal range. It was especially noted that pulse was weaker on the left arm. As an initial diagnosis of TA, neck MRI with intravenous contrast was carried out and vasculitis process was confirmed involving distal part of left common carotid artery, carotid bifurcation and proximal internal carotid artery wall (Figures 2 and 3). Diagnosed with TA, the medical treatment is scheduled as; methyl prednisolon 1g once-a-day (OD) for three days followed by prednisolone 1mg/kg (60mg) for two weeks was commenced, along with my cophenolatemofetil 500mg per oral (PO) bis in die (BD), acetyl salicyclic acid 100mg PO OD, Enoxaparine sodium 6000 anti-Xa IU-0.6 ml. These were well tolerated with no side effects experienced. After two weeks of treatment patient was evaluated on control appointment by both ENT and the rheumatology department. Fullness was still going on but tenderness almost diminished. Prednisolone dosage was decreased to 30mg PO OD / 4 weeks, 20 mg PO OD /4 weeks, 10mg/ 4 weeks and then stopped; and mycophenolate mofetil was increased to 750 mg PO BD. It has been 10 months since the patient presented and regular follow-ups continue at increasing intervals from TA perspective, she remains without any complaints.
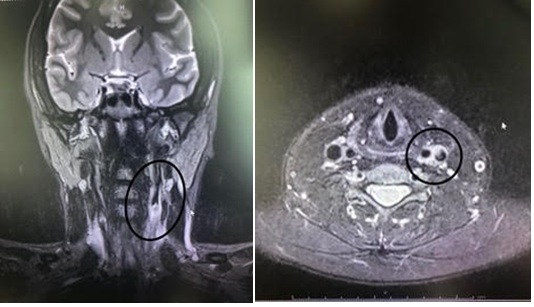 Figures 2 and 3: Vasculitis process involving distal part of left common carotid artery, carotid bifurcation and proximal internal carotid artery wall.
Figures 2 and 3: Vasculitis process involving distal part of left common carotid artery, carotid bifurcation and proximal internal carotid artery wall.
DISCUSSION
TA is a rare, large-vessel arteritis of unknown etiology. It is a life-threatening disease without intensive treatment [1-3]. The 5-year survival is 92.9% and 10-year survival is 87.2 % [2]. Histologically, it is characterized by a granulomatous infiltrative process of the arterial wall (acute stage) with marked intimal proliferation and fibrosis of the media and adventitia (fibrotic stage), resulting in severe stenosis, occlusion or aneurysmal dilation (from extensive destruction of elastic fibers in the media) [4,5].
The clinical manifestations of the disease are divided into early and late phases. The early or pre-pulse less phase is often characterized by non-specific signs and general symptoms of systemic inflammation (fever, weight loss, night sweats, weakness, myalgia, arthralgia), whereas the late or pulse less phase (consequences of vascular inflammation or fibrosis) may be associated with symptoms of ischemia of limb, renovascular hypertension, pulmonary hypertension, pulmonary embolism, myocardial ischemia and neurological symptoms [3-6].
The term carotidynia was defined as “carotid pain by Fay in 1927, to describe the patients presenting with dull, throbbing pain directly over the carotid artery (either unilateral or bilateral) that was exacerbated with light pressure. In 1988, the International Headache Society (IHS) declared acute idiopathic carotidynia to be a separate entity using four clinical criteria for diagnosis; including appropriate investigations not revealing structural abnormality [7]. In 1994, the validity of the HIS classification of carotidynia was questioned by a review and the controversy led the HIS to remove carotidynia as a distinct entity, instead referring it as a syndrome of unilateral neck pain. Today, carotidynia remains as a controversial subject. Many authors continue to use the term to describe neck pain due to any etiology, whereas some maintain that it is a separate disease entity [7,8].
Carotidynia is a neck pain syndrome associated with tenderness on palpation over the carotid bifurcation. The pain is mild to moderate intensity typically dull, throbbing and continuous just like in our case. The pain may be aggrevated by swallowing, coughing, sneezing or elevating the head while moving it toward the contralateral side. Carotidynia has been reported in 32% of patients with TA. Differential diagnosis for carotidynia includes large-vessel vasculitis such as TA and temporal arteritis, arteriosclerosis, thrombosis, dissection, aneurysm, pharyngitis, lymphadenitis, submandibular gland disease and thyroiditis [3].
Although conventional angiography has been the gold standard imaging tool for diagnosis and evaluation of TA, being invasive with procedural morbidity and mortality risks it is not so commonly used. The initial diagnosis of TA is made using serological markers, including CRP and ESR, combined with imaging modalities including US, CT angiography, MRI and FDG-PET if necessary. According to the recommendations for use of imaging in large-vessel vasculitis outlined by the European League Against Rheumatism (EULAR), MRI should be used as the first imaging test for diagnosis TA. MRI with enhancement of the thickened walls with gadolinium contrast suggests the active phase of TA. FDG-PET, CT and US as alternative imaging modalities in patients suspected TA [3,5]. During our diagnosis process; neck US was wanted to understand the etiology of neck pain, with the suspicion of US, CT angiography was carried out to understand if there was a leakage through the arterial wall. The contrasted MRI had a key role to name the disease TA.
Due to the rarity of TA and the lack of international collaborative studies, treatment modalities are proposed based on clinical observations and experts’ opinions. Corticosteroids (CS) remain the main stay of medical treatment; however, TA is often resistant to treatment, so pulse therapy with methyl prednisolone should be considered. Several immunosuppressive agents such as metothrexate, cyclophosphamide, azathioprine, cyclosporine and mycophenolate mofetil have been used as steroid-sparing agents in TA patients with varying efficacy. Obstructive lesions need to be managed by revascularization techniques such as angioplasty and surgery [3,6,9,10].
In conclusion, carotidynia is a painful symptom that may be underrated, but should be taken into consideration in case of non-palpable neck pain. It might be a clinical sign of Takayasu’s arteritis and other large-vessel vasulitis. Non-invasive imaging modalities such as US, CT and MRI allow earlier diagnosis than conventional imaging. MRI enhanced with gadolinium and PET scan offer additional information regarding the staging, dynamic evaluation and management of Takayasu’s arteritis.
ACKNOWLEDGEMENTS
The author declares that informed consent was obtained from the patient referred on this report regarding the publication of all included information.
DISCLOSURE STATEMENT
The author hereby declares having no conflicts of interest to declare regarding the publication of this article.
FUNDING SOURCES
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
STATEMENT OF ETHICS
This research involves the patient’s informed consent that was given willingly. In addition to the patient's informed consent, the research was conducted ethically in accordance with the World Medical Association Declaration of Helsinki.
REFERENCES
- O'Connor MB, Murphy E, O'Donovan N, Murphy M, Phelan MJ, et al. (2008) Takayasu's Arteritis presenting as a dissecting aortic aneurysm history: a case report. Cases J 1: 52.
- Andrzejewska K, Starba A, Misterska-Skóra M, Wiland P, Guzi?ski M (2017) Palpable mass of the neck in the course of Takayasu arteritis. Reumatologia 55: 48-52.
- Zeina AR, Slobodin G, Barmeir E (2008) Takayasu's arteritis as a cause of carotidynia: clinical and imaging features. Isr Med Assoc J 10: 158-159.
- Keser G, Direskeneli H, Aksu K (2014) Management of Takayasu arteritis: a systematic review. Rheumatology (Oxford) 53: 793-801.
- Oguro E, Ohshima S, Kikuchi-Taura A, Murata A, Kuzuya K, et al. (2019) Diffusion-weighted Whole-body Imaging with Background Body Signal Suppression (DWIBS)as a Novel Imaging Modality for Disease Activity Assessment in Takayasu's Arteritis. Intern Med 58: 1355-1360.
- Guo J, Zhang G, Tang D, Zhang J (2017) A case report of Takayasu arteritis with aortic dissection as initial presentation. Medicine (Baltimore) 96: e8610.
- Elkins A, Barakate M, Henderson J, Grieve S (2015) A Pain in the Throat: A 19-year History of Symptoms Relating to the Carotid Artery. Wien Klin Wochenschr 127: 143-145.
- Stanbro M, Gray B, Kellicut D (2011) Carotidynia: Revisiting an Unfamiliar Entity. Ann Vasc Surg 25: 1144-1153.
- Watanabe Y, Miyata T, Tanemoto K (2015) Current Clinical Features of New Patients With Takayasu Arteritis Observed From Cross-Country Research in Japan: Age and Sex Specificity. Circulation 132: 1701-1709.
- Nasser M, Cottin V (2018) The Respiratory System in Autoimmune Vascular Diseases. Respiration 96: 12-28.
Citation: Sirkeci BK (2020) Painful Mass of the Neck coming down to Diagnosis of Takayasu’s Arteritis: A Case Report. J Otolaryng Head Neck Surg 6: 43
Copyright: © 2020 Bahar Kayahan Sirkeci, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

