
Pancreatic Function Enzymes in Patients on Maintenance Hemodialysis in Cameroon
*Corresponding Author(s):
Francois Folefack KazeDepartment Of Internal Medicine And Specialties, Faculty Of Medicine And Biomedical Sciences, University Of Yaoundé 1, Yaounde, Cameroon
Tel:+237 699333467,
Email:f_kaze@yahoo.fr
Abstract
Introduction
End stage kidney disease is associated with hemodynamic, biochemical and physiological abnormalities of pancreas and reduced renal clearance of pancreatic enzymes.
Objective
Assess the pancreatic function enzymes in patients on maintenance hemodialysis in Cameroon.
Patients and methods
We conducted a hospital-based cross-sectional study from December 2017 to May 2018 at the Yaounde University Teaching Hospital dialysis unit. We included all consenting adults patients who provided a written informed consent and has been on hemodialysis for more than three months with a native arterio-venous fistula. We excluded patients presenting signs and symptoms of pancreatitis and any conditions which can increase serum pancreatic enzymes. We collected demographic, clinical and laboratory (calcemia, phosphoremia, parathormone, amylasemia and lipasemia) data. Parametric, non-parametric and correlations tests were used to compare variables.
Results
We included 60 (68.3% males) participants with a mean (SD) age of 47.4 (15.8) years and duration in dialysis of 2.1 (0.6) years. Hypertension (30%), diabetes mellitus (25%) and chronic glomerulonephritis (23.3%) were the main baseline nephropathy. There were 7 (11.7%) overweight/obese. Hypercalcemia was noticed in 2 (3.3%) patients whereas hyperphosphatemia and increased parathormone levels were observed in 35 (58.3%) and 28 (46.7%) patients respectively. The mean (SD) lipasemia and amylasemia was 130.6 (43.3) UI/L and 131.8 (62.5) UI/L respectively. Hyperlipasemia and hyperamylasemiawereobservedin59 (98.3%) and 48 (80%) participants respectively. The lipasemia was three times above the upperlimitsin10 (24.4%) participants. Only lipasemia was positively and significantly correlated with amylasemia (r=0.5; p<0.001).
1.5 Conclusion
We observed that almost all patients had hyperlipasemia with nearly a quarter having values above the cut-off point to diagnose acute pancreatitis and eight out of ten had hyperamylasemia. There was a positive correlation between lipasemia and amylasemia.
Keywords
Amylasemia; Cameroon; Hemodialysis; Lipasemia
INTRODUCTION
Chronic Kidney Disease (CKD)is one of the major public health threat worldwide [1]. It evolution to End Stage Kidney Disease (ESKD) affects various systems and organs among which the pancreas. In ESKD, patients are more likely to develop pancreatic diseases [2-4]. Chronic uremia is associated with hemodynamic, biochemical and physiological abnormalities of pancreas as well as reduced renal clearance of pancreatic enzymes [4,5]. Studies revealed that in asymptomatic patients on maintenance hemodialysis, the mean serum pancreatic enzymes levels are significantly higher compare to controls; this increase concerns serum amylase and lipase which can exceed the cut-off point of diagnosis value of acute pancreatitis, making difficult his diagnosis in such patients [6-8]. Despite the diagnosis difficulties, there is an increase incidence of acute pancreatitis in patients on chronic hemodialysis compare to general population; incidence increasing with the duration in dialysis [5, 9].
In sub-Saharan Africa, there is dearth of research evaluating the pancreatic function enzymes in patients on maintenance hemodialysis. Willing to fill a critical gap of knowledge regarding the subject in our setting, we conducted the present study which aimed to assess the pancreatic function enzymes in patients on maintenance hemodialysis in Cameroon.
PATIENTS AND METHODS
Study design and setting
We conducted a hospital-based cross-sectional study from December 2017 to May 2018 at the dialysis unit of the Yaounde University Teaching Hospital (YUTH). The center has a capacity of 10 hemodialysis generators and operates from Monday to Saturday for chronic hemodialysis patients. All chronic hemodialyzed patients had two hemodialyisis sessions of 4 hours duration each per week. The dialysis is performed with Nipro SurdialTM-55 Plus generators (Nipro Medical Devices, Osaka, Japan), synthetic polysulfone dialysis membrane, bicarbonate and unfractionned heparin. Ethical approval and administrative authorization were obtained from the institutional ethical board of the faculty of medicine and biomedical sciences of the Yaounde 1 university and the YUTH respectively.
Data collection
We included all consenting adults (≥18 years old) patients who provided a written informed consent and has been on hemodialysis for more than three months with the use of a native arterio-venous fistula. We excluded patients presenting the signs and symptoms of pancreatitis and any conditions which can increase pancreatic enzymes such as alcohol intake and drugs use. A self-designed and pre-tested questionnaire was used to collect demographic (age and sex), clinical (blood pressure, weight, height, duration in dialysis, comorbidities, baseline nephropathy) and laboratory (hemoglobin, C reactive protein, calcemia, phosphatemia, parathormone, amylasemia and lipasemia) data. We collected 5ml of whole blood in a dry tube from the arterial dialysis line before the begining of the dialysis session. The serum was used for lipase and amylase analysis. The activity of amylase was determined by a kinetic blocked Ethylene p-Nitrophenyl-Maltoheptaoside (E-pNPG7) method while colorimetric enzymatic method was used for lipase. Others laboratory analysis were collected from the dialysis file of patients used for their routine follow-up. All analysis were performed in the biochemistry laboratory of the YUTH.
De?nitions
Overweight and/or obesity were defined by Body Mass Index (BMI) ≥25kg/m2. Hypertension was diagnosed in the Presence of Systolic (SBP) ≥140mmHg and/or a Diastolic Blood Pressure (DBP) ≥90mmHg at the beginning of the dialysis session. Hypercalcemia corresponds to serum calcium level >100mg/l whereas hyperphosphatemia was phosphate level >50mg/l. Increase Parathormone (PTH) level was considered when above 9 times the upper limits of the normal value (>70pg/ml). Hyperlipasemia was a serum lipase level >59UI/L while hyperamylasemia corresponds to serum level >80UI/L.
Statistical analysis
Data were entered and coded using EPI info version 7.0 and analysed using Statistical Package for Social Science (SPSS) version 21.0. We used means and standard deviations for continuous variables. Frequencies and proportions were computed for categorical variables. Chi-square and/or fisher tests and Student t-test and/or Mann Whitney tests were used to compare qualitative and quantitative variables. The Correlation between variables was performed using the Pearson and Spearman’s correlation tests. A p value was considered statistically significant at <0.05.
RESULTS
Sociodemographic, clinical and paraclinical characteristics of study population
We included 60 participants among whom 41 (68.3%) men with a Mean (SD) age of 47.4 (15.8) years. The Mean (SD) duration in dialysis was 2.1 (0.6) years ranging from 1 to 10 years. Hypertension (30%), diabetes mellitus (25%) and chronic glomerulonephritis (23.3%) were the main baseline nephropathy, figure 1. The main comorbidities observed were hypertension (76.7%), diabetes mellitus (25%), left ventricular hypertrophy (13.3%) and smoking (8.3%), figure 2. There was 7 (11.7%) overweight/obese and 40 (66.7%) hypertensive participants with no gender difference between the mean BMI, SBP and DBP (p>0.3), table 1. As presented in table 2, hypercalcemia was noticed in 2 (3.3%) patients whereas hyperphosphatemia and increased PTH levels were observed in 35 (58.3%) and 28 (46.7%) patients respectively. There was no gender difference in the mean of paraclinical parameters (p≥0.42).
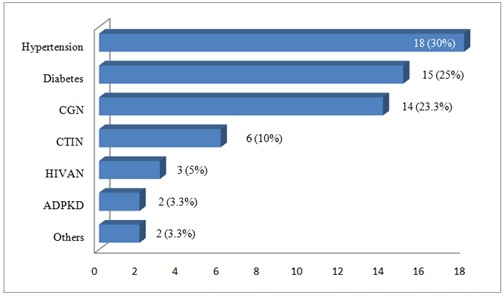 Figure 1: Distribution of baseline nephropathies.
Figure 1: Distribution of baseline nephropathies.
Note: ADPKD: Autosomal Dominant Polycystic Kidney Disease; CGN: Chronic Glomerulonephritis; CTIN: Chronic Tubulointerstitial Nephritis; HIVAN: HIV Associated Nephropathy.
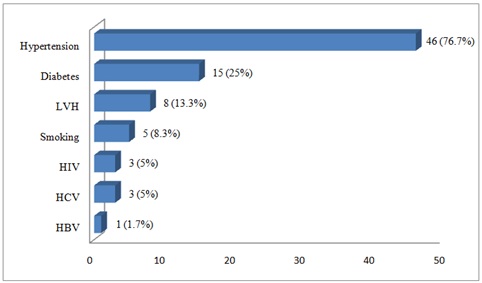 Figure 2 : Distribution of comorbidities.
Figure 2 : Distribution of comorbidities.
Note: HBV: Hepatitis B Virus; HCV: Hepatitis C Virus; HIV: Human Immunodeficiency Virus; LVH: Left Ventricular Hypertrophy.
|
Variables |
Total |
Male |
Female |
p-Value |
|
N (%) |
60 (100) |
41 (68.3) |
19 (31.7) |
|
|
Mean age (SD), years |
47.4 (15.8) |
48.3 (15.5) |
45.4 (16.6) |
0.50 |
|
Mean duration in dialysis (SD), years |
2.1 (0.6) |
2.3 (0.7) |
1.5 (0.4) |
0.09 |
|
Mean BMI (SD), kg/m2 |
21.8 (3.7) |
21.4 (2.6) |
22.5 (5.3) |
0.30 |
|
Over weight/obese, n (%) |
7 (11.7) |
|
|
|
|
Mean SBP (SD), mmHg |
153.3 (27.9) |
153.4 (24.3) |
153.15 (35.3) |
0.97 |
|
Mean DBP (SD), mmHg |
87.4 (27.9) |
78.8 (13.2) |
86 (21.9) |
0.96 |
|
Hypertension, n (%) |
40 (66.7) |
|
|
|
|
Mean calcemia (SD), mg/l |
83.1 (10.5) |
82.2 (9.3) |
85.1 (13.1) |
0.42 |
|
Hypercalcemia, n (%) |
2 (3.3) |
|
|
|
|
Mean phosphatemia (SD), mg/l |
52.3 (26.5) |
51.6 (27.8) |
54 (24.3) |
0.79 |
|
Hyperphosphatemia, n (%) |
35 (58.3) |
|
|
|
|
Mean PTH (SD), pg/ml |
478.5 (276) |
446.3 (298) |
555.2 (320.1) |
0.56 |
|
Increase PTH, n (%) |
28 (46.7) |
|
|
|
|
Mean CRP (SD), mg/l |
34.8 (39.1) |
43.1 (40.9) |
15.2 (26.9) |
0.76 |
|
Mean hemoglobin (SD), g/dl |
8.9 (2.1) |
9 (2.2) |
8.8 (1.6) |
0.72 |
Table 1: Sociodemographic, clinical and paraclinical characteristics of study population.
Note: BMI: Body Mass Index; CRP: C Reactive Protein; DBP: Diastolic Blood Pressure; PTH: Parathormone; SBP: Systolic Blood Pressure; SD: Standard Deviation.
|
Variables |
Total |
Male |
Female |
p-Value |
|
N (%) |
60 (100) |
41 (68.3) |
19 (31.7) |
|
|
Mean amylasemia (SD), UI/L |
131.8 (62.5) |
123 (53.1) |
150.6 (77.5) |
0.89 |
|
Mean lipasemia (SD), UI/L |
130.6 (43.3) |
129 (44.8) |
134 (40.9) |
0.89 |
|
Hyperamylasemia, n (%) |
48 (80) |
33 (80.5) |
15 (78.9) |
0.96 |
|
Hyperlipasemia, n(%) |
59 (98.3) |
40 (97.6) |
19 (100) |
0.46 |
Table 2: Distribution of pancreatic function enzymes.
Note: SD: Standard deviation.
Distribution and correlation of pancreatic function enzymes tests
The Mean (SD) lipasemia was 130.6 (43.3)UI/L where as the Mean (SD) amylasemia was 131.8 (62.5)UI/L. We observed hyperlipasemia in 59 (98.3%) participants while hyperamylasemia was noticed in 48 (80%) of them. When considering the cut-off point of a three times increase of lipasemia used for the diagnostic of acute pancreatitis, 10 (24.4%) participants fulfilled this criteria, table 2. We did no observed any gender difference according to pancreatic function enzymes tests (p≥0.46).
Only lipasemia was positively and significantly correlated with amylasemia (r=0.5 ; p<0.001). None of the tested variables was correlated to lipasemia, noramylasemia (p>0.05), table 3.
|
Variables |
Amylasemia |
p-Value |
Lipasemia |
p-Value |
|
Age |
0.03 |
0.802 |
0.12 |
0.332 |
|
Duration in dialysis |
-0.41 |
0.755 |
-0.12 |
0.930 |
|
BMI |
0.20 |
0.125 |
0.19 |
0.143 |
|
Calcemia |
-0.01 |
0.945 |
-0.14 |
0.366 |
|
Phosphatemia |
0.04 |
0.799 |
0.05 |
0.720 |
|
PTH level |
0.08 |
0.775 |
0.42 |
0.151 |
|
CRP level |
-0.22 |
0.337 |
-0.36 |
0.103 |
|
Lipasemia |
0.50 |
<0.001 |
- |
- |
Table 3: Correlation between amylasemia, lipasemia and others variables.
Note: BMI: Body Mass Index; CRP: C Reactive Protein; PTH: Parathormone.
DISCUSSION
This study revealed that almost all chronic hemodialyzed patients in this Cameroon dialysis center had hyperlipasemia with nearly a quarter having values above the cut-off point to diagnose acute pancreatitis. There was eight out of ten with hyperamylasemia and only lipasemia was positively and significantly correlated with amylasemia.
We observed that chronic hemodialyzed Cameroon patients are mainly young adults with male predominance and slight increase of the mean duration in dialysis as previously reported in this setting [10,11]. The increase duration in dialysis could be explained by the increase number of the dialysis centers in the country. The baseline nephropathy, comorbidities as well as biological parameter were similar to those reported earlier in Cameroon [12,13].
This study showed an increase mean level of serum lipase and amylase as reported elsewhere [14]. The increase level of this enzymes could be related to the hemodynamic, biochemical and physiological abnormalities as well as reduced renal clearance of these enzymes in chronic hemodialyzed patients [4,5]. A quarter of study participants had higher level of serum lipase above the cut-off point for the diagnosis of acute pancreatitis in asymptomatic patients; this makes difficult the diagnosis of acute pancreatitis using this enzyme in dialysis patients as reported elsewhere [5-8,15]. This situation suggests that the instrumental imaging is mandatory to diagnose acute pancreatitis in such patients [16]. We found a positive and correlation between serum amylase and lipase as reported earlier suggesting the reduction of renal clearance of these enzymes in dialysis patients [6,8,14].
STRENGTH AND LIMITATIONS
The main limitations of this study are the reduce sample size and the absence of imaging tests of the pancreas which could have given us information on the structure of the organ. Nevertheless, this study is the first in Central Africa, to the very best of our knowledge, to assess the pancreatic function enzymes tests in patients on maintenance hemodialysis. These findings contribute to enrich data on the systemic consequences of chronic uremia in our setting. The cut-off value of serum lipase to diagnose acute pancreatitis in patients on maintenance hemodialysis should take into account the fact that up to a quarter of such asymptomatic patients had an increase value.
CONCLUSION
The present study shows that the majority of asymptomatic chronic hemodialyzed patients in this Cameroon center had an increase pancreatic function enzymes. We observed that almost all patients had hyper lipasemia with nearly quarter having values above the cut-off point to diagnose acute pancreatitis and eight out of ten had hyperamylasemia. We also noticed a positive and significant correlation between serum lipase and amylase.
LIST OF ABBREVIATIONS
ADPKD: Autosomal Dominant Polycystic Kidney Disease;
BMI: Body Mass Index;
CGN: Chronic Glomerulonephritis;
CKD: Chronic Kidney Disease;
CRP: C Reactive Protein;
CTIN: Chronic Tubulointerstitial Nephritis;
DBP: Diastolic Blood Pressure;
ESKD: End Stage Kidney Disease;
HBV: Hepatitis B Virus;
HCV: Hepatitis C Virus;
HIV: Human Immunodeficiency Virus;
HIVAN: Human Immunodeficiency Virus Associated Nephropathy;
LVH: Left Ventricular Hypertrophy;
PTH: Parathormone;
SBP: Systolic Blood Pressure;
SD: Standard Deviation;
YUTH: Yaounde University Teaching Hospital.
DECLARATIONS
Ethics approval and consent to participate
This study received administrative authorization from the Yaounde University Teaching Hospitals and was approved by the ethical board of the faculty of medicine and biomedical sciences of the Yaounde 1 university (Number: 0330/UY1/FMSB/VDRC/CSD) and all participants provided a written informed consent before enrolment.
Consent for publication
All authors gave their approval for publication
Competing interests
The authors report no conflicts of interest.
Funding
The authors did not receive any fund for this study.
Authors’ contribution statement
Study conception: FFK, COEZ, MPK
Clinical data collection and supervision: FFK, COEZ, EN, MPK, VJAM
Acquisition and validation of the biological data: FFK, HDFME, COEZ, EN, VJAM
Data analysis: FFK, MPH
Data interpretation: FFK, MPH
Manuscript drafting : FFK, MPH
Critical revision of the manuscript: HDFME, COEZ, EN, MPK, VJAM
Availability of data and materials
Data and materials are available with corresponding author which is the principal investigator. They can be consulted at any time upon request. However, the ethical clearance and the inform consent form did mention that patient data could be share to a third party.
Acknowledgement
We thank the Yaounde University Teaching Hospital’s biochemistry laboratory technicians.
REFERENCES
- World Kidney Day (2020) About World kidney day. World Kidney Day, Brussels, Belgium.
- Hou SW, Lee YK, Hsu CY, Lee CC, Su YC (2013) Increased risk of acute pancreatitis in patients with chronic hemodialysis: a 4-year follow-up study. PLoS One 8: 71801.
- Araki T, Ueda M, Ogawa K, Tsuji T (1992) Histological pancreatitis in end-stage renal disease. Int J Pancreatol 12: 263-269.
- Vaziri ND, Dure-Smith B, Miller R, Mirahmadi M (1987) Pancreatic pathology in chronic dialysis patients--an autopsy study of 78 cases. Nephron 46: 347-349.
- Ventrucci M, Campieri C, Di Stefano M, Ubalducci GM, Li Bassi S, et al. (1995) Alterations of exocrine pancreas in end-stage renal disease. Do they reflect a clinically relevant uremic pancreopathy? Dig Dis Sci 40: 2576-2581.
- Masoero G, Bruno M, Gallo L, Colaferro S, Cosseddu D, et al. (1996) Increased serum pancreatic enzymes in uremia: Relation with treatment modality and pancreatic involvement. Pancreas 13: 350-355.
- Stanescu A, Mayer D, Rosenthal J, Malfertheiner P (1990) Effect of chronic renal failure and hemodialysis on the pancreas-specific enzyme pattern in the serum. Leber Magen Darm 2: 83-89.
- Caruana RJ, Altman R, Fowler B, Blansit B, Chaudhary BA, et al. (1988) Correlates of amylase and lipase levels in chronic dialysis patients. Int J Artif Organs 11: 454-458.
- Chen HJ, Wang JJ, Tsay WI, Her SH, Lin CH, et al. (2017) Epidemiology and outcome of acute pancreatitis in end-stage renal disease dialysis patients: A 10-year national cohort study. Nephrol Dial Transplant 32: 1731-1736.
- Kaze FF, Kengne AP, Mambap AT, Halle MP, Mbanya D, et al. (2015) Anemia in patients on chronic hemodialysis in Cameroon: Prevalence, characteristics and management in low resources setting. Afr Health Sci 15: 253-260.
- Kaze FF, Ashuntantang G, Kengne AP, Hassan A, Halle MP, et al. (2012) Acute hemodialysis complications in end-stage renal disease patients: The burden and implications for the under-resourced Sub-Saharan African health systems. Hemodial Int 16: 526-531.
- Patrice HM, Pascal KA, Francois KF, Hilaire D, Solange DM, et al. (2020) Markers and risk factors for chronic kidney disease in sub-Saharan Africans: Baseline levels and 12-month trajectories in newly referred patients in Cameroon. BMC Nephrol 21: 101.
- Halle MP, Takongue C, Kengne AP, Kaze FF, Ngu KB (2015) Epidemiological profile of patients with end stage renal disease in a referral hospital in Cameroon. BMC Nephrol 16: 59.
- Khan SI, Iqbal M, Chowdhury AA, Roy AS, Ahammed SU, et al. (2020) Comparison of serum amylase and lipase levels between predialysis and maintenance haemodialysis CKD Patients. Mymensingh Med J 29: 21-31.
- Barbara M, Tsen A, Rosenkranz L (2018) Acute pancreatitis in chronic dialysis patients. Pancreas 47: 946-951.
- Vidal E, Alberici I, Verrina E (2019) Acute pancreatitis in children on chronic maintenance dialysis. Pediatr Nephrol 34: 1501-1512.
Citation: Kaze FF, Kowo MP, Zang COE, Moor VJA, Fouda HDME, et al. (2020) Pancreatic Function Enzymes in Patients on Maintenance Hemodialysis in Cameroon. J Nephrol Renal Ther 6: 031.
Copyright: © 2020 Francois Folefack Kaze, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

