
Pathophysiology of Long-Term Post-Cesarean Complications: Novel Insight from Tissue Magnification Video-Recording
*Corresponding Author(s):
Clarel AntoineDepartment Of Obstetrics And Gynecology, New York University School Of Medicine, 530 First Ave, New York, 10016, United States
Tel:+1 2128263300,
Fax:+1 6465902699
Email:clarel.antoine@nyulangone.org
Introduction
Just over one century ago, the Cesarean operation was almost exclusively performed on a dead or dying mother to remove an infant, either dead or alive. During this time, it was avoided because of its high mortality rate [1]. The beginning of the 20th century was met with newer surgical developments, leading to the conservative Cesarean section introduced by Max Sanger [2] in Prague and the lower transverse uterine segment incision by Munro Kerr (1868-1960) [3,4] in Scotland. These contemporaneous operative techniques significantly reduced maternal mortality and morbidity. Sanger and Kerr laid the foundation for the Cesarean surgical procedures as practiced and modified over the past five decades, during which time improved maternal safety became achievable with antibiotic use, blood transfusion availability, anesthesia and high-standard neonatal care.
Today, Cesarean section is the most common operation in the United States, plateauing at 30-33% during the past decade [5], while the global rate has doubled from 10% to 21% during the past two decades with an increasing annual rate of 4% [6]. These disparities vary from 4% in some sub-Saharan African localities to 80% in others in Brazil [7]. Concurrent with the increasing global rates is an escalating post-Cesarean complication rate ranging from life-altering to life-threatening injuries [8,9]. While aggressive research and clinical applications abound in treating post-Cesarean sequelae [10,11], much work remains to uncover their etiology and offer preventative strategies.
Antoine and Timor-Tritsch, authors of the original article “A new era in teaching: how advanced optical recording technology could change the post-Cesarean delivery complication conundrum,” published in the American Journal of Obstetrics and Gynecology, Maternal-Fetal Medicine in November 2022, introduced a high-definition optical recording system to highlight Cesarean operative steps and surgical techniques and to give further insight into the underlying factors leading to long-term post-Cesarean sequelae [12].
History
In a historical overview of the Cesarean section, Antoine and Young captured more than one hundred years of surgical development of operative delivery [13]. They reported that in 1920 through 1970, the Cesarean uterine techniques in use were predominantly the work of Sanger and Kerr with a suprapubic transverse skin incision as described by German obstetrician Hermann Johannes Pfannenstiel [14]. In the 1970s, Michael Stark introduced an abdominal incision at Misgav-Ladach Hospital in Jerusalem based on the surgeon Joel-Cohen method for hysterectomy [15] and adapted a similar technique to Cesarean section [16]. His approach restricts the use of sharp instruments, prefers blunt entries, reduces blood loss, requires less suture material and results in time-saving.
Hundreds of publications in the past five decades have favorably compared the Misgav-Ladach method to the Pfannenstiel-Kerr for quick recovery, less post-operative analgesia requirement, and time and cost savings [17-19]. While these studies address short-term complications, there have been warnings of a lack of knowledge on long-term sequelae and the need for further research [20,21]. Despite the lack of conclusive evidence on future outcomes however, the Misgav-Ladach method has been proposed for universal use [22] and integrated into the commentary for standardizing Cesarean delivery surgical techniques [23]. The later proposal emphasized time and cost savings and the lack of a clear benefit compared to other methods. It has gained popularity in most Obstetrics and Gynecology resident training and is supported by present leaders in our field.
Long-Term Complications
Although Cesarean delivery (CD) is considered a safe procedure, it can also lead to immediate and long-term health effects and complications, which may affect women, children, and future pregnancies [8,9]. With millions of Cesareans performed annually, the long-term sequelae are alarming and mounting globally. A recent survey among obstetricians in one institution illustrates various techniques are employed without concern for potential adverse sequelae [24]. These include Cesarean scar pregnancy, placenta accreta spectrum, uterine rupture in future pregnancies, infertility, irregular bleeding, and pelvic pain in non-pregnant women. Complex management strategies have been formulated and actively researched to improve outcomes for mothers and newborns [10,11]. Laparoscopy, hysteroscopy, and other interventions have become critical to enhance the lifestyle of affected women [25]. In countries with minimal resources, the maternal mortality associated with PAS is disproportionately high [26]. The common risk factor linking these post-Cesarean health effects is the Cesarean surgical technique and subsequent healing [27-29].
Comment
The call for standardizing the Cesarean delivery technique highlights the urgent need to examine the method of individual obstetricians and accountability for maternal outcomes. Dahlke et al., emphasized their proposed approach's short-term benefits and endorsed omitting established steps, primarily for cost and time savings [23]. The emphasis on time savings in particular creates a generation of surgeons fixated on the finish line without adequate consideration of long-term risks and adverse maternal outcomes (Table 1).
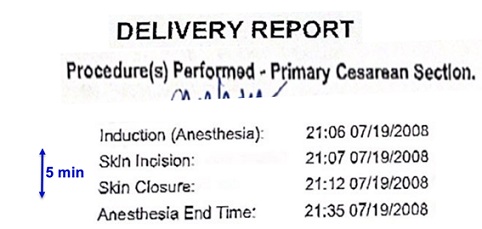 Table 1: Five minute-long Cesarean section.
Table 1: Five minute-long Cesarean section.
The pathophysiology of these consequences remains unsettled. The absence of statistical evidence of the benefit of harmless surgical steps is not necessarily proof of the evidence of absence justification. As for costs associated with severe adverse outcomes [30], no available data incorporates them in analyzing the alleged benefits of any proposed technique. The argument is simple however: time savings and cost in the operating room do not necessarily predict optimal outcomes. A century ago, the pioneers of Cesarean section emphasized avoiding the endometrium/decidua in the uterine closure [2-4]. This practice was universally standard until the 1970s when attention became focused on hurrying surgical techniques and unsound time/cost savings while omitting the additional effort required to exclude the endometrium in the uterine closure. However, a specific “Endometrium-Free Uterine Closure Technique” (EFCT) has been well documented as a risk reduction of abnormal placentation in subsequent pregnancies [29] and is associated with fewer and less severe uterine scar defects when compared with closures with unknown or endometrium inclusion [28].
An indiscriminate single-layer uterine closure is a risk factor for uterine scar defect [27]. These studies strengthened the rationale for layer-to-layer approximation and endometrium exclusion at closure [31]. In today’s practice and training however, consideration of the endometrium is mostly abandoned despite supporting research. Furthermore, the suggested omission of closing the peritoneal layers is premature, particularly as adhesion formation and related complications still need to be better understood [32,33]. We are confronted with increasing maternal morbidities and even death related to Cesarean deliveries, with limited explanation, misinterpretation of evidence while facing rushed changes in operative technique. A prematurely enforced technique on obstetricians would discourage accountability, promote blind adherence and venerate surgical haste rather than sound surgical principles. Wrong standardization is far worse than no standardization. Further high-quality research is required before established sound surgical principles can be abandoned.
The present-day technique of blunt stretching leading to layers not identified nor preserved does not consider the impact on long-term complications. A Gravida 2 Para 2, who underwent a primary CD under a recorded time of five minutes (Table 1) and a secondary CD for a ruptured uterus during a trial of labor, exemplifies the short-term benefits but also the costly long-term complications. This practice, which is not regulated, quantified by the medical community, or understood by the patients, merits further investigation, and the recording telescope can provide an effective tool to evaluate the accountability of surgical steps to subsequent outcomes and adds objectivity and transparency to our conventional research armamentarium. The introduction of video-photography documentation provides factual photographs of the healing result of specific surgical steps. Credible, unbiased follow-up documentation of any surgical step would further validate its worth for use in obstetrics. This latest tool pushes boundaries in research and education to expose the root causes of long-term post-Cesarean complications and ultimately improve maternal outcomes.
Disclosure
The author reports no conflict of interest.
References
- Harris RP (1881) Special statistics of the cesarean operation in the United States, showing the successes and failures in each state. The American Journal of Obstetrics and Diseases of Women and Children (1869-1919) 14: 341.
- Hem E, Børdahl PE (2003) Max Sänger - father of the modern caesarean section. Gynecol Obstet Invest 55: 127-129.
- Peleg D, Burke YZ, Solt I, Fisher M (2018) The History of the Low Transverse Cesarean Section: The Pivotal Role of Munro Kerr. Isr Med Assoc J 20: 316-319.
- Kerr JMM (1928) The technique of cesarean section, with special reference to the lower uterine segment incision. American Journal of Obstetrics and Gynecology 1928: 729-734.
- Hamilton BE, Martin JA, Osterman MJ (2021) Births: Provisional data for 2020. NVSS, CDC, Georgia, USA.
- Boerma T, Ronsmans C, Melesse DY, Barros AJD, Barros FC, et al. (2018) Global epidemiology of use of and disparities in caesarean sections. The Lancet 392: 1341-1348.
- Nakamura-Pereira M, do Carmo Leal M, Esteves-Pereira AP, Domingues RMSM, Torres JA, et al. (2016) Use of Robson classification to assess cesarean section rate in Brazil: the role of source of payment for childbirth. Reproductive health 13: 245-256.
- Sandall J, Tribe RM, Avery L, Mola G, Visser GH, et al. (2018) Short-term and long-term effects of caesarean section on the health of women and children. Lancet 392: 1349-1357.
- Keag OE, Norman JE, Stock SJ (2018) Long-term risks and benefits associated with cesarean delivery for mother, baby, and subsequent pregnancies: Systematic review and meta-analysis. PLoS Med 15: 1002494.
- Yu HY, Gumusoglu SB, Cantonwine DE, Carusi DA, Gurnani P, et al. (2023) Circulating microparticle proteins predict pregnancies complicated by placenta accreta spectrum. Sci Rep 12: 21922.
- Cahill AG, Beigi R, Heine RP, Silver RM, Wax JR (2018) Placenta Accreta Spectrum. Am J Obstet Gynecol 219: 2-16.
- Antoine C, Timor-Tritsch IE, Agoha C, Alexander J (2022) A new era in teaching: How advanced optical recording technology could change the postcesarean delivery complication conundrum. Am J Obstet Gynecol MFM 4: 100744.
- Antoine C, Young BK (2020) Cesarean section one hundred years 1920-2020: The Good, the Bad and the Ugly. J Perinat Med 49: 5-16.
- Pfannenstiel J (1897) On the advantages of a transverse cut of the fascia above the symphysis for gynecological laparotomies, and advice on surgical methods and indications. Samml Klin Vortr Gynakol 68: 1-22.
- Joel-Cohen S (1972) Abdominal and vaginal hysterectomy: new techniques based on time and motion studies. Lippincott, Pennsylvania, USA.
- Holmgren G, Sjöholm L, Stark M (1999) The Misgav Ladach method for cesarean section: Method description. Acta Obstet Gynecol Scand 78: 615-621.
- Stark M, Finkel AR (1994) Comparison between the Joel-Cohen and Pfannenstiel incisions in cesarean section. Eur J Obstet Gynecol Reprod Biol 53: 121-122.
- Stark M, Chavkin Y, Kupfersztain C, Guedj P, Finkel AR (1995) Evaluation of combinations of procedures in cesarean section. Int J Gynaecol Obstet 48: 273-276.
- Xavier P, Ayres-De-Campos D, Reynolds A, Guimaraes M, Costa-Santos C, et al. (2006) The modified misgav-ladach versus the pfannenstiel-kerr technique for cesarean section: A randomized trial. Obstetrical & gynecological survey 61: 10-12.
- Dodd JM, Anderson ER, Gates S, Grivell RM (2014) Surgical techniques for uterine incision and uterine closure at the time of caesarean section. Cochrane Database Syst Rev: CD004732.
- Temmerman M (2016) Caesarean section surgical techniques: All equally safe. Lancet 388: 8-9.
- Stark M (2019) Evidence-Based Cesarean Section for Universal Use in China: The “Stark (Misgav Ladach) Method”. Maternal-Fetal Medicine 1: 48-52.
- Dahlke JD, Mendez-Figueroa H, Maggio L, Sperling JD, Chauhan SP, et al. (2020) The Case for Standardizing Cesarean Delivery Technique: Seeing the Forest for the Trees. Obstet Gynecol 136: 972-980.
- Antoine C, Alexander JS, Yaghoubian YC, Harary JM (2022) Variations in uterine closure technique: An institutional survey of obstetricians and implications for patient counseling and prevention of adverse sequelae. J Perinat Med 50: 1045-1052.
- Harjee R, Khinda J, Bedaiwy MA (2021) Reproductive outcomes following surgical management for Isthmoceles: a systematic review. J Minim Invasive Gynecol 28: 1291-1302.
- Nieto-Calvache AJ, Palacios-Jaraquemada JM, Osanan G, Cortes-Charry R, Aryananda RA, et al. (2021) Lack of experience is a main cause of maternal death in placenta accreta spectrum patients. Acta Obstet Gynecol Scand 100: 1445-1453.
- Antoine C, Pimentel RN, Timor-Tritsch IE, Mittal K, Bennett TA, et al. (2021) Origin of a Post-Cesarean Delivery Niche: Diagnosis, Pathophysiologic Characteristics, and Video Documentation. J Ultrasound Med 40: 205-208.
- Antoine C, Meyer JA, Silverstein JS, Alexander J, Oh C, et al. (2022) The Impact of Uterine Incision Closure Techniques on Post-cesarean Delivery Niche Formation and Size: Sonohysterographic Examination of Nonpregnant Women. J Ultrasound Med 41: 1763-1771.
- Antoine C, Pimentel RN, Reece EA, Oh C (2021) Endometrium-free uterine closure technique and abnormal placental implantation in subsequent pregnancies. J Matern Fetal Neonatal Med 34: 2513-2521.
- Mogos MF, Salemi JL, Ashley M, Whiteman VE, Salihu HM (2016) Recent trends in placenta accreta in the United States and its impact on maternal-fetal morbidity and healthcare-associated costs, 1998-2011. J Matern Fetal Neonatal Med 29: 1077-1082.
- Babu K, Magon N (2012) Uterine closure in cesarean delivery: A new technique. N Am J Med Sci 4: 358-361.
- Moro F, Mavrelos D, Pateman K, Holland T, Hoo WL, et al. (2015) Prevalence of pelvic adhesions on ultrasound examination in women with a history of Cesarean section. Ultrasound Obstet Gynecol 45: 223-228.
- González-Quintero VH, Cruz-Pachano FE (2009) Preventing adhesions in obstetric and gynecologic surgical procedures. Rev Obstet Gynecol 2: 38-45.
Citation: Antoine C (2023) Pathophysiology of Long-Term Post-Cesarean Complications: Novel Insight from Tissue Magnification Video-Recording. J Reprod Med Gynecol Obstet 8: 127.
Copyright: © 2023 Clarel Antoine, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

