Pedicle Subtraction Osteotomy on a Patient with Severe Sagittal Imbalance Progression But Proportionate Gap Score Case Report and Lliterature Review
*Corresponding Author(s):
Silvia Suarez-MonsalveDepartment Of Neurosurgery Research Group, Medicine, Pontificia Universidad Javeriana, Bogota, Colombia
Tel:+571 3208320,
Email:silvia-suarez@javeriana.edu.co
Abstract
Purpose: To demonstrate the successful surgical management of a patient with Degenerative Disc Disease (DDD) who underwent multiple surgeries but continued to suffer from severe sagittal imbalance despite a proportioned GAP Score.
Methods: A case report was conducted on a patient diagnosed with a DDD that progressed to severely symptomatic positive sagittal imbalance but a proportionated GAP Score. Additionally, a literature review was conducted on indexed databases such as PubMed, Embase, and OVID, using MeSH terms such as “sagittal balance”, “GAP score” and “spinal column surgery”.
Results: Sagittal spine balance is crucial in evaluating patients with spinal deformities and determining the most appropriate surgical approach for each patient. The Global Alignment and Proportion Score (GAP) is a validated method for determining ideal spinopelvic parameters for patients undergoing spinal column surgery. This score is an individualized method of analyzing the sagittal plane based on pelvic incidence, effectively predicting mechanical complications of surgery for adult spinal deformity. Unlike the GAP score, the Sagittal Vertical Axis (SVA) is a reference in this method, and instead, it is replaced by the Global Tilt, which can evaluate spinal and pelvic alignment.
Conclusion: This case report describes a DDD patient and severe symptomatic positive sagittal imbalance. The patient's proportions were appropriate according to the GAP score, but the SVA was over 150 mm. A Pedicle Subtraction Osteotomy (PSO) at L3 was performed, resulting in lumbar hyperlordosis and correcting the SVA while significantly reducing the patient's symptoms.
Keywords
GAP score; Pedicle subtraction osteotomy; Sagittal balance; Spine surgery
Introduction
The spinal column is a bone structure tasked with protecting the spinal cord, maintaining an erect posture, and executing movements without pain. In the human species, it also allows bipedalism and march without any external support. The latter was achieved by developing compensatory spinal column curvatures on the sagittal plane which conditions sagittal balance with minimum energy consumption [1]. Pathological changes with these curvatures may cause sagittal disbalance which requires musculoskeletal secondary compensation forces to balance functionality and posture, which also represents greater energy expenditure leading to pain, functional limitations, and quality of life deterioration [2,3]. Sagittal balance connects variables that relate the spinal column with the pelvis and lower limbs, which are denominated as spinopelvic parameters. These correspond to measurable values on a sagittal X-ray with a patient standing and looking to the front. When encountered with pathologies that disrupt the sagittal balance, restoring these parameters to recover the biomechanical relation between these structures is necessary to avoid patient complications [4]. At present there is a tool called the Global Alignment and Proportion score (GAP), which permits analyzing current sagittal balance to make a surgical plan looking forward to ideal biomechanical values and outstanding clinical outcomes [5]. We present the case of an adult male with spinal column disc degenerative disease with prior surgery. The patient progresses to severe sagittal disbalance requiring multiple surgical interventions, finally leading to Pedicle Subtraction Osteotomy (PSO). Although this procedure generates lumbar hyperlordosis, the patient can recover and tolerate bipedalism and march without any external support, drastically improving its functionality and quality of life.
Case Report
First surgical intervention
A male patient in his sixties, with a prior history of grade I obesity, consulting for lumbosacral pain of two years radiating to both lower limbs and associated with paraesthesia and hypoesthesia. Neurological exam evidenced pain to lumbosacral paravertebral touch and pain to axial movements. Preserved strength and sensitivity without signs of radicular stretch or facet stress. Lumbosacral MRI evidenced multilevel degenerative discal disease L2-L3 and L3-L4 Pffirmann III, and L4-L5 and L5-S1 Pffirmann IV, associated with facet hypertrophy. Dynamic lumbosacral X-ray demonstrates diminished disc height for L2-L3 and L5-S1 (figure 1). Panoramic initial X-ray (March 2020) evidenced right convex 15-degree scoliosis with apex L4-L5. The patient underwent his first surgery via TLIF MIS L4-L5-S1 + T10 to S1 posterior simple instrumentation, correcting coronal disbalance without complications. Clinical follow-up documents pain persistence on the thoracolumbar region associated with lower limb paraesthesia. Post-op images show adequately placed arthrodesis material (figure 2).
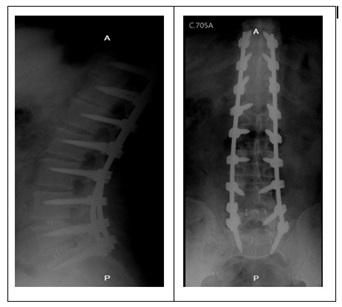 Figure 1: First post-op simple X-rays. Arthrodesis material adequately placed, pedicular screws fixation and intersomatic cages L4-L5 and L5-S1.
Figure 1: First post-op simple X-rays. Arthrodesis material adequately placed, pedicular screws fixation and intersomatic cages L4-L5 and L5-S1.
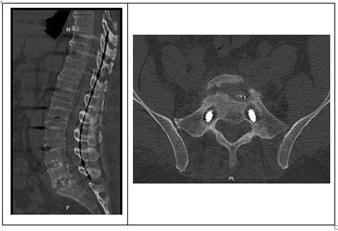 Figure 2: First Post-op CT: Intersomatic fusion mass without complete consolidation, sacroiliac joint vacuum in S1 instrumentation with left predominance.
Figure 2: First Post-op CT: Intersomatic fusion mass without complete consolidation, sacroiliac joint vacuum in S1 instrumentation with left predominance.
Second surgical intervention
On the fourth-month post-op, due to symptom persistence despite surgical management a CT scan was ordered as a complementary study, showing a lumbosacral spine with vast foraminal decompression, however, the CT also reported fusion mass without complete consolidation (figure 3). An L5-S1 pseudoarthrosis was considered an adjacent segment disease. A revision, osteotomy, and inter-somatic cage removal TLIF were performed to further insert a new OLIF MIS cage and T5 to S2 iliac extension instrumentation considering the extension of DDD and facet hypertrophic.
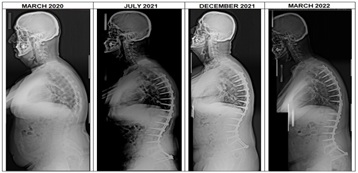 Figure 3: Panoramic radiographs in clinical follow-up.
Figure 3: Panoramic radiographs in clinical follow-up.
Forwarding two months, the pain was relinquished to 2/10 on the analog pain scale, with sensitive symptom resolution and no motor deficit. The patient received rehab physical therapy.
Third surgical intervention
On the fourth-month post-op of the last surgical intervention, the patient persists with lumbar and left glute mechanic pain predominantly when standing up and with sacroiliac compression pain. Concatenating with CT these findings suggest post fusion sacroiliitis. The suggested procedure was a bilateral L5-S1-S2 radio frequency percutaneous neuro-ablation technique (DREZ). Likewise, a T5 screw change and Ponte T10-T11-T12-L1 osteotomy with satellite bar connector implantation as reinforcement. The next clinical follow up the patient persists with axial pain and functional limitations. New CT showed L5-S1 pseudoarthrosis signs with L5-S1 intersomatic fusion, and transpedicular screws inserted normally without loosening up. However, as the patient continued having pain, a new panoramic X-ray was taken, and every image taken was used as a comparison and to measure spinopelvic parameters (figure 4). These parameters were labeled as proportional according to GAP score [6], apart from sagittal balance (parameter not included in the GAP score) which showed severe progression overthrowing the 150mm of positive disbalance (figure 4). Severe sagittal disbalance made progressive and significant changes in the patient’s posture, increasing his cervical lordosis to maintain eye gaze frontwards, inclining the pelvis backward, extending the hip, and flexing both knees while walking. This translated into an osteomuscular energy expenditure increase causing pain, fatigue, and medical absent leaves.
 Figure 4: Double bar system L3 PSO day one post op X-ray. A posterior wall reduction is appreciated and lumbar lordosis gains.
Figure 4: Double bar system L3 PSO day one post op X-ray. A posterior wall reduction is appreciated and lumbar lordosis gains.
Fourth Surgical Intervention
Knowing the severe sagittal disbalance and the patient’s adaptive changes, despite adequate spinopelvic proportion classification, a fourth surgical intervention was decided to improve sagittal balance even though this can compromise other parameters (table 1). An L3 PSO was performed (figure 5) with the goal of diminishing posterior vertebral wall height, and overcorrecting lumbar lordosis which reduces sagittal deformity (figure 6). Intra-operatory findings demonstrate chromium-cobalt bar rupture on the distal segment, connecting with the great mechanical effort the patient made, requiring T3 instrumental extension and double bar lumbosacral reinforcement (figure 7).
|
Spinopelvic parameters |
Initial |
POP 1st surgery |
POP 2nd surgery |
POP 3rd surgery |
POP Lastsurgery |
|
Pelvicincidence (PI) |
60º |
62º |
69º |
69º |
62.8º |
|
PelvicTilt (PT) |
14º |
20º |
24º |
22º |
23.3º |
|
SacralSlope (SS) |
49º |
47º |
49º |
47º |
42.4º |
|
Lumbar Lordosis L1-S1 |
59º |
65º |
70º |
60º |
72.8º |
|
Lumbar Lordosis L4-S1 |
40º |
46º |
53º |
42º |
31.3º |
|
Sagital vertical axis (SVA) |
112 mm |
113 mm |
11 mm |
165 mm |
72 mm |
|
Global Tilt (GT) |
17.5º |
26.2º |
31.5º |
30º |
30º |
|
Global Alignment and proportion (GAP) Score |
1 |
0 |
1 |
1 |
2 |
|
MISMATCH (LL-PI) |
-1 |
+2 |
+3 |
+9 |
+13.2 |
Table 1: Spinopelvic parameter comparisons while measuring on the follow up panoramic X-rays.
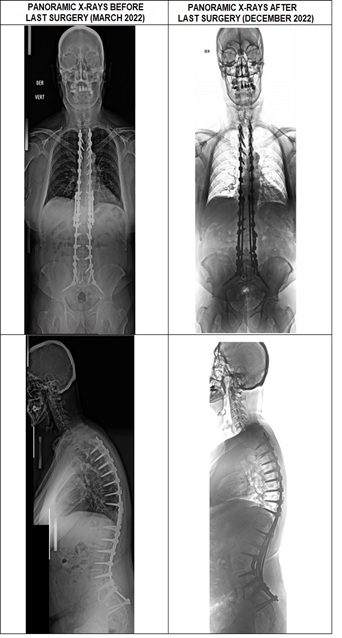 Figure 5: Coronal and Sagittal panoramic X-ray comparison from the last surgery.
Figure 5: Coronal and Sagittal panoramic X-ray comparison from the last surgery.
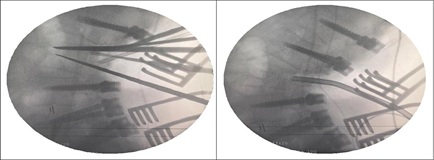 Figure 6: Intraoperative fluoroscopy X-rays. The left image shows osteotomes building wedges with the anterior vertex. The right image shows the wedge removed. An immediate lordosis gain is evidenced compared with previous bar implantation.
Figure 6: Intraoperative fluoroscopy X-rays. The left image shows osteotomes building wedges with the anterior vertex. The right image shows the wedge removed. An immediate lordosis gain is evidenced compared with previous bar implantation.
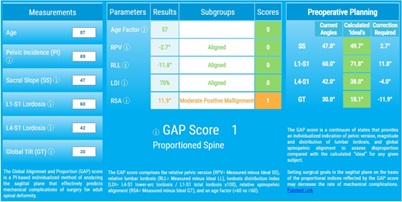 Figure 7: Patient GAP score before the last surgical procedure within proportions, calculated withhttp://www.gapcalculator.com/
Figure 7: Patient GAP score before the last surgical procedure within proportions, calculated withhttp://www.gapcalculator.com/
From that point onwards, the patient began to show consistent clinica improvement. His posture changed, andhe continued to experience a significant recovery in his quality of life, which has remained consistent even after a year.
Discussion
Bipedalism in Homo sapiens stands as an evolutionary feat, liberating upper limbs during movement. However, this exchange, though advantageous, decreases sagittal balance stability compared to other mammals, increasing susceptibility to spinal degenerative diseases [7,8]. Unlike most primates, humans developed cervical and lumbar lordosis to counter thoracic kyphosis, preserving a forward head posture [7,9]. Spinal balance predominantly relies on sagittal plane curvature over coronal curvature [5]. Multiple pathologies can disrupt this balance, necessitating a comprehensive understanding of normal sagittal balance and compensatory mechanisms for effective therapeutic strategies.
Evaluating spinal balance is dynamic, often done using static exams like X-rays. However, this approach has limitations as it reflects the patient's position during the exam, constraining interpretation. To overcome this, a holistic approach analyzing body postures (sitting, standing, walking), forward head posture, horizontal gaze position, lower extremity adjustments, and upper limb support needs consideration [10,11].
The Sagittal Vertical Axis (SVA), measuring the distance between a line through half of C7's vertebral body and one from the sacrum's poster inferior corner, is a critical parameter for evaluating quality of life [12]. It widens with aging, although position-related variations introduce bias (2.5). Increasing sagittal imbalance increases pain and functional limitations, warranting surgical intervention.
The Global Alignment and Proportion score (GAP score), assessing sagittal balance against patient Pelvic Incidence (PI), predicts post-op complications (p-value <0.001, CI 0.85-0.98) based on parameters like pelvic version, lumbar lordosis distribution, and spinopelvic alignment (5). A proportional balance yields a 6% complication rate, contrasting 47-95% for moderate to severe disproportion [5]. Anterior deviation increases complications, especially with pelvic anteversion and hyperlordosis. Nevertheless, the GAP score's predictive capacity for mechanical failure remains debated [13-15].
Our case had a calculated GAP score but a notably positive SVA, complicating bipedalism, walking, and causing mechanical issues. SVA, excluded from the GAP formula, demands individual analysis for surgery. It's vital to customize each case, considering SVA's variation and its linkage to quality of life [12]. Descriptive parameters serve as guides, not rigid rules, varying with age, sex, and race.
Aging and spinal deformities evoke compensatory musculoskeletal shifts to maintain sagittal balance, including lumbar lordosis, thoracic spine flattening, pelvic retroversion, and knee flexion [16]. These adaptations seek bipedal posture and horizontal gaze with minimal energy expenditure. Correcting lower limb alignment, exemplified in our case, becomes a key therapeutic goal for spinopelvic surgery planning, yielding successful results [17-25].
Conclusion
Sagittal spinal column balance is achieved by maintaining harmony within its architecture, preserving constitutional curvature ranges. This allows us to maintain bipedalism equilibrium with a low energy expenditure. When patients have an affected sagittal balance, knowing about compensatory mechanisms, parameters and global evaluation is fundamental to making therapeutic decisions and reducing mechanical complications in spinal deformity surgical procedures. However, it is important to highlight that, while spinopelvic parameters are valuable reference values, at times, the patient`s clinical presentation takes precedence over these measurements. Even when a patient is classified as “proportionate” or with a GAP of 1, the may continue to exhibit symptoms that lead to multiple surgeries. In some cases, hyperlordosis generations is resorted to in order to compensate for their sagittal balance and alleviate symptoms. This underscores the importance of addressing each case on an invidivualized basis, considering both spinipelvic parameters and the patient’s clinical experiences.
Ethical Considerations
This case corresponds to a patient with an age of majority, having all his cognitive qualities preserved. Who widely knows the nature, benefits, and risks of this research, as the academic interest of publishing his medical history. Informed consent procedures were undertaken according to the International Medical Ethics Committee´s directives.
Statements and Declarations
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
References
- Ames CP, Smith JS, Scheer JK, Bess S, Bederman SS, et al. (2012) Impact of Spinopelvic Alignment on Decision Making in Deformity Surgery in Adults: A Review. J Neurosurg Spine 16: 547-564.
- Totera JIC, Valenzuela JGF, Arancibia JAG, Contreras STP, Lalanne LB, et al. (2021) Sagittal Balance: From Theory to Clinical Practice. EFORT Open Rev 6: 1193-1202.
- Schwab F, Patel A, Ungar B, Farcy JP, Lafage V (2010) Adult Spinal Deformity-Postoperative Standing Imbalance: How Much Can You Tolerate? An Overview of Key Parameters in Assessing Alignment and Planning Corrective Surgery.Spine (Phila Pa 1976) 35: 2224-2231.
- Ohba T, Ebata S, Ikegami S, Oba H, Haro H (2020) Indications and Limitations of Minimally Invasive Lateral Lumbar Interbody Fusion without Osteotomy for Adult Spinal Deformity. Eur Spine J 29: 1362-1370.
- Yilgor C, Sogunmez N, Boissiere L, Yavuz Y, Obeid I, et al. (2017) Global Alignment and Proportion (GAP) Score: Development and Validation of a New Method of Analyzing Spinopelvic Alignment to Predict Mechanical Complications after Adult Spinal Deformity Surgery. J Bone Joint Surg Am 99:1661-1672.
- Yener U, Buell TJ, Burke RM, Ames CP, Yen CP, et al. (2021) Pedicle Subtraction Osteotomy. Revis Lumbar Spine Surg 10: 140-151.
- Le Huec JC, Thompson W, Mohsinaly Y, Barrey C, Faundez A (2019) Sagittal Balance of the Spine. Eur Spine J 28:1889-1905.
- Abelin-Genevois K (2021) Sagittal balance of the spine. Orthop Traumatol Surg Res 107: 102769.
- Yan YZ, Shao ZX, Pan XX, Chen SQ, Wu AM, et al. (2018) Acceptable Chin-Brow Vertical Angle for Neutral Position Radiography: Preliminary Analyses Based on Parameters of the Whole Sagittal Spine of an Asymptomatic Chinese Population. World Neurosurg 120: 488-496.
- Yilgor C, Pellise DLF (2016) Global Tilt: A Single Parameter Incorporating Spinal and Pelvic Sagittal Parameters and Least Affected By Patient Positioning. Eur Spine J 25: 3644-3649.
- Shah AA, Lemans JVc, Zavatsky J, Agarwal A, Kruyt MC, et al. (2019) Spinal Balance/Alignment-Clinical Relevance and Biomechanics. J Biomech Eng.
- Yu M, Zhao WK, Li M, Wang SB, Sun Y, et al. (2015) Analysis of Cervical and Global Spine Alignment Under Roussouly Sagittal Classification in Chinese Cervical Spondylotic Patients and Asymptomatic Subjects. Eur Spine J 24: 1265-1273.
- Le Huec JC, Hasegawa K (2016) Normative Values for the Spine Shape Parameters Using 3D Standing Analysis from a Database of 268 Asymptomatic Caucasian and Japanese Subjects. Eur Spine J 25: 3630-3637.
- Celestre PC, Dimar JR, Glassman SD (2018) Spinopelvic Parameters: Lumbar Lordosis, Pelvic Incidence, Pelvic Tilt, and Sacral Slope: What Does a Spine Surgeon Need to Know to Plan a Lumbar Deformity Correction? Neurosurg Clin N Am 29: 323-329.
- Barrey C, Jund J, Noseda O, Roussouly P (2007) Sagittal Balance of the Pelvis-Spine Complex and Lumbar Degenerative Diseases. A Comparative Study About 85 Cases. Eur Spine J 16: 1459-1467.
- Duval-Beaupere G, Schmidt C, Cosson P (1992) A Barycentremetic Study of the Sagittal Shape of Spine and Pelvis: The Conditions Required for an Economic Standing Position. Ann Biomed Eng 20: 451-462.
- Glassman S, Bridwell K, Berven S, Horton W, Schwab F (2004) The Impact of Positive Sagittal Balance in Adult Spinal Deformity. Spine (Phila Pa 1976) 30: 2024-2029.
- Roussouly P, Gollogly S, Berthonnaud E, Dimnet J (2005) Classification of the Normal Variation in the Sagittal Alignment of the Human Lumbar Spine and Pelvis in the Standing Position. Spine (Phila Pa 1976) 30: 346-353.
- Hiyama A, Katoh H, Sakai D, Watanabe M (2022) Analysis of Mechanical Failure Using the GAP Score After Surgery With Lateral and Posterior Fusion for Adult Spinal Deformity. Glob Spine J 13: 2488-2496.
- Jacobs E, van Royen BJ, van Kuijk SMJ, Merk JMR, Stadhouder A, et al. (2019) Prediction of Mechanical Complications in Adult Spinal Deformity Surgery-The GAP Score Versus the Schwab Classification. Spine J 19: 781-788.
- Kwan KYH, Lenke LG, Shaffrey CI, Carreon LY, Dahl BT, et al. (2021) Are Higher Global Alignment and Proportion Scores Associated With Increased Risks of Mechanical Complications After Adult Spinal Deformity Surgery? An External Validation.Clin Orthop Relat Res 479: 312-320.
- Ma H, Hu Z, Shi B, Liu Z, Zhu Z, et al. (2022) Global Alignment and Proportion (GAP) Score in Asymptomatic Individuals: Is it Universal? Spine J 22: 1566-1575.
- Hasegawa K, Dubousset JF (2022) Cone of Economy with the Chain of Balance-Historical Perspective and Proof of Concept. Spine Surg Relat Res 6: 337-349.
- Barrey C, Perrin G, Michel F, Vital JC, Obeid I (2014) Pedicle Subtraction Osteotomy in the Lumbar Spine?: Indications , Technical Aspects , Results and Complications. Eur J Orthop Surg Traumatol.
- Halim A, Kiester D, Lee Y-P (2017) Smith-Peterson and Pedicle Subtraction Osteotomies. Seminars in Spine Surgery 29: 91-99.
Citation: Suarez-Monsalve S, Sierra-Peña JA, Becerra JE, Perez JC (2023) Pedicle Subtraction Osteotomy on a Patient with Severe Sagittal Imbalance Progression But Proportionate Gap Score Case Report and Lliterature Review. Int J Case Rep Ther Stud 4: 024.
Copyright: © 2023 Silvia Suarez-Monsalve, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.