
Percutaneous Coronary Intervention in Older Patients with High-Risk Non-ST-Elevation Myocardial Infarction in Vietnam: An Observational Study
*Corresponding Author(s):
Tan Van NguyenDepartment Of Geriatric And Gerontology, University Of Medicine And Pharmacy, 217 Hong Bang, Ward 7, District 5, Ho Chi Minh City, Vietnam
Tel:+84 0903739273,
Email:nguyenvtan10@ump.edu.vn
Abstract
Objective: This study aims to describe the clinical characteristics of older patients with high-risk Non-St-Elevation Myocardial Infarction (NSTEMI) in Vietnam and to examine the impact of early Percutaneous Coronary Intervention (PCI) on adverse outcomes after 3 months.
Methods: In a prospective, observational, multicenter cohort study, between Sep 1, 2017 and Jan 31, 2018, we recruited patients aged 60 years or older with high or very high risk acute NSTEMI admitted to 2 hospitals in the South Region of Vietnam. Participants were followed up for 3 months. The primary outcome was defined as a composite of cardiovascular death or cardiovascular re-admission due to heart failure, myocardial re-infarction, or stroke. The secondary outcomes were all-cause mortality, cardiovascular death, recurrent myocardial infarction, stroke and cardiovascular re-admission.
Results: There were 301 participants, mean age 76, 43% female. Of these, 121 (40.2%) patients received early PCI. After a 3-month follow-up, the event rates of the primary composite outcome were 30% in the PCI group and 60% in the non-PCI group (adjusted hazard ratio HR 0.44, 95% CI 0.20-0.67, p<0.001). Secondary outcome events also favored early PCI including all-cause mortality (adjusted HR0.23, 95%CI 0.09-0.62,p=0.003), cardiovascular death (adjusted HR 0.17, 95%CI 0.04-0.78, p=0.02), recurrent myocardial infarction (adjusted HR, 0.46, 95%CI 0.29-0.71, p<0.001), stroke (adjusted HR, 0.29, 95%CI 0.11-0.74, p=0.01) and cardiovascular re-admission (adjusted HR, 0.50, 95%CI0.31-0.82, p=0.006).
Conclusion: In this study of older patients presenting with high risk NTEMI, early PCI was associated with reduced cardiovascular events after 3-month.
Keywords
Acute coronary syndrome; Elderly; High risk; Non-ST-elevation myocardial infarction; Optimal medical therapy; Percutaneous coronary intervention
INTRODUCTION
Clinical outcomes of acute Non-St-Elevation Myocardial Infarction (NSTEMI) has improved in recent years due to improvement of treatment strategies including Optimal Medical Therapy (OMT) and coronary revascularization. Percutaneous Coronary Intervention (PCI) has been proven to be a more effective method compared to conservative treatment in patients with NSTEMI [1,2]. However, the optimal treatment strategy in the older patients remains uncertain, especially in the older patients with high risk or very high risk NSTEMI. These patients are usually less likely to receive invasive treatment due to comorbidities and higher rate of complications [3]. They are also underrepresented in large randomized controlled acute coronary syndrome trials [1,2]. Registry data suggest that invasive treatment is associated with superior outcomes including mortality in elderly NSTEMI patients [3-5]. However, randomized trials addressing this group of patients have yielded mixed results [6-10]. While the definition for “older” or “elderly” is variable in the literature, patients aged 60 years or older is considered elderly in Vietnam and there is limited evidence on the impact of early PCI on high risk NSTEMI in this population. Therefore, the aim of this observational cohort study was to describe the clinical characteristics of older patients with high-risk NSTEMI in Vietnam and to examine the impact of early PCI on adverse outcomes after 3 months.
METHODS
Study design
This was a prospective, observational, multicenter cohort study. Between Sep 1, 2017 and Jan 31, 2018, patients admitted to two hospitals in Ho Chi Minh City, Vietnam were recruited. All participants were followed for 3 months.
Participants
The study enrolled consecutive patients aged 60 years or older with high or very high risk NSTEMI, according to the guideline from the European Society of Cardiology [1]. High-risk NSTEMI criteria include: GRACE score >140, dynamic ST or T wave changes, or rise and fall in cardiac troponin compatible with MI. Very-high risk NSTEMI criteria include: hemodynamic instability or shock, recurrent or ongoing chest pain refractory to medical treatment, life-threatening arrhythmias or cardiac arrest, mechanical complications of MI, acute heart failure, or recurrent dynamic ST-T wave changes [1]. Elevated troponin was defined as a value exceeding the 99th percentile of the upper limit of normal at the local laboratory at each participating site. Exclusion criteria were: declining to participate in the study, expected short life expectancy (
Outcomes
The primary clinical outcome was defined as a composite of cardiovascular death or cardiovascular re-admission including heart failure, myocardial re-infarction, or stroke after 3 months of follow-up. Myocardial re-infarction was defined as recurrence of ischemic symptoms after the initial MI with >20% increase in troponin T-hs from baseline or new ST elevation >1mm in two or more contiguous leads [11]. Stroke was defined as a new focal neurological deficit of vascular origin lasting more than 24 hours. Refractory angina and the need for urgent revascularization was defined as increasing angina pectoris symptoms despite OMT with or without Electrocardiogram (ECG) changes as judged by the cardiologists in the community hospitals. The secondary clinical outcomes were all-cause mortality, cardiovascular death, myocardial re-infarction, stroke, and cardiovascular re-admission.
Sample size considerations: We estimated our study sample size based on the After Eighty study [6], which found that the primary outcome occurred in 40.6% of patients assigned to the invasive group and 61.4% of patients assigned to the conservative group. Power analysis indicated that at least 99 participants would be needed in each group to detect the difference in the primary outcome (at the power of 80% and p=0.05).
Statistical analysis
Data are presented as mean (± standard deviation) for continuous data with a normal distribution or as median (25th, 75th percentile) for continuous data with a non-normal distribution or as number (percent) for categorical variables. Continuous data variables were compared using either the Student’s t test or the Kruskal - Wallis test, depending on whether the data followed a normal distribution. We compared categorical variables using the χ2 test or Fisher’s exact test when applicable. Cumulative event rates of primary and secondary clinical outcomes were estimated using the Kaplan - Meier method. The log - rank statistic was used to test for significant differences in event rates between treatment groups. Univariate and multivariate analyses were performed using Cox regression analysis to calculate hazard ratios between groups and to adjust for possible confounders including age, gender, comorbidities (smoking, hypertension, dyslipidemia, diabetes, chronic kidney disease, heart failure, prior stroke, atrial fibrillation, and cognitive dysfunction) and hemoglobin levels. The number of variables included in the model was based on the allowed degrees of freedom dependent on event rate. All significant tests were two-tailed and were considered statistically significant at p
Results
During the recruitment period, there were 1381 patients with acute myocardial infarction admitted to the study hospitals. Of these, 965 patients were diagnosed with NSTEMI. Among these 965 patients, 664 were excluded from this study (11 due to short life expectancy, 334 due to aged <60, 319 due to low/intermediate risk NTEMI). Finally, a total of 301 participants were included in this study. They had a mean age of 76 and 43% were female. The proportion of participants receiving PCI was 40.2%.
The baseline characteristics of the participants are summarized in table 1. Patients treated with PCI were younger (median 71 versus79 years, p< 0.001) compared to patients treated conservatively. Patients in the PCI group were less likely to have chronic kidney disease (12% versus 33%, p < 0.001), cognitive dysfunction (15% versus 41%, p < 0.001), dementia (10% versus 39%, p < 0.001), Killip class ≥ III (p <0.001), and had lower GRACE score (median 145 versus 150, p < 0.001). Also, patients treated with PCI had higher baseline left ventricular ejection fraction (mean 60% versus 54.7%, p < 0.001) and lower rate of heart failure (17% versus 42%, p <0.001) which are well-known strong prognostic factors of adverse outcomes in myocardial infarction. Patients underwent PCI had shorter length of hospital stays compared to those in OMT group (median 9 versus 13 days, p < 0.001).
|
Overall (n = 301) |
PCI+OMT group (n = 121) |
OMT group (n = 180) |
P value |
|
|
Age (years)* |
76 (67, 83) |
71 (65, 78) |
79 (69, 86) |
< 0.001 |
|
Sex Female Male |
129 (43) 172 (57) |
41 (34) 80 (66) |
88 (49) 92 (51) |
0.014 |
|
BMI (kg/m2) |
23.7 (3.4) |
23.5 (3.8) |
23.8 (3.2) |
0.332 |
|
Medical History Smoking Hypertension Dyslipidemia Type 2 Diabetes Chronic Kidney Disease Hemodialysis Prior MI Heart Failure Prior Stroke Atrial Fibrillation Cognitive Dysfunction Dementia |
176 (58) 281 (93) 209 (69) 124 (41) 73 (24) 21 (7) 51 (17) 96 (32) 50 (17) 28 (9) 91 (30) 82 (27) |
79 (65) 111 (92) 90 (74) 52 (43) 14 (12) 7 (6) 16 (13) 21 (17) 15 (12) 5 (4) 18 (15) 12 (10) |
97 (54) 170 (94) 119 (66) 72 (40) 59 (33) 14 (8) 35 (19) 75 (42) 35 (19) 23 (13) 73 (41) 70 (39) |
0.065 0.491 0.162 0.693 < 0.001 0.664 0.21 < 0.001 0.146 0.02 < 0.001 < 0.001 |
|
Ejection Fraction (%) |
56.8 (11) |
60 (8.9) |
54.7 (11.8) |
< 0.001 |
|
Killip Class I II III IV |
74 (25) 155 (51) 56 (19) 16 (5) |
37 (31) 69 (57) 7 (6) 8 (7) |
37 (21) 86 (48) 49 (27) 8 (4) |
< 0.001 |
|
Laboratory Tests at Admission CKMB (U/L)* Troponin T-hs (pg/mL)* SGOT (U/L)* SGPT (U/L)* Hemoglobin (g/dL)* Platelet (K/mm3) WBC (K/mm3)* Urea (mmol/L)* Creatinine (µmol/L)* eGFR (mL/min/1.73 m2) Total Cholesterol (mg/dL) Triglyceride (mg/dL) HDL-C (mg/dL) LDL-C (mg/dL) |
56 (45, 73) 457 (234, 1221) 56 (45, 67) 45 (34, 54) 12.7 (10.4, 14) 265.6 (86.1) 6.3 (5.7, 11) 6.3 (5.5, 11) 105 (85, 126) 49.4 (23.1) 212.7 (42.5) 194.9 (53.1) 38.7 (7.7) 108.3 (34.8) |
56 (45, 78) 441 (228, 1225) 55 (45, 67) 45 (35, 55) 13.5 (11.9, 14.2) 276 (87.7) 6.2 (5.6, 7.8) 6 (5.3, 8) 98 (87, 120) 59 (23) 220.4 (38.7) 203.7 (53.1) 38.7 (7.7) 116 (34.8) |
56 (45, 68) 497 (234.75, 1186) 56 (45, 67) 43 (34, 51) 12 (9.8, 13.5) 258.7 (84.5) 6.6 (5.7, 13.8) 7.1 (5.6, 12) 109.5 (81.8, 137.3) 42.9 (20.9) 205 (42.5) 186 (62) 38.7 (7.7) 104.4 (34.8) |
0.197 0.743 0.935 0.04 < 0.001 0.157 < 0.001 < 0.001 0.124 < 0.001 < 0.001 0.001 0.128 0.003 |
|
ECG at Admission Sinus Tachycardia Sinus Bradycardia Bundle Branch Block Atrioventricular Block Atrial Flutter/Fibrillation Ventricular Tachycardia/Fibrillation |
79 (26) 10 (3) 19 (6) 14 (5) 29 (10)
13 (4) |
20 (17) 4 (3) 8 (7) 7 (6) 7 (6)
6 (5) |
59 (33) 6 (3) 11 (6) 7 (4) 22 (12)
7 (4) |
0.003 1 1 0.626 0.098
0.874 |
|
GRACE Score* |
150 (145, 158) |
145 (145, 152) |
150 (145, 160) |
< 0.001 |
|
Days in Hospital* |
12 (8, 14) |
9 (8, 12) |
13 (11, 15) |
< 0.001 |
|
Coronary Angiographic Lesions LMCA LAD LCX RCA Three Vessel Disease |
24 (20) 108 (89) 84 (69) 84 (69) 63 (52) |
|
||
Table 1: Baseline characteristics of the patients.
Data are displayed in n (%) for categorical variables, mean (standard deviation, SD) for continuous variables with normal distribution and median (25th, 75th percentile) for continuous variables with non-normal distribution. BMI=Body Mass Index. CKMB=Creatine Kinase Myocardial Band. ECG=Electrocardiogram. eGFR=Estimated Glomerular Filtration Rate. HDL-C=High Density Lipoprotein Cholesterol. LDL-C=Low Density Lipoprotein Cholesterol. MI=Myocardial Infarction. OMT=Optimal Medical Therapy. PCI=Percutaneous Coronary Intervention. SGOT=Serum Glutamic Oxaloacetic Transaminase. SGPT=Serum Glutamic Pyruvic Transaminase. Troponin T-hs=high sensitive Troponin T. WBC=White Blood Cell. *continuous variables with non-normal distribution. LAD= Left Anterior Descending, LCX=Left Circumflex, RCA= Right Coronary Artery
The median follow-up time was 90 days. The primary composite clinical outcome of cardiovascular death or cardiovascular re-admission due to heart failure, myocardial re-infarction, stroke occurred in 36 of 121 (30%) patients in the PCI group and in 108 of 180 (60%) patients in the OMT group. Kaplan-Meier analysis showed that there was a significant difference in cumulative composite outcome between the PCI and OMT groups (mean freedom time of 66 [95% CI 62 to 71 days] versus 80 [05% CI 69 to 75] days; log rank p < 0.001) (Figure 1). Cox regression analysis showed that even after controlling for comorbidities and other factors patients who underwent PCI still had superior primary outcome than the OMT group (Hazard Ratio (HR) 0.44 95% CI 0.20 to 0.67], p < 0.001) in regard to primary outcome (Table 2).
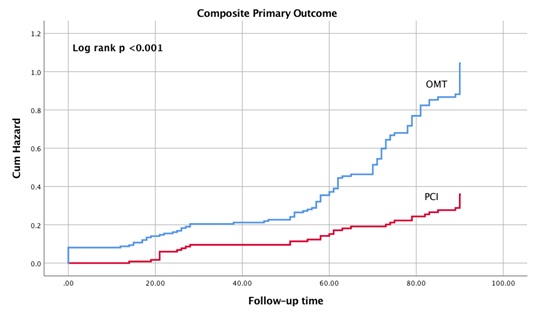 Figure 1: Kaplan-Meier Analysis of cumulative composite primary outcome.
Figure 1: Kaplan-Meier Analysis of cumulative composite primary outcome.
OMT=Optimal Medical Therapy. PCI=Percutaneous Coronary Intervention. The primary clinical outcome was defined as a composite of cardiovascular death or cardiovascular re-admission including heart failure, myocardial re-infarction, or stroke.
|
|
PCI+OMT N=121 |
OMT N=180 |
Unadjusted Hazard Ratio |
Unadjusted P value |
Adjusted Hazard Ratio |
Adjusted P Value |
|
Primary outcome |
36 (30) |
108 (60) |
0.348 (0.238-0.508) |
<0.001 |
0.437 (0.288-0.662) |
<0.001 |
|
All cause mortality |
5 (4) |
48 (27) |
0.130 (0.052-0.328) |
<0.001 |
0.232 (0.087-0.618) |
0.003 |
|
CV death |
2 (1.7) |
26 (14) |
0.099 (0.024-0.419) |
0.002 |
0.170 (0.037-0.775) |
0.022 |
|
Myocardial re-infarction |
33 (27) |
92 (51) |
0.367 (0.246-0.548) |
<0.001 |
0.455 (0.293-0.706) |
<0.001 |
|
Stroke |
6 (5) |
25 (14) |
0.269 (0.110-0.657) |
0.001 |
0.285 (0.110-0.739) |
0.010 |
|
Readmission |
29 (24) |
66 (43) |
0.454 (0.293-0.704) |
<0.001 |
0.505 (0.312-0.819) |
0.006 |
Table 2: Adjusted hazard ratio of PCI Plus OMT versus OMT in primary and secondary outcomes.
Data are displayed in n (%). OMT=Optimal Medical Therapy. CV = Cardiovascular. PCI=Percutaneous Coronary Intervention. The primary clinical outcome was defined as a composite of cardiovascular death or cardiovascular re-admission including heart failure, myocardial re-infarction, or stroke. The variables used in the multivariate analysis included: age, gender, smoking, hypertension, dyslipidemia, diabetes, chronic kidney disease, heart failure, prior stroke, atrial fibrillation, cognitive dysfunction and hemoglobin.
All five of the secondary outcomes also favored the PCI group including all-cause mortality (4% versus 27%, adjusted HR 0.23; 95% CI, 0.09 to 0.62; p = 0.003), cardiovascular death (1.7% versus 14%, adjusted HR 0.17; 95% CI 0.04-0.78; p=0.02),myocardial re-infarction (27% versus 51%, adjusted HR, 0.46; 95% CI, 0.29 to 0.71; p < 0.001), stroke (5% versus 14%, adjusted HR, 0.29; 95% CI, 0.11 to 0.74; p = 0.01) and cardiovascular re-admission (24% versus 43%, adjusted HR, 0.50; 95% CI, 0.31 to 0.82; p = 0.006) (Figures 2A-2E) (Table 2).
Figure 2A:
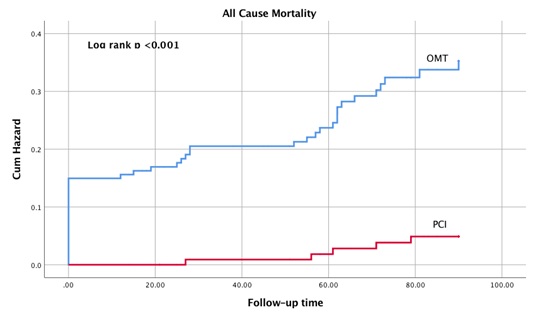 Figure 2B:
Figure 2B:
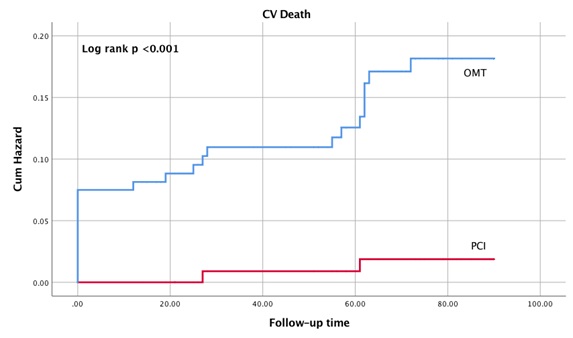 Figure 2C:
Figure 2C:
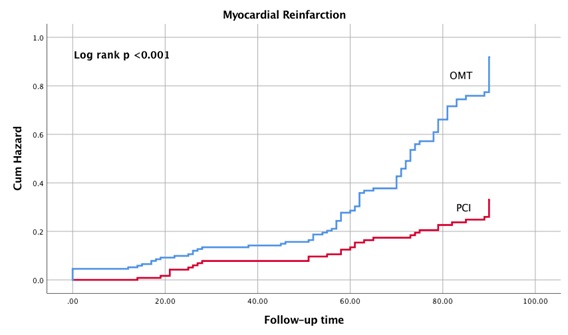 Figure 2D:
Figure 2D:
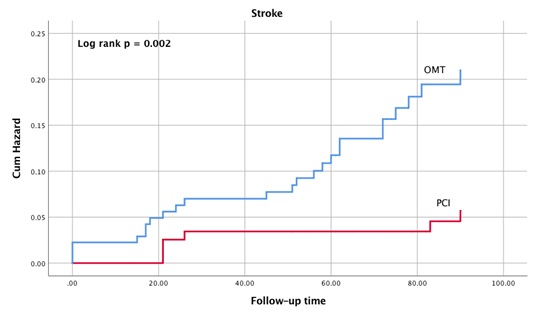 Figure 2E:
Figure 2E:
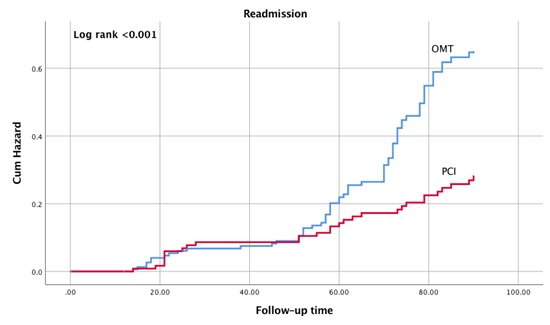
Figures 2A-2E: Kaplan-Meier Analysis of Cumulative Secondary Outcomes.
OMT = Optimal Medical Therapy. PCI=Percutaneous Coronary Intervention. Follow up time in days.
DISCUSSION
Older patients with Acute Coronary Syndrome (ACS) are a heterogeneous population with variable degree of frailty and differences in physiological ageing, comorbidity, functional status, and social aspects [12]. They are underrepresented in large clinical trials, and practice guidelines are often based on extrapolation of data from a substantially younger population [2]. Consequently, the optimal management of NSTEMI in the older patients, especially when they are high risk or very high risk is not clear. While the age cutoff for the “older” or “elderly” is variable in the literature ranging from 60 - 75 year old, we chose the lower limit since this is the local practice and reflects the significantly lower life expectancy in our population compared to developed nations [13,14].
Larger data sample from registries and large retrospective studies tend to favor an early invasive strategy. In patients aged 80 years or older with NSTEMI or unstable angina, invasive strategy was associated with a reduction in major adverse endpoints (a composite of myocardial infarction, stroke, death, bleeding complications and length of hospital stay) in the 2003–2010 Nationwide Inpatient Sample database and the GRACE registry [3,4]. In another large retrospective database analysis, invasive strategy was associated with lower mortality even in patients over 90 year old, although the bleeding risk was higher [5]. There were three major randomized controlled trials evaluating the benefit of PCI versus OMT in elderly patients with NSTEMI or unstable angina with inconsistent results. The Italian Elderly ACS trial found no significant difference in death, myocardial infarction or severe bleeding between PCI versus OMT alone in 313 elderly patients aged ≥75 years with NSTEMI or unstable angina, although, a subgroup analysis showed a significant benefit from invasive treatment in patients with elevated troponin levels [8]. The comorbilidades en el Síndrome Coronario Agudo (MOSCA) study found no significant difference between invasive versus conservative treatment in comorbid elderly patients aged ≥70 years with NSTEMI [7]. The After Eighty study provided the best evidence in favor of an invasive strategy in 457 clinically stable elderly patients aged ≥80 years with NSTEMI or unstable angina [6]. The primary outcome occurred in 93 (40.6%) of 229 patients assigned to the invasive group and 140 (61.4%) of 228 patients assigned to the conservative group (HR, 0.53; 95% CI 0.41 - 0.69; p = 0.0001).
Limitations from these studies are that they are small in number and the largest study (After Eighty) enrolled only ~10% of the patients screened making these results less generalizable [15]. The SENIOR-RITA trial is currently enrolling patients (expected to be 2300) with NSTEMI age ≥75 and randomizing them to either invasive or conservative treatment strategy which will add significantly to current knowledge (NCT03052036). The results of this study adds to the current body of evidence that an early PCI strategy compared to OMT is associated with reduction in major adverse events in older patients presenting with high or very high risk NSTEMI. It also highlights that these patients have very high event rates consistent with other reports of outcomes after acute coronary syndrome in low-income countries and thus would derive more benefits from aggressive therapies [16,17]. In relatively resource-limited communities such as our practice, the considerable benefits of early PCI demonstrated in this study suggest that investing in the current therapy may have high impact to public health.
A major limitation of this study is that this is an observational study which can lead to selection bias and the results may be influenced by potential confounders. A multivariable Cox proportional regression method was used to account for the influence of the potential confounders. Ideally, a large randomized controlled trial would provide more definitive answer to the optimal treatment strategy in this group of patient. However, this real world cohort study gives evidence that invasive streategy is a reasonable approach for elderly patients presenting with high or very high risk NSTEMI.
CONCLUSION
Early PCI plus OMT is associated with superior clinical outcomes compared to OMT alone at 3-month in older patients with high or very high risk acute NSTEMI.
DISCLOSURES
The authors have no relevant disclosures.
REFERENCES
- Roffi M, Patrono C, Collet JP, Mueller C, Valgimigli M, et al. (2016) 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J 37: 267-315.
- Fox KAA, Clayton TC, Damman P, Pocock SJ, de Winter RJ, et al. (2010) for the FIR Collaboration. Long-term outcome of a routine versus selective invasive strategy in patients with non-ST-segment elevation acute coronary syndrome a meta-analysis of individual patient data. J Am Coll Cardiol 55: 2435-2445.
- Devlin G, Gore JM, Elliott J, Wijesinghe N, Eagle KA, et al. (2008) Management and 6-month outcomes in elderly and very elderly patients with high-risk non-ST-elevation acute coronary syndromes: The Global Registry of Acute Coronary Events. Eur Heart J 29: 1275-1282.
- Kolte D, Khera S, Palaniswamy C, Mujib M, Fonarow GC, et al. (2013) Early invasive versus initial conservative treatment strategies in octogenarians with UA/NSTEMI. Am J Med 126: 1076-1083.
- Couture EL, Farand P, Nguyen M, Allard C, Wells GA, et al. (2018) Impact of an invasive strategy in the elderly hospitalized with acute coronary syndrome with emphasis on the nonagenarians. Catheter Cardiovasc Interv 92: 441-448.
- Tegn N, Abdelnoor M, Aaberge L, Endresen K, Smith P, et al. (2016) Invasive versus conservative strategy in patients aged 80 years or older with non-ST-elevation myocardial infarction or unstable angina pectoris (After Eighty study): An open-label randomised controlled trial. Lancet 387: 1057-1065.
- Sanchis J, Núñez E, Barrabés JA, Marín F, Consuegra-Sánchez L, et al. (2016) Randomized comparison between the invasive and conservative strategies in comorbid elderly patients with non-ST elevation myocardial infarction. Eur J Intern Med 35: 89-94.
- Savonitto S, Cavallini C, Petronio AS, Murena E, Antonicelli R, et al. (2012) Early aggressive versus initially conservative treatment in elderly patients with non-ST-segment elevation acute coronary syndrome: A randomized controlled trial. JACC Cardiovasc Interv 5: 906-916.
- Alexander KP, Newby LK, Cannon CP, Armstrong PW, Gibler WB, et al. (2007) Acute coronary care in the elderly, part I: Non-ST-segment-elevation acute coronary syndromes: A scientific statement for healthcare professionals from the American Heart Association Council on Clinical Cardiology: In collaboration with the Society of Geriatric Cardiology. Circulation 115: 2549-2569.
- Damman P, Clayton T, Wallentin L, Lagerqvist B, Fox KA, et al. (2012) Effects of age on long-term outcomes after a routine invasive or selective invasive strategy in patients presenting with non-ST segment elevation acute coronary syndromes: A collaborative analysis of individual data from the FRISC II - ICTUS - RITA-3 (FIR) trials. Heart 98: 207-213.
- Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, et al. (2018) Fourth Universal Definition of Myocardial Infarction (2018). J Am Coll Cardiol 72: 2231-2264.
- Madhavan MV, Gersh BJ, Alexander KP, Granger CB, Stone GW (2018) Coronary Artery Disease in Patients ≥80 Years of Age. J Am Coll Cardiol 71: 2015-2040.
- De Rosa R, Piscione F, Galasso G, De Servi S, Savonitto S (2019) Antiplatelet therapy in very elderly and comorbid patients with acute coronary syndromes. J Geriatr Cardiol 16: 103-113.
- https://data.worldbank.org/indicator/SP.DYN.LE00.IN?locations=VN
- Alexander KP (2017) Putting the Acute Coronary Syndrome in Context After 80 Years of Age. Circulation 135: 5-6.
- Qanitha A, Uiterwaal CSPM, Henriques JPS, Mappangara I, Idris I, et al. (2018) Predictors of medium-term mortality in patients hospitalised with coronary artery disease in a resource-limited South-East Asian setting. Open Heart 5: 000801.
- Yusuf S, Rangarajan S, Teo K, Islam S, Li W, et al. (2014) Cardiovascular risk and events in 17 low-, middle-, and high-income countries. N Engl J Med 371: 818-827.
Citation: Nguyen TV, Paul TK, Nguyen QT, Pham MHT, Co M, et al. (2020) Percutaneous Coronary Intervention in Older Patients with High-Risk Non-ST-Elevation Myocardial Infarction in Vietnam: An Observational Study. J Gerontol Geriatr Med 6: 063.
Copyright: © 2020 Tan Van Nguyen, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

