Physician Delay for Delayed Diagnosis of Acute Lymphoblastic Leukemia among Children in a Tertiary Care Hospital
*Corresponding Author(s):
Yasmin TTaslimaYasmin, Associate Professor (Microbiology), President Abdul Hamid Medical College, Kishorganj, Bangladesh
Tel:+880 01713 377003,
Email:taslimasanta@yahoo.com
Abstract
Background: Early diagnosis of cancer gives an opportunity for early treatment which is very important. Unfortunately, late presentation and delayed diagnosis of childhood cancers remain a problem in developing countries including Bangladesh. Few studies on delayed diagnosis of childhood cancers have been conducted in Bangladesh.
Objectives: To evaluate the factors behind physician delay in the diagnosis of acute lymphoblastic leukemia among children in a tertiary care hospital in Bangladesh.
Materials and methods: This was a descriptive cross sectional study carried out in the department of pediatrics, Mymensingh Medical College Hospital, Mymensingh, from April 2013 to September 2013. Information was obtained from hospital records of children diagnosed as acute leukemia Information included socio-demographic variables, duration of illness at diagnosis and other health seeking activities.
Results: Seventy children (44 males, 26 females) were included where the most common age group was 5-10 years which was 37 (52.9%). According to the initial clinical presentation, anemia mimic jaundice was 46 (65.7%), fever 69 (98.6%) and acute leukemia or pallor 2 (2.9%). First visit was taken from medical officer in 43 (61.4%). Median lag time was 60 days.
Conclusion: Lag time was longer than developed countries. Factors contributing to delayed diagnosis included delayed referral, seeking health care from alternate sources. First visit by a specialist physician can reduce the delay.
Keywords
Acute lymphoblastic leukemia; Physician delay.
INTRODUCTION
Acute leukemia is a malignant transformation of a clone of cells from lymphoid and myeloid progenitor cells. The majority of cases are of B-cell origin, but it can also arise from T-cell precursors [1]. Acute Lymphoblastic Leukemia (ALL) represents (80%) of all leukemias in children [2]. In developed countries, the age distribution of ALL shows a major peak at pre-school age (between 1-5 years) with a slow decline toward adolescence [3]. Symptoms includes fatigue, dizziness and palpitation, severe and unusual bone and joint pain, recurrent and severe infections (oral, throat, skin, perianal), fever without obvious infection (but infection should be assumed), left upper quadrant fullness and early satiety due to splenomegaly (10-20%), dyspnea, headache, irritability or altered mental status and neck rigidity, hemorrhagic or thrombotic complications due to thrombocytopenia or Disseminated Intravascular Coagulopathy (DIC) - for example, frequent nosebleeds, spontaneous bruising [1,4]. Diagnosis of ALL begins with a medical history, physical examination, complete blood count, and blood smears [5]. A bone marrow biopsy is conclusive proof of Leukemia [2].
Early diagnosis of cancer is a fundamental goal in pediatriconcology because it gives an opportunity for early treatment. Consequently, prognosis may occur and a cure can be attained with or without minimal side or late effects [6]. Many researchers carried out studies to find out the time to diagnose a variety of childhood cancers and the factors associated with delayed diagnosis in many developed and under developed countries. Some researchers have focused on the time between a patient's first symptom and the diagnosis of cancer. This time period, called diagnostic delay has also been designated as ‘time to diagnosis’, ‘lag time’ or ‘wait time’ by different authors [6]. Others have made a distinction between patient and physician delays [7]. The patient delay was defined as the length of time between the onset of signs and symptoms and the patient's first visit to the health care system, whereas the length of delay between the first health care visit and the diagnosis was designated as physician delay. Definition of physician delay may however not be strictly applicable in our country for a variety of social, cultural and official reasons. Factors contributing to delayed diagnosis included delayed referral by doctors, seeking health care from alternate sources, financial constraints, low educational level of parents [8-10]. More than (12%) of cancer cases are initially misdiagnosed. This often leads to seriously delayed diagnosis of cancer, which can sometimes causes treatable cancers to become harder to treat or completely untreatable. This may lead to serious complications, disfigurement and wrongful death.
So far no known published studies were conducted in Bangladesh regarding the factors influencing time lag between first appearances of symptoms to the final diagnosis of childhood ALL. From this point of view this study was conducted to find out the time lag between first appearance of symptoms to the final diagnosis of childhood acute leukemia in a tertiary care hospital. The result of the study may help taking proper interventions at hospital and community level, improving awareness among parents about symptoms of ALL, early referral, early diagnosis, proper treatment and also increasing survival rate and better care.
MATERIALS AND METHODS
This was a descriptive cross-sectional study conducted over a period of six months from April to September 2013 in Mymensingh Medical College Hospital, Mymensingh. Children of both sex admitted in the inpatient department of pediatrics were enrolled. Inclusion criteria were age bellow 18 years and diagnosed case of acute leukemia Exclusion criteria were children above 18 years, childhood cancer other than leukemia and sever anemia other than acute leukemia.Sampling technique was non probability purposive sampling. Data related to demography of patients, their socio-economic status, first appearing symptoms, first visit by health personal, other health seeking activities, etc. were obtained from hospital records and documented on predesigned data sheet. Data were analyzed by using computer based programmed excel and Statistical Package for Social Science (SPSS) version 25.0.
RESULTS
A total 70 children were enrolled as study population, among them male& female were 44 (62.9%) and 26 (37.1%) respectively. Most common age group was 5-10 years 37 (52.9%) [Table-I]. According to the initial clinical presentation, anemia mimic jaundice were 46 (65.7%), fever 69 (98.6%) and acute leukemia or pallor 2 (2.9%) [Figure-I]. Suspicion of leukemia was committed at primary set up in 69 (98.6%) [Table-II]. First visit by consultant, medical officer, medical assistant and none were 1 (1.4%), 43 (61.4%), 21 (30%) and 5 (7.1%) respectively prior treatment [Table-III]. Rheumatism was another symptom which was confused with the symptoms of ALL in 15 (21.4%) [Figure-II]. Total median diagnostic delay was 60 days. Median age is 7.00 Average age is 6.76.
|
Age |
Frequency |
Male |
Female |
|
<5 |
25 (35.7%) |
44 (62.9%) |
26 (37.1%) |
|
5-10 |
37 (52.9%) |
||
|
>10 |
8 (11.4%) |
||
|
Total |
70 (100%) |
Table I: Age and sex distribution of the studied children.
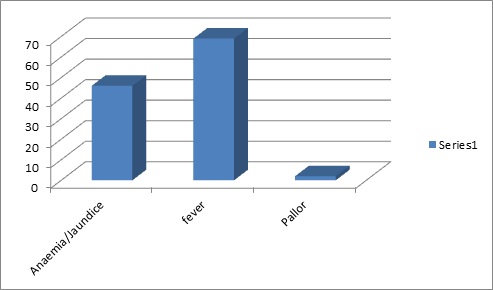 Figure I: Frequency of symptom at initial period of ALL.
Figure I: Frequency of symptom at initial period of ALL.
Figure I shows patients came at initial period with the first symptom anemia mimic jaundice were 46 (65.7%), fever 69 (98.6%) and ALL or pallor 2(2.9%).
|
Suspicion of leukemia |
Frequency |
|
Late |
1 (1.4%) |
|
Omitted |
69 (98.6%) |
|
Total |
70 (100%) |
Table II: Suspicion of leukemia at primary set up.
Table II shows at primary set up leukemia suspicion was only 1 (1.4%).
|
Health care professional |
Frequency |
Percentages |
|
Medical officer |
43 |
61.4 |
|
Medical assistant |
21 |
30 |
|
None |
5 |
7.1 |
|
Consultant |
1 |
1.4 |
|
Total |
70 |
100 |
Table III: Pattern of visit by health care professionalprior treatment.
Table III shows that the highest percentage of patients were initially visited by medical officer 43(61.4%).
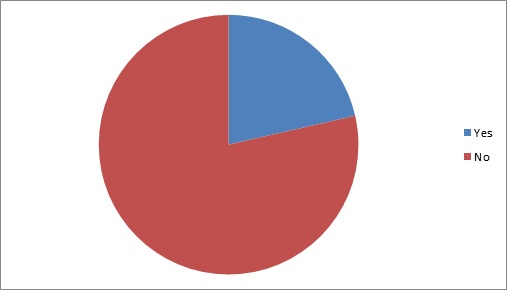 Figure II: ALL diagnosis confused with rheumatism.
Figure II: ALL diagnosis confused with rheumatism.
Figure II shows rheumatism was another symptoms which was confused with the symptoms of ALL 15(21.4%).
DISCUSSION
Literature providing adequate assessment of the survival variability by age at diagnosis is scarce. In developed countries, the age distribution of ALL shows a major peak at pre-school age (between 1-5 years) with a low decline toward adolescence [11]. This contrast to the typical age distribution in less developed countries with no pre-school peak [12]. In our study median age for ALL was 7 years, whereas average age was 6.76 (Table- I). Jubayar and his colleague found maximum age group was 1–4, which was (82%) likely to die compared to children diagnosed in infancy [13]. Hjalgrim et al. found in statistical analyzed data collected over 20 yrs (January’1 1982 andDecember’ 31, 2001) that 1595 girls and 1859 boys were diagnosed as ALL [14]. Other study done by James BO and his colleagues revealed that there were 40 males and 24 females suffering from ALL [15]. In our study we found 44 male and 26 female, which was similar with other studies (Table I). Another study done by Mehta V and his colleagues found that tumors were more common among male patients [16] whereas Amar Ali et al. found that there was no relationship with gender, age.
Common symptoms at the time of presentation of ALL include anemia, fever, pallor, bone pain, joint pain, which is overlapped by rheumatism. Such symptoms are confusing for physician, which may lead to delay diagnosis and treatment [17]. Early diagnosis is fundamental for cancer management because it allows rapid treatment. Symptoms of ALL are so general, many other diseases with similar symptoms, which must be carefully excluded to reduce time for delayed diagnosis [16]. For this reason specialist knowledge is required for physicians. Usually symptoms are not specific to ALL, because lack of normal and healthy blood cells as they are crowded out by malignant and immature leukocytes. In our study we have found that patients came with anemia mimic jaundice in 46 (65.7%), fever 69 (98.6%), pallor 2 (2.9%). Zombori L and others studied both leukemia and lymphoma- two third of both group of patients had other general symptoms like fever, fatigue. Twenty four percent of all children were previously evaluated by an orthopedist prior to diagnosis, which correlates with our study [18]. Stephen P and his colleagues found that symptoms of ALL include bruising or bleeding due to thrombocytopenia, pallor, fatigue from anemia and infection caused by neutropenia [19].
In childhood ALL, non-hematological manifestations involving the musculoskeletal system can also be encountered. These manifestations may cause a delay in the diagnosis. Öztürkmen in his case report showed that a six-year-old boy who developed bone pain and long bone fracture and was diagnosed as ALL after a considerable delay [20]. Falcini found out of 296 eligible patients, 179 (60%) had no bone pain, 65 (22%) had some bone pain and 52 (18%) had prominent bone pain [21]. In our study we have found similar relationship with delay in diagnosis in ALL confused with 15 (21.7%). Lins et al. found significant relationship between delayed diagnosis and joint pain as symptom [22].
Another important feature is suspicion of leukemia at primary set up is very important. But this suspicion is only done by expert physician either medical officer or consultant. In this study this suspicion was omitted in 69 (98.6%).
There may be delay when patient came to medical assistant or medical officers who are not specialist about ALL. In our study, before the patient reach to tertiary care hospital, they came to consultant (child specialist) in only 1 (1.4%). Compared the first visit by pediatrician and emergency room, there were lower risk of physician delay in case of pediatrician visit, described by Dang-tan [23].
Some studies had shown that median total diagnostic delay was caused by patient and physician delay. In our study median diagnostic delay was 60 days which was higher than Lins study [22]. Abdelkhalek said that misdiagnoses were initially recorded in (39%) patients, where 47 days caused by patients and parents [24]. Stefen DC and Siemonsma F found in their study that physician delay was 20 days and patient delay was 5 days [17]. Brown BJ and his colleagues found median lag time was shortest in ALL than other childhood tumor [15]. More than (12%) cancer cases are initially misdiagnosed. Evans et al found median diagnostic time was 3 weeks, patient diagnostic delay was (40.0%) and health associated delay (46.7%) [25].
CONCLUSION
In conclusion, this often leads to seriously delayed diagnosis of cancer, which can sometimes cause treatable cancers to become harder to treat or completely untreatable. This may lead to serious complications, disfigurement and wrongful death. So, this study was conducted to evaluate the causes of delayed diagnosis of ALL. Delayed diagnosis of cancer requires a sophisticated team of legal professionals who have experience working closely with medical specialists.
REFERENCES
- Roman E, Simpson J, Ansell P, Kinsey S, Mitchell CD, et al. (2007) Childhood acute lymphoblastic leukemia and infections in the first year of life:a report from the United Kingdom childhood cancer study. Am J Epideml 165: 496-504.
- Redaelli A, Laskin BL, Stephens JM (2005) A systematic literature review of the clinical and epidemiological burden of acute lymphoblastic leukemia (ALL). Eur J Cancer Care (Engl) 14: 53-57.
- Hruák O, Trka J, Zuna A, Polou T, Kalina J (2002) Acute lymphoblastic leukemia incidence during socioeconomic transition: selective increase in children from 1 to 4 years. Leukemia 16: 720-725.
- Ramesh PM, Marwaha RK, Anish TS (2011) Factors influencing time to diagnose of childhood ALL. Indian j Paed 32: 30-33.
- Belson M, Kingsley B, Holmes A (2007) Risk factors for acute leukemia in children: a review. Environ Health Perspect 115: 138-145.
- Chandy M (1995) Childhood acute lymphoblastic leukemia in India: an approach to managementin a three-tier society. Medical and Pediatric Oncology 25: 197-203.
- Wakeford R, Kendall GM, Little MP (2009) The proportion of childhood leukemia incidence in Great Britain that may be Leukemia. Epub 23: 770-776.
- Santoro N, Giordano P, Del Vecchio GC, Guido G, Rizzari C, et al. (2005) Ischemic stroke in children treated for acute lymphoblastic leukemia: a retrospective study. J Pediatr Hematol Oncol 12: 188-200.
- Statistics by country for acute myeloid leukemia. US census bureau, international data base 2004.
- Hoffbrand AV, Moss PAH, Pettit JE (2006) "Essential Haematology".5th Oxford: Blackwell Publishing, chapter 6. Haematologic diseases 189-191.
- Hru ák O, Trka J, Zuna J, Polou ková A, Kalina T (2002) Acute lymphoblastic leukemia incidence during socioeconomic transition: selective increase in children from 1 to 4 years. Leukemia 16: 720-725.
- Williams CK (1984) Some biological and epidemiological characteristics of human leukemia in Africans. IARC Sci Pub l63: 687-712.
- Hossain MJ, Xie L, Suzanne M, McCahan (2014) Characterization of pediatric acute lymphoblastic leukemia survival patterns by age at diagnosis. J Cancer Epidemiol 16: 865-979.
- Hjalgrim LL, Rostgaard K, Schmiegelow K, So¨derha¨ll S, Kolmannskog K, et al. (2003) Age and sex specific incidence of childhood leukemiaby immunophenotype in the Nordic countries. J Natl Cancer Inst 95: 1539-1544.
- James BO, Ajayi SO, Ogun OA, Oladokun RE (2009) Factors influencing time to diagnosis of childhood cancer in Ibadan, Nigeria. Afr Health Sci 9: 275-278.
- Mehta V, Chapman A, McNeely PD, Walling S, Howes WJ (2002) Latency between symptom onset and diagnosis of pediatric brain tumors: an Eastern Canadian geographic study. Neurosurgery 51: 365-372.
- Stefan DC, Siemonsma F (2011) Delay and causes of delay in the diagnosis of childhood cancer in Africa. Pediatr Blood Cancer 56: 80-85.
- Zombori L, Kovacs G, Csoka M, Derfalvi B (2013) Rheumatic symptoms in childhood leukaemia and lymphoma-a ten-year retrospective study. Paediatr Rheumatol Online J 4: 11-20.
- Stephen P, Hunger MD, Charles G, Mullighan MD (2015) Acute lymphoblastic leukemia in children. NEJM 373:1541-1542.
- Öztürkmen S, Akyay A, B?çakç? Z, Karakoç Y, Ar?kan?M, (2010) Delayed diagnosis of acute leukemia in a patient with bone pain and fracture. Turk J Pediatr 52: 552-555.
- Falcini F, Bardare M, Cimaz R, Lippi A, Corona F (1998) Arthritis as a presenting feature of non-Hodgkin's lymphoma. Arch Dis Child 78: 367-370.
- Lins MM, Amorim M, Vilela P, Viana M, Ribeiro RC, et al. (2012) Delayed diagnosis of leukemia and association with morbid-mortality in children in Pernambuco, Brazil. J Pediatr Hematol Oncol 34: 271-6.
- Dang-Tan T, Franco EL (2007) Diagnosis delays in childhood cancer: a review. Cancer 110: 703-713.
- Abdelkhalek ER, Sherief LM, Kamal NM, Soliman RM (2014) Factors associated with delayed cancer diagnosis in Egyptian children. Clin Med Insights Pediatr. 8: 39-44.
- Evans NT, Wakefield CE, McLoone JK, Cohn RJ (2015) Familial diagnostic experiences in paediatric oncology. Br J Cancer 112: 20-23.
Citation: Mowla MG, Choudhury AM, Khaleque MA, Haque MM, Yasmin T (2020) Physician Delay for Delayed Diagnosis of Acute Lymphoblastic Leukemia among Children in a Tertiary Care Hospital. J Pharmacol Pharmaceut Pharmacovig 4: 018.
Copyright: © 2020 Mowla MG, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.