
Placental Abruption in Primiparous Women: Risk Factors and Maternal-Fetal Prognosis at the Gynecology-Obstetrics Department of Gabriel Touré University Hospital, Bamako, Mali
*Corresponding Author(s):
Amadou BocoumDepartment Of Gynecology And Obstetrics, Gabriel TOURE University Hospital, Bamako, Mali
Tel:+223 00223760259,
Email:abocoum2000@yahoo.fr
Abstract
Introduction: Placental Abruption (PA) is a serious obstetric emergency whose frequency and severity seem particularly high among primiparous women in sub-Saharan Africa.
Objective: To determine the frequency, risk factors and maternal-fetal prognosis of PA in primiparous women at Gabriel Touré University Hospital in Bamako (Mali).
Methods: Case-control study carried out from August 2023 to July 2024. Fifty (50) primiparous women with PA (cases) were matched to 100 primiparous women without PA (controls) according to age. Socio-demographic, clinical, therapeutic and prognostic data were compared.
Results: Out of 3 436 deliveries, 307 PA were recorded (8.93%), including 50 in primiparous women (frequency 18.6%). The risk factors significantly associated with PA were: evacuation/referral (92% vs 54%; OR = 9.79; 95% CI [3.27-29.27]), total absence of prenatal consultation (52% vs 14%; OR = 0.05; 95% CI [0.01-0.17]) and the presence of hemoglobinopathy (OR = 11; 95% CI [1.24-96.89]). Caesarean section was performed in 94% of cases and blood transfusion in 64%. Maternal prognosis was marked by 8% mortality (all due to hemorrhagic shock). Fetal prognosis was dramatic with 76% fresh stillbirths and an Apgar score of 0 at the 1st minute in 76% of cases.
Conclusion: in primiparous women in Mali, PA is extremely frequent (18.6%) and burdened with very high maternal (8%) and perinatal (76%) mortality. The absence of prenatal follow-up and delay in management (late evacuations) are the main aggravating factors. Early and regular strengthening of prenatal consultations in adolescent primiparous women is the prevention priority.
Keywords
Mali; Maternal-Fetal Prognosis; Placental Abruption; Prenatal Consultations; Primiparous Women; Risk Factors
Introduction
Placental abruption, or Premature Detachment of the Normally Inserted Placenta (DPPNI), occurs when the placenta detaches from the uterine wall before birth, thereby interrupting maternal-fetal exchanges [1-3]. Its global incidence varies between 0.5% and 1.8% of pregnancies [4]. Although well-established risk factors exist, such as extreme maternal ages, women of melanodermic descent, history of caesarean section or PA, thrombophilias, use of toxic substances, Arterial Hypertension (HTA), Premature Rupture Of Membranes (PROM) and abdominal trauma [5-8], PA remains a pathology that is difficult to predict. Parity has also been identified as an important risk factor [9]. Indeed, several studies carried out in Africa, such as those of Mian D et al., in 2014 in Côte d'Ivoire [9] and Thiam O et al., [10] in Senegal the same year showed that primiparity is associated with a high frequency of PA, reaching respectively 54.2% and 36.7%. PA in primiparous women could be partly due to insufficient prenatal follow-up, which prevents early detection and management of associated risk factors [11]. Clinically, PA often manifests unpredictably, with characteristic symptoms such as dark blood metrorrhagia, permanent uterine contraction accompanied by sudden abdominal pain, and reduction or absence of active fetal movements. Paraclinically, it can be confirmed by Fetal Heart Rate (FHR) abnormalities and the demonstration of a hematoma on ultrasound [5,6]. Occurring generally during the second half of pregnancy, PA causes serious complications for the mother and fetus, making it a vital emergency. Maternal mortality is approximately 1.1 per 100,000 live births in industrialized countries [6], but can reach 6% in developing countries [10]. Despite advances in diagnosis and treatment, PA remains a severe obstetric complication and often difficult to diagnose, due to its frequent atypical forms. Few studies have been specifically carried out on PA in primiparous women in the gynecology-obstetrics department of Gabriel Touré University Hospital in Bamako. This study aims to analyze the risk factors and prognosis of PA in primiparous women in the gynecology-obstetrics department of Gabriel Touré University Hospital, a referral institution in Mali, due to the large number of evacuations to this hospital. The main objectives were to determine the frequency of PA in primiparous women, to identify the different risk factors causing PA in primiparous women, to describe the management and to establish the maternal-fetal prognosis. The research hypotheses were as follows:
- Primiparous women with PA have a less favorable maternal-fetal prognosis compared to those without complications, due to the frequency of severe forms and complications associated with PA.
- Early management and rapid diagnosis of PA reduce the mortality and morbidity rates in primiparous women.
Patients and method:
- This is a cross-sectional case-control study concerning data from the period from August 2023 to July 2024, i.e. a period of 12 months
- The study population consisted of all pregnant and parturient women admitted to the department during the collection period concerned
- We carried out exhaustive sampling for the cases including all primiparous patients who presented PA and for the controls, all primiparous patients who did not present PA. The matching criterion for cases and controls was age with one case for two controls
- Data collection was done from obstetric files, partograms, delivery register, hospitalization register, operative report register and patient referral-evacuation forms
- The data were processed and analyzed on SPSS version 22.0 software
- We used the following parameters: means, frequencies, standard deviations
- Pearson’s chi-square test and Fisher’s test were used to compare the variables of interest with a significance threshold of 5% i.e. (p < 0.05)
- NB: Fisher’s test was used for contingency tables with at least 1 count less than 5
- The Odds Ratio was used to determine the degree of relationship between the variables of interest with a 95% confidence index CI
- The gestational age was calculated from the date of last menstruation for some and for others from the first ultrasound. Ethical aspects
- The confidentiality of the data was guaranteed. Patients’ names do not appear in any document relating to the results of this study. Operational definition
- Good general condition: WHO stage 0 and 1, Fair general condition: WHO stage 2 and 3, Poor general condition: WHO stage 4
- PA I: Grade I placental abruption, the diagnosis of PA is retrospective
- PA II: Grade II placental abruption, the signs of PA are present and the fetus is alive.
- PA IIIA: Grade IIIA placental abruption, the signs of PA are present but the fetus is dead. PA IIIB: Grade IIIB placental abruption, the signs of PA are present but the fetus is dead and there is a coagulation disorder
- Good Apgar: Newborn with a score between 8 and 10 Morbid Apgar: Newborn with a score between 4 and 7 Poor Apgar: Newborn with a score < 4
Results
- Overall frequency
We recorded 3436 deliveries during the collection period, including 307 cases of placental abruption, i.e. a frequency of placental abruption of 8.93%. Among these deliveries, there were 269 primiparous women with 50 patients admitted for placental abruption, i.e. a frequency of placental abruption in primiparous women of 18.6%.
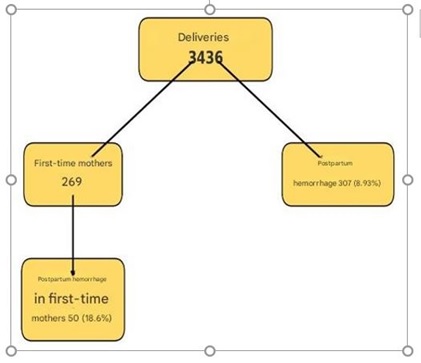 Figure 1: Flow chart.
Figure 1: Flow chart.
- Socio-demographic characteristics
The age group of 19 years and under was represented with 58% in cases and controls without statistically significant difference (p = 0.999). The mean age was 18.98 ± 2.89 years with extremes of 15 and 26 years. Uneducated patients were represented in cases and controls with respectively 64.7% and 50% without statistically significant difference (p = 0.418). Uneducated patients had 1.32 times more risk of developing PA. Referred patients were represented in cases with 92% while in controls they were represented in 54% of cases with a statistically significant difference p: 0.000. Referred patients had 9.79 times more risk of developing PA. Hemoglobinopathy was present in cases (10%) and in controls (1%) with a statistically significant difference (p = 0.016). Patients with hemoglobinopathy had 11 times more risk of developing PA. Fifty-two percent (52%) of patients had not carried out ANC in cases compared to fourteen percent (14%) of controls with a statistically significant difference (p = 0.000). The mean number of ANC was 2.51 ± 2.05 (Table 1).
|
Age group |
Number |
Total (%) |
|
|
|
|
Case (%) |
Controls (%) |
|
|
|
≤ 19 years old |
29 (58.0) |
58 (58.0) |
87 (58.0) |
|
|
20-25 years old |
19 (38.0) |
38 (38.0) |
57 (38.0) |
|
|
> 25 years old |
2 (2,0) |
4 (4.0) |
6 (4.0) |
|
|
Mean number of prenatal consultations |
Number |
Total (%) |
OR [95% CI] |
|
|
Case (%) |
Controls (%) |
|
|
|
|
0 |
26 (52.0) |
14 (14.0) |
40 (26.7) |
0.05 [0.01-0.17] |
|
1-3 |
19 (38.0) |
38 (38.0) |
57 (38.0) |
0.20 [0.07-0.60] |
|
≥ 4 |
5 (10.0) |
48 (48.0) |
53 (35.3) |
|
|
Total |
50 (100.0) |
100 (100,0) |
150 (100,0) |
Total |
|
Mode of Admission |
Number |
Total (%) |
OR [95% CI] |
|
|
Case (%) |
Controls (%) |
|
|
|
|
Self-referred |
4 (8.0) |
46 (46.0) |
50 (33.3) |
- |
|
Referred / Evacuated |
46 (92.0) |
54 (54,0) |
100 (66.7) |
9.79 [3.27-29.27] |
|
Total |
50 (100.0) |
100 (100,0) |
150 (100,0) |
|
Table 1: Data on socio-demographic characteristics.
- Clinical data on admission
PA represented 78% of the reasons for admission in cases while in controls, labor represented 41% with a statistically significant difference (p = 0.000). The mean gestational age was 35.45 ± 2.96 for cases with extremes of 24 weeks and 39 weeks. General condition was good in cases in 54% and in controls in 82% of cases with a statistically significant difference (p = 0.000). Patients in the latent phase were represented in cases (90.2%) and in controls (94.6%) without statistically significant difference (p = 0.380). FHR were absent in cases in 76% and in controls in 4% with a statistically significant difference (p = 0.000). The hemoglobin level 8-10.9 g/dl was predominant in cases with 68%, against a predominance of the level >11 g/dl in controls with 45% and a statistically significant difference (p = 0.001). The mean hemoglobin level in cases was 10.74 ± 1.46 g/dl. The predominant diagnosis in cases was Grade IIIA PA in 58% of cases while the predominant diagnosis in controls was normal labor in 41% of cases with a statistically significant difference (p = 0.000) (Table 2).
|
Final diagnosis |
Number |
|
Total (%) |
|
|
Case (%) |
Controls (%) |
|
|
Normal spontaneous labor |
0 (0,0) |
41 (41,0) |
41 (27,3) |
|
Grade IIIa placental abruption |
29 (58,0) |
0 (0,0) |
29 (19,3) |
|
Preeclampsia |
0 (0,0) |
24 (24,0) |
24 (16,0) |
|
Threatened Preterm Labor (TPL) |
0 (0,0) |
13 (13,0) |
13 (88,7) |
|
Grade II placental abruption |
12 (24,0) |
0 (0,0) |
12 (8,0) |
|
Eclampsia |
0 (0,0) |
12 (12,0) |
12 (8,0) |
|
HRP grade IIIb |
9 (18,0) |
0 (0,0) |
9 (6,0) |
|
Placenta prævia |
0 (0,0) |
5 (5,0) |
5 (3,3) |
|
Gestational age |
Number |
Total (%) |
|
|
|
Case (%) |
Controls (%) |
|
|
< 28 weeks GA |
2 (4,0) |
1 (1,0) |
3 (2,0) |
|
29 - 33 weeks GA |
13 (26,0) |
15 (15,0) |
28 (18,7) |
|
34 - 36 weeks GA |
27 (54,0) |
29 (29,0) |
56 (37,3) |
|
≥ 37 weeks GA |
8 (8,0) |
55 (55,0) |
63 (42,0) |
|
Total |
50 (100,0) |
100 (100,0) |
150 (100,0) |
Table 2: Clinical data on admission.
- Therapeutic management
Vaginal delivery represented in controls (63%) while caesarean section represented in cases (94%) with a statistically significant difference (p = 0.000). Transfusion was performed in 64% of cases against 2% of controls with a statistically significant difference (p = 0.000). In cases (32) and controls (2) all patients had received at least one unit of packed red blood cells (PRBC). Thirteen (13) patients among the cases had also received at least one unit of fresh frozen plasma (FFP). Transfer to intensive care was carried out in 17.4% of cases against 8% of controls without statistically significant difference (p = 0.135). In controls, the reasons for transfer to intensive care were eclamptic state (7/8) and hemorrhagic shock (1/8). In cases, the reasons for transfer to intensive care were hemorrhagic shock (7/8) and functional renal failure (1/8) (Table 3).
|
Mode of childbirth |
Number |
Total (%) |
|
|
Case (%) |
Controls (%) |
||
|
Vaginal delivery |
3 (6,0) |
63 (63,0) |
66 (44,0) |
|
Caesarean section |
47 (94,0) |
37 (37,0) |
84 (66,0) |
|
Total |
50 (100,0) |
100 (100,0) |
150 (100,0) |
|
Blood product administration |
Number |
Total (%) |
|
|
Case (%) |
Controls (%) |
||
|
Yes |
32 (64,0) |
2 (2,0) |
34 (22,7) |
|
No |
18 (36,0) |
98 (98,0) |
116 (77,3) |
|
Total |
50 (100,0) |
100 (100,0) |
150 (100,0) |
|
Transfer to Intensive Care |
Number |
Total (%) |
|
|
Case (%) |
Controls (%) |
||
|
Yes |
8 (17,4) |
8 (8,0) |
16 (8,1) |
|
No |
38 (82,6) |
92 (92,0) |
134 (91,9) |
|
Total |
46 (100,0) |
100 (100,0) |
146 (100,0) |
Table 3: Data on management.
- Maternal-fetal prognosis
Anemia was the most frequent complication in cases (100%) and in controls (5%) respectively. Patients are alive in 92% and 100% respectively, in cases and in controls with a statistically significant difference (p = 0.004). The cause of death in cases was hemorrhagic shock (4/4) (Table 4).
|
Maternal complications in the postpartum period |
Number |
Total (n=150) |
Pv |
|
|
Case (%) |
Controls (%) |
|
||
|
Severe anemia |
50 (100,0) |
5 (5,0) |
55 (36,7) |
0,000 |
|
Postpartum haemorrhage |
11 (22,0) |
0 (0,0) |
11 (7,3) |
0,000 |
|
Blood clotting disorders |
9 (18,0) |
0 (0,0) |
9 (6,0) |
0,000 |
|
Acute renal failure |
9 (18,0) |
1 (1,0) |
10 (6,7) |
0,000 |
|
Mother's condition |
Effectifs |
Total (%) |
|
|
|
Case (%) |
Controls (%) |
|||
|
Living |
46 (92,0) |
100 (100,0) |
146 (97,3) |
|
|
Deaths |
4 (8,0) |
0 (0,0) |
4 (2,7) |
|
|
Total |
50 (100,0) |
100 (100,0) |
150 (100,0) |
|
Table 4: Maternal prognosis.
The state of fresh stillbirth predominated in cases in 76% of cases while the live newborn predominated in controls in 95% of cases with a statistically significant difference (p = 0.000). The Apgar score 0 at the 1st minute was in cases 76% against 5% in controls. The minimal Apgar score for live newborns was 5. The Apgar score at the 5th minute of 8 to 10 in cases in 66.7% of cases against 100% in controls. The minimal Apgar score was 6. The weight of newborns between 2000-3000 g was 54% in cases and 69% in controls with a statistically significant difference (p = 0.031). The mean weight was 2536.3 ± 509.68 g. Transfer to neonatology concerned 66.7% of newborns from cases i.e. 8/12 against 27.4% of newborns from controls. In cases, the reasons for transfer to neonatology were prematurity (7/8) and hypotrophy (1/8). In controls, the reasons for transfer to neonatology were prematurity (21/26), hypotrophy (3/26); asphyxia (1/26) and malformation (1/26) (Table 5).
|
Condition of newborns at birth |
Number |
Total (%) |
|
|
Case (%) |
Controls (%) |
||
|
Live birth |
12 (24,0) |
95 (95,0) |
107 (71,3) |
|
Fresh stillbirth |
38 (76,0) |
2 (2,0) |
40 (26,7) |
|
Stillborn macerated |
0 ((0,0) |
3 (3,0) |
3 (2,0) |
|
Total |
50 (100,0) |
100 (100,0) |
150 (100,0) |
|
Apgar's score in the 1st minute |
Number |
Total (%) |
|
|
Case (%) |
Controls (%) |
||
|
0 |
38 (76,0) |
5 (5,0) |
43 (42,0) |
|
3-7 |
10 (20,0) |
28 (28,0) |
38 (25,3) |
|
8-10 |
2 (2,0) |
67 (67,0) |
69 (46,0) |
|
Transfer to neonatology |
Number |
Total (%) |
|
|
Case (%) |
Controls (%) |
||
|
Yes |
8 (66,7) |
26 (27,4) |
34 (37,6) |
|
No |
4 (33,3) |
69 (72,6) |
73 (62,4) |
|
Total |
12 (100,0) |
95 (100,0) |
117 (100,0) |
Table 5: Immediate prognosis of newborns.
Certain risk factors have been identified as favoring the occurrence of PA in cases, including non-schooling with an OR 1.32 CI [0.66-2.63] and non-follow-up of pregnancy with an OR 0.05 and CI [0.01-0.17] (Table 6).
|
Risk Factors |
Number |
OR [IC à 95%] |
|
|
Case (%) |
Controls (%) |
||
|
Illiterate |
29 (58,0%) |
51 (51,0%) |
1,32[0,66-2,63] |
|
Hemoglobinopathy |
5 (8,33%) |
1 (50,0%) |
11[1,24-96,89] |
|
Hypertension |
1 (16,7%) |
1 (50,0%) |
2,02[0,12-32,98] |
|
No prenatal care |
26 (52,0%) |
14 (14,0%) |
0,05[0,01-0,17] |
Table 6: Summary of risk factors of PA in primiparous women.
Discussion
- Limitations of the study
The retrospective analysis of non-computerized medical records presented a major difficulty due to the significant presence of missing or insufficiently filled data. This gap inevitably affected the results of the study, thus reducing statistical power and increasing the risk of bias, particularly if the missing data are not randomly distributed. This loss of information may have limited the precision of estimates, masked potential associations and restricted the feasible statistical analyses, making the interpretation of the results more complex and the generalization of the conclusions more cautious.
- Overall frequency
During the study period, we recorded 3436 deliveries, among which 307 cases of placental abruption, i.e., a frequency of 8.93%. This rate is higher than that reported by Bonkoungou et al., [12] in 2014 in Burkina Faso (1.55%), Ali Z et al., [13] in 2024 in Niger (5.20%), and Yaya S et al., [14] in 2024 in Côte d’Ivoire (0.96%). Although these frequencies are relatively high, they can be explained by the specific context of the study, the size of the study population, as well as the selection criteria of the sample.
During the study period, we admitted 269 primiparous patients. Among them, 50 presented placental abruption, i.e. a frequency of 18.6%. This result is comparable to that of Ali Z et al., [13] in 2024 in Niger, who reported a frequency of 15.4% in primiparous women, with a statistically significant association between parity and placental abruption (p = 0.001).
- Socio-demographic characteristics
The age group of under 19 years was the most represented, with 58% in the case and control groups (Pv=0.999). The mean age was 18.98 ± 2.89 years, with extremes of 15 and 26 years. This result is in agreement with that reported by Ali Z et al., [13] in 2024 in Niger, where the 25-34 years age group was predominant, representing 43.5% in the case group and 37.6% in the control group, without statistically significant association between age and the presence of placental abruption. Uneducated patients were also more frequent in cases (58%) compared to controls (51%) (Pv=0.418). Uneducated patients had a 1.3 times higher risk of developing placental abruption, which could be explained by poor knowledge of good pregnancy follow-up practices.
Referred patients were more frequent among cases (92%) than among controls (54%) with a statistically significant difference (Pv=0.000). Referred patients had a 9.79 times higher risk of developing placental abruption. This result is similar to that of Sidibé B [15] in Mali in 2024, who reported a risk of 1.9 in referred patients. This can be explained by the fact that referred patients are often those who did not initially benefit from adequate management and arrive in a critical state.
Our study reveals that hemoglobinopathy was the predominant history in cases (83.3%) and in controls (50%), with a statistically significant difference (Pv=0.016). This result is comparable to those reported by Ali Z et al., [13] in 2024 in Niger, who observed a statistically significant association between arterial hypertension and placental abruption (Pv=0.02). Chronic arterial hypertension is a well-documented risk factor for premature placental detachment, as shown by several studies. Indeed, women with chronic hypertension have a 2.4 times higher risk of PA, and this risk increases further with pre-eclampsia.
Regarding prenatal consultations, 52% of cases had not benefited from prenatal consultations, compared to 14% in controls, with a statistically significant difference (Pv = 0.000). The mean number of prenatal consultations was 2.51 ± 2.05. This result is similar to that reported by Sidibé B [15] in Mali in 2024, who observed that women who had not carried out prenatal consultation had 3.2 times more risk of developing placental abruption. According to World Health Organization recommendations, an increased number of prenatal consultations (four to eight) is associated with a lower probability of fetal mortality, by allowing early detection of complications such as arterial hypertension.
- Clinical data
Placental abruption was the predominant reason for admission in cases (78%) while in controls, labor predominated (41%) with a statistically significant difference (Pv=0.000). Our result differs from that reported by Thiam O et al., [10] in 2014 in Senegal, who observed that metrorrhagia were the most frequent (41.7%), followed by uterine contractions (27.2%) and absence of fetal heart activity (21.1%). This difference can be explained by the fact that the majority of our patients were referred with an already established diagnosis. The gestational age between 34 and 36 weeks of amenorrhea (SA) was predominant in cases (54%) and in controls (29%), with a statistically significant difference (Pv = 0.000). The mean gestational age was 35.45 ± 2.96 weeks. This result differs from that reported by Ali Z et al., [13] in 2024 in Niger, who found a statistically significant link between the occurrence of placental abruption and a gestational age greater than 37 SA. Severe anemia (hemoglobin level
<8 g/dl) was more frequent in cases (74%) than in controls (2%), with a statistically significant difference (Pv = 0.000). The mean hemoglobin level was 9.95 ± 2.20 g/dl. This result is similar to that reported by Sidibé B [15] in Mali in 2024, where a mean hemoglobin level of 11.56 ± 3.5 g/dl was observed.
- Management
Caesarean section was the predominant mode of delivery in cases (94%) versus 37% in controls, with a statistically significant difference (Pv=0.000). This result is similar to that reported by Ali Z et al., [13] in 2024 in Niger, where caesarean section was performed in 99.6% of cases of placental abruption, versus 10.3% of controls. In contrast, vaginal delivery was performed in 6% of primiparous women. These data show the importance of caesarean section in the management of placental abruption, a serious obstetric event often requiring rapid intervention. Blood transfusions were significantly more frequent in patients with placental abruption (64%) than in controls (2%), with a statistically significant difference (Pv=0.000). Similar studies carried out by Ali Z et al., [13] in Niger in 2024 (68.7% of patients with placental abruption were transfused) and Sidibé B [15] in Mali in 2024 (43.1% of cases versus 2% of controls) corroborate this observation. These data underline the severity of placental abruption as a major obstetric emergency causing significant blood loss requiring transfusions.
- Prognosis
Patients were alive in 92% of cases and in 100% of controls, with a statistically significant difference (Pv=0.004). Anemia was the predominant secondary complication in 100% of cases of placental abruption, versus 5% in controls. As in most African studies, maternal morbidity was dominated by anemia (75.4%) in the study by Biaye et al., [16] in 2019 in Senegal, in a context weakened by precarious social conditions. The condition of the newborns was also significantly different between the groups. Fresh stillbirths predominated in cases (76%), while live newborns predominated in controls (95%) with a statistically significant difference (Pv=0.000). The mean birth weight was 2536.3 ± 509.68 g. This result is similar to that reported by Thiam O et al., [10] in 2014 in Senegal, where 60% of newborns weighed less than 2500 g. In 66.7% the newborns from cases were transferred to neonatology versus 27.4% for newborns from controls. In cases, the reason for transfer to neonatology was dominated by prematurity (7/8) and hypotrophy (1/8). In controls, the reason for transfer to neonatology was dominated by prematurity (22/26); hypotrophy (2/26); asphyxia (1/26) and malformation (1/26).
Conclusion
Placental abruption remains a major obstetric emergency, particularly in primiparous women, and requires close monitoring of identifiable risk factors. This study highlights that the absence of prenatal follow-up and inadequate management of risk factors considerably increase the probability of occurrence of this pathology. Maternal-fetal prognosis depends directly on the speed of diagnosis and management. It is essential to strengthen prenatal monitoring to prevent complications associated with placental abruption and improve outcomes for mothers and newborns.
Acknowledgment
We sincerely express our thanks to all those who contributed to the completion of this study. First, we warmly thank the staff of the gynecology-obstetrics department of Gabriel Touré Hospital in Bamako for their constant support and valuable collaboration throughout this study. We also express our deep gratitude to our colleagues for their wise advice and expertise. Their academic support was decisive in carrying out this work. We also thank the patients who agreed to participate in this study, without whom this work could not have seen the light of day. Their trust and cooperation were essential.
References
- Saftlas AF, Olson DR, Atrash HK, Rochat R, Rowley D (1991) National trends in the incidence of abruptio placentae, 1979-1987. Obstet Gynecol 78: 1081-1086.
- Cisse L (2001) Évolution de la prise en charge et pronostic de l'hématome retro placentaire au centre de santé Roi Baudouin de Guédiawaye [thesis of medicine]. Université Cheick Anta Diop, Dakar, Senegal.
- Dumont A, De Bernis L, Decame C, Ba M, Pollet X (1996) Indicateurs de la coagulation intravasculaire disséminée (CIVD) dans les HRP. Med Afr Noire 43: 6-11.
- Bohec C, Collet M (2010) Hématome rétroplacentaire. Ann Fr Anesth Reanim 29: 115-119.
- Ducloy-Bouthors AS, Jessenne E, Dedet B, Deruelle P, Tournoys A, et al. (2009) Hémorragies du troisième SFAR, Paris, France.
- Boisramé T, Sananès N, Fritz G, Boudier E, Viville B, et al. (2014) Hématome rétroplacentaire. Diagnostic, prise en charge et pronostic maternofœtal: étude rétrospective de 100 cas. Gynecol Obstet Fertil 42: 78-83.
- Macheku GS, Philemon RN, Oneko O, Mlay PS, Masenga G, et al. (2015) Frequency, risk factors and feto-maternal outcomes of abruptio placentae in Northern Tanzania: a registry-based retrospective cohort study. BMC Pregnancy Childbirth 15: 274.
- Tikkanen M (2011) Placental abruption: Epidemiology, risk factors and consequences. Acta Obstet Gynecol Scand 90: 140-149.
- Mian DB, Angoi V, N’guessan KLP, Abauleth YR, Kouakou F, et al. (2014) Hématome rétro-placentaire (HRP) et mort fœtale in utero (MFIU) : à propos de 70 cas et revue de la littérature. Saraf 1: 1-5.
- Thiam O, Mbaye M, Diouf AA, Touré FB, Gueye M, et al. (2014) Epidemiological, prognostic and therapeutic aspects of retro placental hematoma (HRP) in a referral maternity in rural area. Pan Afr Med J 17: 11.
- Mezane S, Achnani M, Ziyadi M, Babahabib A, Hafidi R, et al. (2023) Hématome retro-placentaire et mort fœtale in utero : à propos de 49 cas et revue de la littérature. Int J Innov Appl Stud 3: 570-578.
- Bonkoungou P, Bako Y, Simporé A, Savadogo S, Kinda B, et al. (2014) L’éclampsie en réanimation : épidémiologie et pronostic au CHU Yalgado Ouédraogo de Ouagadougou. Rev Afr Anesth Med Urgence 19: 28-32.
- Ali Z, Issoufou Harouna B, Idé Amadou H, Sayo Djibo A (2024) Determinants of retroplacental hematoma at the Maradi mother and child health center, Niger: A case-control study. BMC Pregnancy Childbirth 24: 724.
- Yaya S, Estelle DL, Michele MMB, Narcisse KK, Alamun AI, et al. (2024) Retro Placental Hematoma: Maternal and Fetal Prognosis at the Maternity of the University Hospital of Bouake. Open J Obstet Gynecol 14: 44-56.
- Sidibé B (2024) Hématome retro placentaire études cas-témoins sur les aspects épidémio-cliques et thérapeutiques au centre de santé de référence de Bamako: USTTB-FMOS.
- Biaye B, Gassama O, Gueye MDN, Diallo M, Niass A, et al. (2019) Epidemiology and prognosis of retroplacental hematoma in a maternity ward at a regional hospital center in southern Senegal. Open J Obstet Gynecol 9: 149-157.
Citation: Bocoum A, Traoré SO, Sima M, Fané S, Sissoko A, et al. (2025) Placental Abruption in Primiparous Women: Risk Factors and Maternal-Fetal Prognosis at the Gynecology-Obstetrics Department of Gabriel Touré University Hospital, Bamako, Mali. HSOA J Reprod Med Gynaecol Obstet 10: 208.
Copyright: © 2025 Amadou Bocoum, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

