
Pneumothorax in a Spontaneously Breathing Post-Partum Woman with COVID-19 Infection
*Corresponding Author(s):
Megan SavageDepartment Of Obstetrics And Gynecology, Division Of Maternal-Fetal Medicine, Weill Cornell Medicine, 525 East 68th Street Box 122, New York, NY 10065, United States
Tel:+1 2127463225,
Email:mes9168@nyp.org
Abstract
Pneumothorax is a rare complication of SARS-CoV-2 (COVID-19) infection, occurring in 1-2% of cases [1,2]. The pathogenesis and risk factors for this complication remain unknown. In this case, we describe a 19-year-old postpartum woman who developed a spontaneous pneumothorax 29 days after vaginal delivery and Intensive Care Unit (ICU) admission for acute hypoxemic respiratory failure secondary to COVID-19 infection. She did not have any pre-existing risk factors for pneumothorax and she did not receive mechanical ventilation while in the ICU. This case illustrates that pneumothorax secondary to COVID-19 infection can present even after clinical improvement and hospital discharge, and that pneumothorax can occur in non-mechanically ventilated patients who are breathing spontaneously. Physicians must maintain a high degree of clinical suspicion for pneumothorax in all COVID-19 patients with new or worsening dyspnea regardless of age, sex, pre-existing risk factors, mechanical ventilation status, or disease time course.
Keywords
COVID-19; Post-partum; Pregnancy; Spontaneous pneumothorax
OBSERVATIONS
The patient is a 19-year-old Hispanic G1P0 at 37 0/7 Weeks Gestational Age (WGA). Her medical history is notable for class I obesity (pre-gravid body mass index of 33.7) and iron deficiency anemia. On March 21, 2020, she first presented to labor and delivery triage with two days of fever, shortness of breath and muscle aches. She was febrile to 39.2 degrees Celsius and tachycardic with a heart rate of 125 beats per minute, but her oxygen saturation on room air was 100% and her respiratory rate was normal. She was not in respiratory distress, and she did not desaturate with ambulation. Laboratory evaluation was notable for a white blood cell count of 9.8, and cell differential revealed lymphopenia. No chest x-ray was performed. Nasopharyngeal (NP) swab for SARS-CoV-2 real-time Reverse Transcription Polymerase Chain Reaction (RT-PCR) was positive. She was given 500 milliliters of normal saline and her heart rate normalized. She reported subjective improvement in her symptoms. The fetal status was reassuring. She was counseled on return precautions and discharged home.
The patient re-presented to labor and delivery five days later, on March 25, 2020, at 37 6/7 WGA. She reported interval development of labored breathing, diarrhea and cough. She was noted to be hypoxemic to 91% on room air, and she desaturated to 82% with ambulation. Repeat laboratory evaluation was notable for a new transaminitis (AST 62, ALT 104). Chest x-ray revealed diffuse alveolar infiltrates bilaterally (Figure 1). She was placed on 2 Liters (L) of oxygen via Nasal Canula (NC) and admitted to labor and delivery. Within 24 hours, the patient’s oxygen requirement increased, and she required 6L NC followed by a non-rebreather mask at 15 L to maintain an oxygen saturation >90%. She was transferred to the medical ICU and placed on oxygen via high flow nasal cannula. At that time, per the infectious disease protocol at our institution, her COVID-19 infection was treated with hydroxychloroquine. She also received azithromycin and ceftriaxone to treat a presumed secondary bacterial pneumonia. Her fevers and myalgias were treated with acetaminophen. The fetal status remained reassuring and there was no maternal or fetal indication to proceed with delivery.
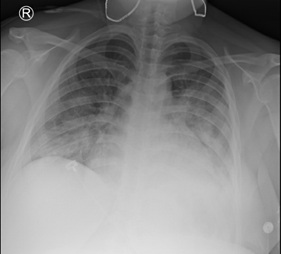 Figure 1: Chest x-ray with diffuse bilateral consolidations consistent with pneumonia secondary to COVID-19.
Figure 1: Chest x-ray with diffuse bilateral consolidations consistent with pneumonia secondary to COVID-19.
On March 29, 2020, the patient was transferred from the ICU to labor and delivery at 38 0/7 WGA in spontaneous labor. She was weaned to 4L NC, received regional anesthesia, and gave birth to a 3390 gram female infant via spontaneous vaginal delivery. The infant had reassuring APGAR scores (9/9) and the infant tested negative for COVID-19. The patient’s post-partum course was notable for persistent cough. On April 1, 2020, three days after delivery, the patient was no longer hypoxemic at rest or with exertion. She was discharged home without the need for oxygen.
On April 27, 2020, 29 days after her delivery, the patient presented to the emergency department with 3 days of shortness of breath and chest pain. She reported complete resolution of the symptoms present during her COVID-19 illness four weeks prior. She was afebrile and saturating 100% on room air. Repeat SARS-CoV-2 RT-PCR testing was positive. At that time, serology testing was unavailable. Her chest x-ray showed improvement in the previously identified alveolar infiltrates but revealed a new left-sided pneumothorax (Figure 2). There was no mediastinal shift. She underwent placement of a left-sided pigtail catheter and was admitted to the cardiothoracic surgery service. Under -20 centimeters of water suction, the left lung re-expanded. The chest tube remained on suction for 24 hours and was then placed to water seal. However, repeat chest x-ray with the chest tube on water seal revealed reemergence of the left-sided pneumothorax. The chest tube was placed back to suction and the patient was discharged the following day with a Heimlich valve. Two weeks later, the chest tube was removed in cardiothoracic surgery clinic. A final chest x-ray confirmed that the left lung remained expanded. She has remained without further pulmonary issues on follow up.
 Figure 2: Chest x-ray with left-sided pneumothorax prior to chest tube placement.
Figure 2: Chest x-ray with left-sided pneumothorax prior to chest tube placement.
DISCUSSION
Epidemiological aspects
Since December 2019, there have been 32.3 million cases of the SARS-CoV-2 (COVID-19) virus worldwide [1]. Pneumothorax has emerged as a rare but life threatening complication of COVID-19, although the specific pathophysiology, epidemiology, and risk factors for pneumothorax in this novel disease are unknown. In three (3) separate observational studies of 50-100 patients with COVID-19 in Wuhan, China, one patient (1-2%) in each study was found to have a pneumothorax [2-4]. These studies did not specify patient gender, presence of chronic lung disease, current or past tobacco abuse, or use of mechanical ventilation. Of the millions of COVID-19 cases worldwide, 21, 573 have been in pregnant or post-partum women [5]. Pneumothorax from any cause is extremely rare in pregnancy [6], and there are no existing reports of pneumothorax complicating COVID-19 infection in a pregnant or postpartum woman.
Diagnostic aspects
This is the first documented case of pneumothorax complicating COVID-19 infection in a postpartum woman. In addition to highlighting the incidence of pneumothorax in a traditionally rare demographic -- young antepartum or postpartum females -- it is noteworthy for several reasons. First, the patient developed a pneumothorax on day 29 of her COVID-19 illness, long after she had fully recovered symptomatically and been discharged from the hospital. Of the existing case reports of pneumothorax complicating COVID-19 infection, three occurred around day 20 of hospitalization, and two were present upon the initial emergency room visit [7-11]. None occurred after the patient was discharged home. This case demonstrates that the time course during which pneumothorax can complicate COVID-19 infection is highly variable; it can present as early as the first day of symptoms and as late as a month after recovery, when the patient is otherwise entirely asymptomatic.
Second, while it is common to see pneumothorax in mechanically ventilated patients who suffer from viral pneumonia complicated by ARDS, our patient’s pneumothorax occurred while breathing spontaneously. She was never treated with invasive mechanical ventilation. This corroborates existing reports and underscores the phenomenon that pneumothorax can occur in patients with COVID-19 regardless of whether they received positive pressure ventilation.
Therapeutic aspects
This case also demonstrates that the typical risk factors for pneumothorax do not need to be present in those with COVID-19. Our patient was not male, did not have a history of chronic lung disease, did not use tobacco, and was not mechanically ventilated, all known risk factors for pneumothorax pre-dating the COVID-19 pandemic. We must also consider that our patient was postpartum. Many factors contribute to the under-diagnosis of pneumothorax in pregnant and postpartum patients. The majority of pregnant and postpartum patients are healthy non-smokers without precipitating risk factors for a pneumothorax. Additionally, symptoms of a pneumothorax, namely dyspnea, are common in pregnancy. In the absence of common risk factors for a pneumothorax, providers often attribute these symptoms to the pregnancy and not an underlying pathology. Importantly, provider uncertainty regarding the safety of chest x-ray or Computed Tomography (CT) in pregnant women leads to underutilization of these diagnostic modalities.
In this case, a chest x-ray was able to promptly identify the presence of a pneumothorax. X-ray and CT are not contraindicated in pregnancy and should not be withheld if clinically indicated. However, in pregnancy these imaging modalities should supplement the provider’s clinical assessment and be used judiciously to aid in management decisions. The use of ultrasound to identify pneumothorax is an alternative diagnostic modality that avoids the small radiation exposure associated with x-ray and CT; however, obstetricians and gynecologists are not routinely trained in pleural ultrasound, and many pregnant and postpartum patients present to labor and delivery, as opposed to the emergency department, limiting its use. Based on this case, we recommend prompt pleural ultrasonography or chest x-ray in pregnant or postpartum women with COVID-19 who report new or worsening dyspnea.
CONCLUSION
Our case highlights COVID-19’s affinity for atypical presentations. We urge clinicians to maintain a high index of suspicion for pneumothorax in all patients with COVID-19, regardless of age, sex, pre-existing risk factors, mechanical ventilation status, or disease time course. We recommend pleural ultrasonography or chest x-ray in pregnant or postpartum women with COVID-19 and new or worsening dyspnea.
REFERENCES
- World Health Organization, Coronavirus Disease (COVID-19) (2020) Situation Report - 169. WHO, Geneva, Switzerland.
- Chen N, Zhou M, Dong X, Qu J, Gong F, et al (2020) Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet 395: 507?513.
- Yang X, Yu Y, Xu J, Shu H, Xia J, et al. (2020) Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir Med 8: 475?481.
- Yang F, Shi S, Zhu J, Shi J, Dai K, et al. (2020) Analysis of 92 deceased patients with COVID-19. J Med Virol: 10.
- Center for Disease Control and Prevention (2020) Data on COVID-19 during Pregnancy. CDC, Atlanta, Georgia, USA.
- Agrafiotis AC, Assouad J, Lardinois I, Markou GA (2020) Pneumothorax and Pregnancy: A Systematic Review of the Current Literature and Proposal of Treatment Recommendations. Thorac Cardiovasc Surg.
- Sun R, Liu H, Wang X (2020) Mediastinal Emphysema, Giant Bulla, and Pneumothorax Developed during the Course of COVID-19 Pneumonia. Korean J Radiol 21: 541?544.
- Wang W, Gao R, Zheng Y, Jiang L (2020) COVID-19 with spontaneous pneumothorax, pneumomediastinum and subcutaneous emphysema. J Travel Med 27: taaa062.
- Flower L, Carter JL, Rosales Lopez J, Henry AM (2020) Tension pneumothorax in a patient with COVID-19. BMJ Case Rep 13: 235861.
- Rohailla S, Ahmed N, Gough K (2020) SARS-CoV-2 infection associated with spontaneous pneumothorax. CMAJ.
- Ucpinar BA, Sahin C, Yanc U (2020) Spontaneous pneumothorax and subcutaneous emphysema in COVID-19 patient: Case report. J Infect Public Health 13: 887-889.
Citation: Savage M, LaFond E, Friedlander R, Schenck EJ, Oxford-Horrey C (2020) Pneumothorax in a Spontaneously Breathing Post-Partum Woman with COVID-19 Infection. J Reprod Med Gynecol Obstet 5: 058.
Copyright: © 2020 Megan Savage, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

