
Posterior Reversible Leukoencephalopathy Syndrome and Hypertensive Crisis Due to Obstructive Sleep Apnoea during Haemodialysis Sessions
*Corresponding Author(s):
Montserrat Picazo SánchezDepartments Of Nephrology, Emergency And Pneumology, Fundació Salut Empordà, Figueres, Spain
Email:mps4827@yahoo.es
Abstract
We present the clinical case of a 33-year-old woman on haemodialysis who suffered a severe hypertensive crisis during the sessions. In one of them, she developed Posterior Reversible Leukoencephalopathy Syndrome (PRES). Poor control of her Obstructive Sleep Apnoea Syndrome (OSA) was the cause. Correct placement of a nocturnal Continuous Positive Airway Pressure (CPAP) device, also during dialysis sessions, achieved clinical resolution and optimal control of Blood Pressure (BP).
Keywords
Continuous positive airway pressure; Haemodialysis; Hypertensive crisis; Obstructive sleep apnea-hypopnea syndrome; Reversible posterior leukoencephalopathy syndrome
Introduction
PRES is a rapidly progressive clinic radiological syndrome characterized by severe headache, nausea, vomiting, confusion, cognitive changes, seizures, and occasionally cortical blindness. Brain magnetic resonance imaging (MRI) typically shows bilateral hyper intense lesions at the parieto-occipital subcortical level on T2 and FLAIR sequences. PRES is mainly associated with rapidly developing severe hypertension, acute or chronic renal failure, severe pre-eclampsia and eclampsia, cranioencephalic or spinal cord trauma, etc. [1-4].
OSA is a common cause of secondary hypertension [5,7,8] but has very rarely been described as a cause of hypertensive encephalopathy [5-6] and never previously as a PRES during haemodialysis sessions.
Case Report
The patient presented hypertensive crisis during sessions despite dry weight adjustment, post-dilutional online hemodiafiltration, and quadruple antihypertensive therapy with Enalapril, Lercanidipine, Propranolol, and Doxazosin. As pathological history, she had to restart haemodialysis in May 2020 after chronic renal graft dysfunction, smoking, low body weight, and meningococcal sepsis at 15 years of age with cortical necrosis and chronic renal failure, migraine, hypertension, OSA due to micrognathia and retrognathia with the need for CPAP device and Budd-Chiari syndrome without alterations in the thrombosis study. Due to poor BP control, renal graft embolization had recently been performed, despite which hypertensive crisis persisted.
In July 2021, during a dialysis session, she presented a progressive increase in blood pressure from 139/91 mmHg at baseline to 231/131 mmHg at 4 hours with the onset of severe headache, nausea, and vomiting. Intravenous urapidil was administered without improvement. Due to progressive clinical worsening, she was referred to the emergency department at the end of the session. Shortly afterward, she suffered a decreased level of consciousness and a generalized tonic-clonic seizure. Midazolam, Lacosamide, and continuous infusion of labetalol were administered. Because of the suspicion of PRES, a brain MRI was performed which showed an increase in the bilateral occipital and parietal FLAIR/T2 signal, symmetrical and posteriorly distributed (Figure 1a).
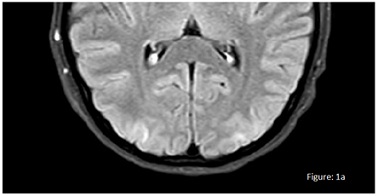 Figure 1a: Brain MRI was performed which showed an increase in the bilateral occipital and parietal FLAIR/T2 signal, symmetrical and posteriorly distributed.
Figure 1a: Brain MRI was performed which showed an increase in the bilateral occipital and parietal FLAIR/T2 signal, symmetrical and posteriorly distributed.
With the possibility of poor adherence to CPAP in mind, we consulted the pneumologist and apnoea-hypoxia indices (AHI) were found above 30-40 events per hour. The mask and inlet pressure were adjusted and the patient was warned of the urgent need for CPAP. It was also decided to place it during haemodialysis sessions as the patient was sleeping for practically the entire duration of these sessions. At the same time, enalapril was replaced by losartan. Subsequently, her evolution showed a very significant decrease in AHI events and normalisation of BP control throughout the day and on haemodialysis. After 15 days, a new brain MRI was performed, with a resolution of the lesions described (Figure 1b).
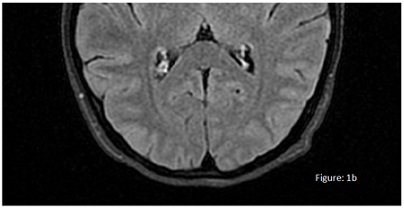 Figure 1b: A new brain MRI was performed, with a resolution of the lesions described.
Figure 1b: A new brain MRI was performed, with a resolution of the lesions described.
Discussion
Patients with ESRD have a combination of risk factors for PRES, such as hypertension, volume overload, use of erythropoietin, hyponatremia, and uremia. In dialysis patients, uremic toxins are associated with endothelial dysfunction, which can disrupt the blood-brain barrier and impair cerebral autoregulation, leading to vasogenic edema, and subsequently to PRES [1].
Acute hypertension is associated with the majority of PRES cases but is not necessary for the diagnosis, and the degree of elevation varies. Cases with normal or low-normal BP values have been reported, but it has been suggested that the rapid increase in BP rather than the absolute value delivers the most risk [2]. Our patient precisely presented rapid and severe increases in BP during haemodialysis.
The PRES diagnosis is supported by acute neurological symptoms in patients with associated comorbidities and neuroimaging features of vasogenic edema [1-4]. Prompt diagnosis of PRES is of the utmost importance because reversibility of this syndrome depends on timely therapy [1,2].
Regarding PRES treatment, prompt and aggressive antihypertensive therapy with intravenous antihypertensive drugs is recommended. Also, specific treatments aimed at the underlying diseases are required [1-4]. In our case, intravenous antihypertensive drugs were administered in addition to anticonvulsant intravenous treatment to control BP and its symptoms.
Despite adjusting dry weight, optimizing haemodialysis, and intensifying antihypertensive treatment, our patient suffered from PRES. Consequently, we began to think of poor control in the treatment of her OSA.
The prevalence of hypertensive crisis in patients with OSA and hypertension maybe 15.7% [7] and it is very prevalent in dialysis patients and can be an important cause of secondary hypertension [8]. This syndrome is also the most prevalent cause of drug-resistant hypertension and increases BP day and night [5,7,8].
In our patient the hypertensive crisis and the episode of PRES occurred during dialysis when the patient was not wearing CPAP and was sleeping, leading a very rapid increase in BP.
To our knowledge, this is the first case of PRES occurring during haemodialysis, and finally, the correct use of CPAP not only during night periods but also during dialysis sessions has achieved the complete resolution of this syndrome and has helped to get the correct control of BP 24 hours a day.
Another point very important it is to consider which antihypertensive drugs are administered in patients on haemodialysis, as some of them may be dialyzed [8]. Therefore, we decided to administer losartan instead of Enalapril, as it has been shown that most angiotensin receptor antagonists do not dialyze during conventional haemodialysis.
References
- Chiang WF, Chen PT, Chen YL, Chen MH (2019) Atypical posterior reversible encephalopathy syndrome in a noncompliant hemodialysis patient: Case report and literature review. Hemodial Int 23: E100-E103.
- Graham BR, Pylypchuk GB (2014) Posterior reversible encephalopathy syndrome in an adult patient undergoing peritoneal dialysis: a case report and literature review. BMC Nephrol 15:10.
- Vázquez Jiménez LC, Troya Saborido MI, Bancu IE, Bonet Sol J (2016) Posterior reversible encephalopathy síndrome and chronic kidney disease. About seven clinical cases and review of the literature. Nefro Plus 8: 7-13.
- Sánchez Santana AY, Monzón Vázquez T, Díaz Novo N, Valga F, Antón G, et al. (2018) Posterior reversible encephalopathy syndrome in haemodialysis: description of a case andreview of the literature. NefroPlus 10: 75-78.
- Edvardsson B (2015) Hypertensive encephalopathy associated with obstructive sleep syndrome. Acta Neurol Belg 115: 741–742.
- Silaruks S, Sawanyawisuth K (2015) A case of obstructive sleep apnoea presented with hypertensive emergency. Vasc Hypertension 24: 19.
- Khamsai S, Chootrakool A, Limpawattana P, Chindaprasirt J, Sukeepaisarnjaroen W, et al. (2021) Hypertensive crisis in patients with obstructive sleep apnea-induced hypertension. BMC Cardiovasc Disord 21:310
- Sarafidis P, Persu A, Agarwal R, Burnier M, Leeuw P, et al. (2017) Hypertension in dialysis patients: a consensus document by the European Renal and Cardiovascular Medicine (EURECA-m) working group of the European Renal Association-European Dialysis and Transplant Association (ERA-EDTA) and the Hypertension and the Kidney working group of the European Society of Hyperntension (ESH). J Hypertens 32: 620-640.
Citation: Sánchez MP, Perez MC, Macías RB, Vallmajor MC, Borroy CS, et al. (2022) Posterior Reversible Leukoencephalopathy Syndrome and Hypertensive Crisis Due to Obstructive Sleep Apnoea during Haemodialysis Sessions. J Nephrol Renal Ther 8: 071.
Copyright: © 2022 Montserrat Picazo Sánchez, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

