
Practice of Diagnosis Hysteroscopic at Gynaecological and Obstetrics Clinic at Aristide Le Dantec Teaching Hospital, Dakar, Senegal
*Corresponding Author(s):
Omar GassamaObstetrics And Gynecological Teaching Hospital Aristide Le Dantec, Cheikh Anta Diop University, Dakar, Senegal
Email:ogasse1979@gmail.com
Abstract
Objective: The aim of this work was to take stock of the practice of diagnostic hysteroscopy at the Gynaecological and Obstetrical Clinic of the Aristide Le Dantec University Hospital.
Materials and methods: This was a prospective, descriptive study of diagnosis hysteroscopy cases performed in our facility from June 15, 2017 to May 31, 2018 (11 months and 15 days). All patients received for diagnostic hysteroscopy were listed. The parameters studied concerned the socio-demographic characteristics, indications and results of the hysteroscopy. The hysteroscopy used the Storz Tele pack with a 30-degree optic and was ambulatory in the consulting room and consisted of vaginoscopy, exploration of the cervical-isthmic prolapse, the uterine cavity, the endometrium and the tubal ostia. A biopsy was performed in case of suspicious endometrial pathology. The data entry was carried out using Excel software and the analysis using SPSS version 20.0 software.
Results: During the study period, we received 168 patients. For the epidemiological profile, the mean age of the patients was 44.7 years. Gestational and mean parity were 3.1 and 2.4, respectively. The reasons for examination were dominated by menometrorrhagia 95 cases (56.5%) and suspicion of endocavitary pathologies 68 cases (40.4%) and. In our study hysteroscopy found polypoid endometrial hypertrophy in 93 cases (60.1%) and endocavitary polyps in 25 cases (18.5%). In our series 47% of the patients over 50 years old consulted for postmenopausal metrorrhagia with a suspicious endometrial tumour.
Conclusion: Hysteroscopy plays an important role in the diagnosis of intracavitary and cervico-isthmic pathologies.
Keywords
Aristide Le dantec maternity; Diagnosis hysteroscopic; Endocavitary pathologies; Senegal
INTRODUCTION
Hysteroscopy is considered to be the reference examination in the diagnosis of endocavitary pathologies [1]. It is an examination that is increasingly practiced in Dakar, Senegal and we conducted a retrospective, descriptive study whose general objective was to evaluate our practice of hysteroscopy at the gynaecological and obstetrical clinic of the Aristide Le dantec Teaching Hospital, Cheikh Anta Diop University.
Materials and methods
Type and duration of study
This was a retrospective, descriptive and analytical study conducted at the Gynaecological and Obstetrical Clinic of the Aristide Le dantec University Hospital during the period from 05 January 2017 to 31 December 2018 (24 months).
Inclusion criteria
The study population consisted of all patients received at the Hysteroscopy Unit of the Gynaecological and Obstetrical Clinic of the Aristide Le Dantec University Hospital. All patients who had undergone diagnostic hysteroscopy were included in the study.
Exclusion criteria
Patients in the second phase of the menstrual cycle and incomplete records were excluded from the study.
Data collection and analysis
Sampling was exhaustive and all hysteroscopic examinations were performed in the first part of the cycle in non-menopausal patients. Certain cervical medications (particularly prostaglandins) were administered intravaginally for 30 minutes to 1 hour on the day of the operation. Hysteroscopy was performed as an outpatient procedure in the consulting room on a gynaecological table with a 2.9 mm Bettochi optic and used saline as a distension medium and began with vaginoscopy, exploration of the cervical-isthmic prolapse, the uterine cavity and the tubal ostia.
Hysteroscopic procedures were performed in cases of endometrial pathology or intrauterine device removal.
We used the terminology of the French Society of Hysteroscopy for the hysteroscopic report. All biopsy samples were fixed in formalin and then sent by the patients to the Laboratory of Pathological Anatomy. The parameters studied were socio-demographic characteristics, history, indications and hysteroscopy results. The data collected were first coded and then entered using Epidata version 7 software. The data were then cleaned and corrected before being analyzed using Statistical Package for the Social Sciences 21 (SPSS 21). An initial univariate analysis allowed us to determine the dispersion and central tendency characteristics of each variable studied. Associations between continuous and categorical variables were measured using the Student’s test. For associations between categorical variables, Pearson’s Chi-square test and Fischer’s test were used.
RESULTS
Descriptive results
Socio-demographic characteristics
In our study 168 patients was enrolled. The mean age of the patients was 44.7 years with extremes of 18 and 82 years. Patients were most often aged between 35 and 44 years (36.3%). Patients under 45 years of age represented 67.9% of the target population as reported in table 1
|
Age range |
Effective (n) |
Percentage (%) |
|
15-24 years |
5 |
12% |
|
25-34 years |
32 |
19.6% |
|
35-44 years |
61 |
36.3% |
|
45-54 years |
29 |
17.7% |
|
55 years and more |
41 |
24.4% |
|
Total |
168 |
100% |
Table 1: Distribution of patients by age groups.
The average gestation was 3.1 with extremes of 0 and 16. Nulligests and primigests represented the majority of our patients (58.8%). The average parity was 2.4 with a standard deviation of 2.4 and extremes of 0 and 15.
Pelvic ultrasound before hysteroscopy
The completion of the ultrasound scan was almost complete (97.6%). In addition, more than ¾ of the ultrasound results (79.2%) were abnormal (Figure 1).
Endometrial thickening was the main abnormality.
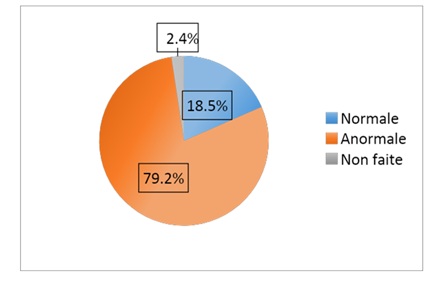 Figure 1: Distribution of patients by ultrasound (N=133).
Figure 1: Distribution of patients by ultrasound (N=133).
Table 2 shows that endometrial pathologies represented 97.6% of the lesions found.
|
Ultrasound abnormalities |
n |
(%) |
|
Endometrial hypertrophy |
89 |
66.9 |
|
Uterine fibroid type 0,1,2 |
40 |
30 |
|
IUD migration |
2 |
1.5 |
|
Hematometry |
1 |
0.7 |
|
Uterine malformation |
1 |
0.7 |
|
Total |
133 |
100% |
Table 2: Distribution of ultrasound abnormalities (N=168).
Indications for hysteroscopy
Menometrorrhagia constituted 56.5% of the indications. The size of uterine myoma averaged 2.5 cm with a standard deviation of 1.6 and extremes of 1.5 and 5.4 cm. Among married patients, 36.3% were treated for hypofertility (Table 3).
|
Indications of hysteroscopy |
n |
(%) |
|
Menometrorrhagia |
95 |
56.5 |
|
Intracavitary fibroid |
35 |
20.8 |
|
Intracavitary polyp |
33 |
19.6 |
|
Uterine synechiae |
3 |
1.7 |
|
Osteoid osteoma tumour |
1 |
0.5 |
|
IUD ablation |
1 |
0.5 |
|
Total |
168 |
100% |
Table 3: Distribution of Patients by Indication (N=168).
Results of diagnostic hysteroscopy
Endometrial pathologies account for 72.47% of patients according to table 4. Hysteroscopy found intracavitary fibroid (Figure 2) for 4.7 as reported in table 4.
|
Pathologies |
n |
% |
|
Endometrial hypertrophy |
93 |
60.1 |
|
Endometrial polyp |
17 |
8.3 |
|
Intrauterine fibroid |
8 |
4.7 |
|
Endometrial atrophy |
6 |
3.5 |
|
Endometrial tumour |
7 |
4.2 |
|
Uterine synechiae |
2 |
1.2 |
|
Osteoid metaplasia |
1 |
0.5 |
|
Uterine malformation |
1 |
0.5 |
|
Normal |
25 |
14.8 |
|
Not realized |
8 |
4.7 |
|
Total |
168 |
100% |
Table 4: Hysteroscopy results.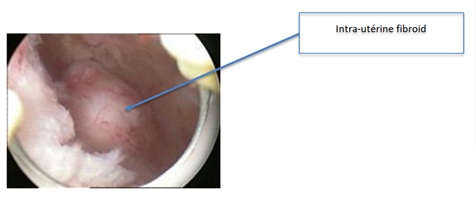 Figure 2: Intra-uterine fibroid.
Figure 2: Intra-uterine fibroid.
Complications
A total of six patients (3.6%) had complications. These were bleeding in 5 cases and pain in 1 case.
Analytical results
Concordance between ultrasound and hysteroscopy results. There is a 75.8% agreement between the results of the two tests as reported in table 5.
|
Hysteroscopy result (Abnormal) |
Ultrasound (abnormal) |
|||||
|
True (N) |
False (N) |
Total |
Kappa |
Sensibility |
Specificity |
|
|
True |
99 |
32 |
131 |
0.052 |
30.8 |
75.8 |
|
False |
18 |
8 |
26 |
|||
Table 5: Concordance between hysteroscopy and ultrasonography.
Concordance between the results of hysterosonography and hysteroscopy. There is a 94.4% agreement between the results of the two tests as reported in table 6.
|
Hysteroscopy result (Abnormal) |
Hysterosonography (abnormal) |
|||||
|
TRUE (N) |
False (N) |
Total |
Kappa |
Sensibility |
Specificity |
|
|
True |
17 |
1 |
18 |
-0.056 |
0.0 |
94.4 |
|
False |
1 |
0 |
1 |
|||
Table 6: Concordance between hysteroscopy and hysterosonography.
DISCUSSION
Limitations of the study
The number of patients received for hysteroscopy is not exhaustive. The register is poorly kept. Hysteroscopy is performed by several gynaecologists.
Socio-demographic characteristics
The mean age of the patients was 44.7 years with extremes of 18 and 82 years. Patients were most often aged between 35 and 44 years (36.3%). In Marrakech, the mean age was 32.8±5.9 years [2]. Patients under 45 years of age represented 67.9% of the target population. They were therefore in the age group susceptible to menometrorrhagia. In Bamako, the 40-49 age groups represented 42% with the extreme ages of 17 and 69 [3]. The average gestational age was 3.1 with extremes of 0 and 16 gestures. The primigravidae represented 52.9%. For SANDRACE, the large multigestates represented 30% of the patients [3].
The average parity was 2.4 gestures with extremes of 0 and 15 gestures. In Bamako like the great multigestates, the great multiparous and nulliparous were more numerous with 26% each respectively, followed by the puciparous, with 24% of the sample [3]. In our study the percentage of abnormal hysteroscopic results was higher in monogamous patients and those with marriage duration of 10 years or more. However, the difference was not statistically significant. In addition, the percentage of abnormal hysteroscopy was higher in women who had not remarried. The difference was statistically significant. A history of abortion was recorded in 40.5% of cases (N=68). The mean number of abortions was 2 with a standard deviation of 1 and extremes of 1 and 7 abortions. The median was 2 abortions. The percentage of abnormal hysteroscopic findings was higher in monogamous patients and those with marriage duration of 10 years or more. However, the difference was not statistically significant. Four patients (2.4%) had a history of extra uterine pregnancy, including 3 who had had 1 and 2 in another woman. Eighteen women (10.7%) had a history of repeat abortion.
Indications for hysteroscopy
In our series, the indications were essentially dominated by menometrorrhagia. This can be explained by the slice most found in our study. In addition, patients over 45 years of age were found in 42.3% of cases. Hypofertility constituted 36.3% of the indications for diagnostic hysteroscopy in our series. This supports Shusham and Rojansky [4] who suggested that diagnostic hysteroscopy should be included as a first-line method of investigation of marital infertility. In general, the use of hysteroscopy has been recommended only when a uterine abnormality is considered the cause of infertility [5].
Results of diagnostic hysteroscopy
Hysteroscopy concluded that an endocavitary lesion was present in 80.8% of cases. The abnormalities found were essentially submucous myomas, polyps and endometrial hypertrophies (73.1%). Intracavitary myomas represented 57.8% of these myomas. Endometrial pathologies represented 97.7% of the lesions found. For Perry, in non-menopausal patients, the probability of actually having a polyp or submucosal fibroma when the hysteroscopic diagnosis is made is 0.90 (0.69-0.97) [1,6]. Dicker performed 312 hysteroscopies in patients undergoing IVF and found 30% uterine abnormalities: polyps, submucosal myomas, adenomyosis and mucosal hyperplasia beyond the age of 40; synechiae, partitions, endometritis/endocervical endometritis and membranes in the tubal ostium previously. In addition, these lesions are more frequent after the age of 40 than before (36.1% versus 23.9%) [7]. In the Koskas study, hysteroscopy was normal in 60.5% of cases, and in women with abnormalities (39.5%), 20% had more than one abnormality and 75% of these abnormalities could be related to infertility [8].
The performance of hysteroscopy is operator-dependent. Biopsy under hysteroscopy for certain endo-uterine abnormalities had been performed in only 35.1% of cases. Hysteroscopy is an examination that requires experience and difficulties are frequent both in hysteroscopy and histological examination to differentiate between benign and cancerous lesions.
Complications
Complications of diagnostic hysteroscopy are rare (3.6%) and most often minor, with 5 bleeds (3%) and 1 pain (0.6%) in our study. Among the 25,409 hysteroscopies reported in CLARK meta-analysis only 8 complications were reported: pelvic infection, 4 uterine perforations, one bladder perforation, precipitation of a hypocalcemic attack, and one episode of angina [9]. This difference can be explained by the implementation of protocols for the prevention of complications during this study.
Concordance of pelvic ultrasound and hysteroscopy
More of the ¾ ultrasound results (79.2%) were abnormal. Endometrial thickening was the main abnormality. Endometrial pathologies represented 83% of the lesions found on ultrasound. In addition, 35 patients had a polymyomatous uterus. The size of the uterine myomas was reported on ultrasound in 7 patients with a mean of 2.5 cm with a standard deviation of 1.6 and extremes of 1.5 and 5.4 cm. There was 75.8% agreement between ultrasound and hysteroscopy in our series, while Loverro showed that ultrasound was consistent with hysteroscopy in 86% of cases, a sensitivity of 80.6%, a specificity of 79.38%, a Positive Predictive Value (PPV) of 67.03% and a Negative Predictive Value (NPV) of 91.54% [10].
Hysterosonography and hysteroscopy agreement
Hysterosonography was performed in 20 patients (11.9%). Endometrial pathologies are the most common (85%) on hysterosonography. This is confirmed by the hysteroscopy which showed 72.4% endometrial lesions. In our series, the concordance is 94.4%. During his thesis in Bamako, Sandrace found a concordance of 90% [3]. A study of 76 patients demonstrated the diagnostic power of contrast hysterosonography compared with hysteroscopy during endometrial evaluation. Deichert demonstrated that contrast hysterosonography is a highly effective means of diagnosing endometrial polyps, submucosal myomas, and synechiae [11].
Hysterosalpingography and hysteroscopy agreement
The correlation between hysteroscopy and hysterosalpingography is 70% in our study, whereas Wadhwa, who studied the correlations between hysterosalpingography and hysteroscopy in 323 infertile women, found that in 74.8% of cases the correlation between these two examinations was perfect, but the false negatives of hysterosalpingography were 13.3% and the false positives 11.7% [12].
CONCLUSION
The purpose of ambulatory hysteroscopy is to visualize endometrial abnormalities and to direct biopsies when clinical symptoms, ultrasound and hysterosonography have suspected an endometrial abnormality. Its practice needs to be popularized in Senegal.
REFERENCES
- Ohannessian A, Marcelli M, Crochet P, Cravello L, Gamerre M, et al. (2014) Hystéroscopie diagnostique. EMC - Gynécologi 10: 1-7.
- Boudaya F, Achour AA, Saoudi S, Gharsa A, Gharbi E, et al. (2016) L’apport de l’échographie dans l’exploration des métrorragies post-ménopaus Pan Afr Med J 24: 175.
- Sandrace K, Sow A, Maiga B, Toure M, Traore I (2004-2005) Evaluation diagnostique de l’hystérosonographie comparée à l’hystérographie dans les pathologies de l’endomètre au centre de santé de référence de la commune II du District de Bamako.. Thèse Médecine. Faculté de Médecine, de Pharmacie et d’Odontostomatologie. Université de Bamako, Bamako, Mali.
- Shushan A, Rojansky N (1999) Should hysteroscopy be a part of the basic infertility workup? Hum Reprod 14: 1923-1924.
- Soummani A, Aboulfalah A, Asmouki H, Benelkhaiat RB (2011) Place de l’hystéroscopie dans la prise en charge de l’infertilité. Université Cadi Ayyad. Faculté de Médecine et de Pharmacie de Marrakech. Thèse Médecine Numéro 142.
- Perry PM, Baughman VL (1990) A Complication of Hysteroscopy: Air Embolism. Anesthesiology 73: 546-547.
- Dicker D, Goldman JA, Ashkenazi J, Feldberg D, Dekel A (1990) The value of hysteroscopy in elderly women prior to in vitro fertilization-embryo transfer (IVF-ET): A comparative study. J In Vitro Fert Embryo Transf 7: 267-270.
- Koskas M, Chanelles O, Mergui JL (2020) Place de l’hystéroscopie dans l'exploration de l'infertilité. Extrait des Mises à jour en Gynécologie Médicale (Vol-2008).
- Clark TJ, Mann CH, Shah N, Khan KS, Song F, et al. (2001) Accuracy of outpatient endometrial biopsy in the diagnosis of endometrial hyperplasia. Acta Obstet Gynecol Scand 80: 784-793.
- Loverro G, Nappi L, Vicino M, Carriero C, Vimercati A, et al. (2001) Uterine cavity assessment in infertile women: Comparison of transvaginal sonography and hysteroscopy. Eur J Obstet Gynecol Reprod Biol 100: 67-71.
- Deichert U, Van de sant M, Daume E (1987) Vaginale hyserokontrastsonographie zur differential diagnostischen abklärung einespseudogestationsack. Ultraschall kiln 2: 245-248.
- Wadhwa L, Rani P, Bhatia P (2017) Comparative Prospective Study of Hysterosalpingography and Hysteroscopy in Infertile Women. J Hum Reprod Sci 10: 73-78.
Citation: Gassama O, Diadhiou M, Biaye B, Diop B, Cissé M, et al. (2020) Practice of Diagnosis Hysteroscopic at Gynaecological and Obstetrics Clinic at Aristide Le Dantec Teaching Hospital, Dakar, Senegal. J Reprod Med Gynecol Obstet 5: 044.
Copyright: © 2020 Omar Gassama, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

