
Precision Surgical Treatment for Chronic Myringitis in the Era of 4k Endoscopes
*Corresponding Author(s):
Wai Tsz ChangDepartment Of Otorhinolaryngology, Head And Neck Surgery, The Chinese University Of Hong Kong, Hong Kong
Tel:+852 35051277,
Email:waitsz@ent.cuhk.edu.hk
Abstract
Objective: To evaluate efficacy of transcanal endoscopic excision with tympanoplasty as a surgical treatment for chronic myringitis and histopathology of the disease.
Design: A prospective cohort study performed from July 2017 to January 2022 with a follow up period of 6 months to 5.4 years.
Setting: This study was performed in a university affiliated tertiary referral center.
Participants: Total thirteen patients with chronic myringitis refractory to topical treatment were enrolled. Patient's age ranged from 42 to 69 years old with a mean age of 60.2.
Intervention: Diseased ear was carefully examined for the extent of myringitis under 4K endoscope. Involved epithelial tympanic layer was peeled off or excised together with the fibrous layer depending on the extent of disease via trans-canal endoscopic approach. Trans-canal endoscopic tympanoplasty was performed after confirming the clearance of granulation tissue using tragal cartilage graft or synthetic graft using the underlay or butterfly graft approaches. Excised myringitis patches were examined by a single experienced pathologist.
Main Outcomes and Measures: Primary outcome of treatment is categorized into complete recovery, partial recovery and treatment failure. Other outcomes including duration of operation and hospitalization, audiometry were also evaluated.
Result: Ninety-two percent of patients had symptoms improvement. Ten (76.9 %) of patients achieved complete recovery after the operation. One patient suffered from graft failure with perforation required revision endoscopic tympanoplasty. Complete recovery was later achieved after a second revision operation. Two (15.4%) of patient achieved partial recovery with improvement in hearing or otorrhea with examination showed mild moist graft or mastoid cavity with no definite myringitis patch. One patient (7.7%) suffered from recurrence of myringitis over a follow up period from 6 months to 5.4 years.
Conclusion: Trans-canal endoscopic excision with tympanoplasty is a precise and efficacious treatment for intractable chronic myringitis associated with low recurrence rate. Histopathological examination of myringitis patch has provided extra information on the nature of the disease.
Keywords
Audiometry; Chronic myringitis; Endoscopes; Otitis media
Introduction
Chronic myringitis, as known as granular myringitis, is a chronic inflammation characterized by de-epithelialization and granulation of tympanic membrane with symptoms duration more than 1 month [1-3]. Whereas bullous myringitis or hemorrhagic myringitis are the acute inflammation of tympanic membrane that often associate with acute otitis media [4]. Patients suffering from chronic myringitisis commonly misdiagnosed as chronic suppurative otitis media or otitis externa since patient may experience chronic itchiness, otorrhea, otalgia in these disorders [1,2]. Chronic myringitis can be a concerning condition as chronic irritation is a known risk factor for squamous cell carcinoma of the external acoustic canal.
Many treatment modalities have been proposed over the past 20 years for treatment of chronic myringitis, including irrigation with diluted vinegar, antiseptics or anti-biotics, laser ablation and surgical excision [5-13]. A Systemic review by Chung et al. in 2018 reported treatment success with topical agents ranged from 63.6% to 100% [5].
The first randomized controlled trial comparing different treatment modalities was performed by Prakairungthong et al. in 2021 [6]. They compared treatment with diluted vinegar irrigation versus chloramphenicol ear drop in 24 patients. Eleven of 12 patients treated with 1 percent diluted vinegar had complete recovery while in the 1 per cent chloramphenicol group, 8 of 12 patients recovered. However, the difference between groups was not statistically significant.
Gentian violet, a topical agent with antibacterial, antifungal, anti-angiogenic properties, was also used for refractory discharging ear with MRSA infection [7]. Kayama et al. achieved a resolution rate of 90% in 52 patients with otorrhea refractory to systemic antibiotics or irrigation with the use of aural toileting together with application of 1% gentian violent. However, oral exposure of gentian violet was shown to have increased risk of hepatocellular carcinoma and thyroid cancer in animal study [8].
When topical treatment fails or its frequent usage affects the patients’ quality of life, surgical treatment is indicated. Since 2017, we have developed a technique of precision endoscopic ear surgery to target chronic myringitis. This study aims at evaluating efficacy of trans-canal endoscopic excision with tympanoplasty as a novel surgical treatment for chronic myringitis. Excised myringitis patches were examined by pathologist, hope to shed light on the histological nature of the poorly understood disease.
Materials And Methods
Patient selection
Cases of chronic myringitis diagnosed in a university affiliated tertiary referral center operated at the Prince of Wales Hospital and Alice Ho Miu Ling Nethersole Hospital in Hong Kong SAR between January 2017 to January 2022 were included. Patients suffered from symptomatic chronic myringitis for more than one year, persistent symptoms despite previous medical treatment and those who were medically fit and agreed for surgical treatment were included. While patient with concurrent or residual otological disease of the middle or external ear such as cholesteatoma, active bacterial infection, poor diabetes mellitus control and those with final pathological diagnosis of disease not myringitis were excluded. All patients consented to the new treatment under a research protocol were subjected to endoscopic transcanal excision and repair as described below.
Surgical technique
The surgery was performed either under local anesthesia or general anesthesia. Diseased ear was first examined under 4K endoscope (0 degree 3mm 14cm coupling to OR1 camera system, Karl Storz, Turlington, Germany or VISERA 4K Camera system, Olympus, Tokyo, Japan) to determine the extent of myringitis. (Figure 1) Digitally enhanced mode was employed under both systems (CLARA: Homogeneous illumination/ CHROMA: Contrast enhancement for the OR1 system and CLARA: Homogeneous illumination/ CHROMA: Contrast enhancement; default 4K UHD for the VISERA system). Figure 1 showed an HD view of a typical case of chronic myringitis on 4K system. Involved epithelial tympanic layer was peeled off or excised together with the fibrous layer depending on the extent of disease via endoscopic transcanal approach. Care is taken to allow the procedure to be performed with reference to debriding abnormal tissue to visually healthy layer or tissue bed, resulting in a perforation of varying sizes and shapes. The perforation was then packed with neurosurgical patties and 1:10,000 adrenaline while the tragal cartilage-perichondrium composite graft was being harvested or the artificial BiodesignTM porcine collagen graft was being prepared. Transcanal endoscopic tympanoplasty was performed after confirming the clearance of granulation tissue using tragal cartilage graft or synthetic graft using the underlay or butterfly graft approaches. External acoustic canal was packed with Gelfoam® soaked with antibiotics (olfoxacin 3% Tarivid, Daiichi, Japan) upon completion.
 Figure 1: Pre operative pictures of myringitic patch.
Figure 1: Pre operative pictures of myringitic patch.
Pathological evaluation
Excised tympanic membrane specimens were put on a layer of filter paper with labelling. They were sent for hematoxylin and eosin stain, Gramstain, fungal stain and IgG/IgG4 stain and reviewed by a single consultant pathologist.
Outcome measurement
Patients were followed up at 1-week, 1-month, 6-month then yearly post operatively in our outpatient clinic (Figures 2 and 3). Primary outcome of treatment is categorized into complete recovery, partial recovery and treatment failure. Complete recovery is defined as resolution of symptoms with physical examination showed epithelialized and dry tympanic membrane. Partial recovery is defined as improvement of symptoms without definite otoscopic finding of myringitis. Failure of treatment is defined as persistent symptoms or recurrence of myringitis over the tympanic membrane. Other outcomes including duration of operation and hospitalization, audiometry were also evaluated.
 Figure 2: post operative 4 weeks.
Figure 2: post operative 4 weeks.
 Figure 3: Post operative 6 months.
Figure 3: Post operative 6 months.
Statistical analysis was made using computer software (IBM SPSS Statistics version 26.0). Pure tone average was taken from the mean of conduction threshold at 0.5, 1,2 and 4 kHz. Wilcoxon signed ranked test was used to analyze pure tone audiogram results. A p-value less than 0.05 are considered to be statistically significant.
Results
A total of 13patients of chronic myringitis refractory to medical treatment were recruited and analyzed. Patient's age ranged from 42 to 69 years old with a mean of 60.2. Mean follow up period was 18 months, ranged from 6 months to 5.4 years. There were6 males and 7 females. Seven of the patients had previous tympanoplasty or tympano-mastoid operations done. The duration of otorrhoea experienced by patient ranged from 1 year to more than 20 years.
Ninety-two percent of patients had symptoms improvement. Ten (76.9%) of the patients achieved complete recovery after the operation. One patient suffered from graft failure with perforation required revision endoscopic tympanoplasty. Complete recovery was later achieved after a second revision operation. Two (15.4%) of the patients achieved partial recovery with improvement in otorrhea with examination showed only mild moist graft or mastoid cavity without definite myringitis patch. One patient (7.7%) suffered from recurrence of myringitis 1.5 years after the surgery and was regarded as treatment failure.
Complications and adverse events observed including one patient suffered from graft infection managed with antibiotics ear drop and another patient of impaired taste sensation after operation with spontaneous recovery after 3 months.
The average duration of operation was 96.5 minutes. Patients were discharged immediately (6 of them) or within 24 hours (7 of them) after surgery.
Comparisons were made between pure tone audiogram before and after the operation with respect to pure tone average, air-bone gaps. There was no statistically significant difference in hearing after the operation (Table 1).
|
PTA results |
Pre-operative (Mean +/- SD) |
Post-operative (Mean +/- SD) |
P-value* |
|
AC (dB) |
62.6 ± 26.9 |
66.3 ± 31.1 |
0.675 |
|
BC (dB) |
37.9 ± 23.0 |
40.4 ± 25.3 |
0.622 |
|
ABG (dB) |
24.7 ± 13.1 |
25.9 ± 13.4 |
0.858 |
Table 1: Comparison of audiological outcomes.
Note: PTA, Pure Tone Audiometry; AC, Air Conduction; BC, Bone Conduction; ABG, Air Bone Gap; SD, Standard Deviation.
*A p-value < 0.05 was considered to be statistically significant.
Pathologically, all specimens were negative for Gram stain and fungal stain. All specimens showed keratosis and had lymphocytes as their predominant inflammatory cell infiltrate. Most of them showed patchy inflammatory infiltrates with variable degrees of inflammation. There were only very few neutrophils in the specimens and all the specimens showed absent to at most focal minimal acute inflammation. There was presence of small glands in stroma in 3 of the specimens (Figures 4 and 5).
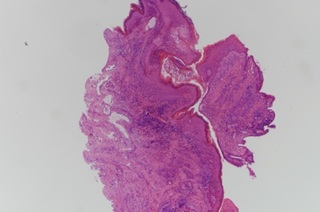 Figure 4: H&E stain 40X.
Figure 4: H&E stain 40X.
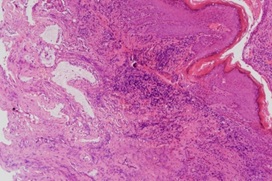 Figure 5: H&E stain 100X.
Figure 5: H&E stain 100X.
IgG/IgG4 staining was performed in 3 of the surgical specimens. They showed insignificant IgG4 to IgG ratio, from zero percent to at most 5%. One of the specimens showed 16 IgG4+ plasma cell per High Power Field (HPF), while the other specimens showed 0 to 2 IgG4+ plasma cell per HPF (Figures 6 and 7).
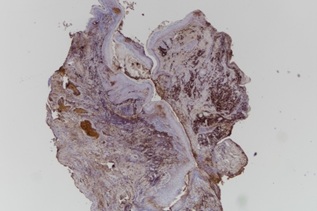 Figure 6: IgG staining.
Figure 6: IgG staining.
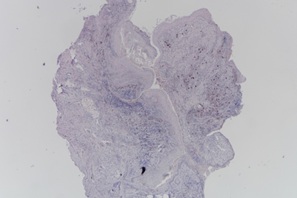 Figure 7: IgG4 staining.
Figure 7: IgG4 staining.
Discussion
When medical treatment fails, surgery is often the last resort when patients suffer from refractory chronic myringitis [5,12,13] El-selfi and Fouad performed myringoplasty in 48 patients with chronic myringitis and reported a resolution rate of 95.8% [12]. Zhang et al. reported 0% recurrence rate in a case series of 21 patients with chronic myringitis treated with surgery over a follow up period from 2 to 5 years [13]. In clinical practice, patients who had previous treatment are often reluctant to open surgical treatment but would consider more minimally invasive approaches.
Advances in endoscopes and development of related instruments have allowed us to examine regions of middle ear and operate under high resolution images and panoramic view without bone curettage via conventional microscopic approach [14]. The high definition 4K camera system allows magnification down to close to cellular levels, differentiation of healthy tissues to pathological ones can be achieved with image contrast enhancement and color shift. Its application in Endoscopic Ear Surgery (EES) to treat myringitis is then evolving. The inflammatory part of the tympanic membrane is identified with confidence by the surgeon and minimizing residual disease and over-excision of the normal tympanic membrane, achieving minimally invasiveness.
In our study, ninety-two percent of the patients experienced symptoms improvement. Seventy-six percent achieved complete recovery and the longest remission was 5.4 years if we included the patient required revision surgery in one patient. In terms of symptoms improvement, our resolution rate is comparanleto El-selfi et al and Zhang’s result, yet EES is probably having less trauma and high patient satisfaction as observed in other comparative series of tympanoplasty surgeries [11,12]. Histological examination of excised specimens identified keratosis and lymphocytosis as common features under light microscopy. Presence of keratosis in our histological findings is contrary to El-selfi et al. finding of tympanic membranes were deficient in keratinization and granulation during the quiescent stage of myringitis [11]. Gram stains were all negative and there were only very few neutrophils in the specimens and minimal acute inflammation. With the absence of usual tissue response to bacterial infection, the relationship of bacterial infection and chronic myringitis is remote. With the insignificant IgG4 to IgG ratio and number of IgG4 plasma cell under HPF, IgG4 related autoimmune inflammation is unlikely accountable for chronic myringitis.
Laser ablation is also adopted to remove the myringitic patch, resurface the tympanic membrane to promote healing [9]. Cheng and Shiao reported a resolution rate 73.3%, partial resolution rate of 23.3% in a series of 30 years with chronic myringitis treated with CO2 laser ablation over a mean follow up period of 19.7 months [10]. We believe that employing lasers in some of these cases may be of an advantage and a current evaluation of lasers in some patients is undertaken.
The result of this study can be affected by selection bias and inter-surgeon difference is also a potential bias. Most of the patients were operated by an experienced otologist (our first author) and others were operated by specialists or under our first author’s supervision. Different surgeons’ preference and operative experience may affect the surgical outcome.
This study is limited by small number of patients and a lack of detailed outcome assessments to reflect the benefits of surgery. Nevertheless, it supports the trend of employing decisive minimal invasive surgery instead of a repeated outpatient visits for chronic myringitis sufferers to topical treatment and aural toileting. Further study in form of a full outcome evaluation or a randomized control trial is needed to evaluate the true efficacy of this treatment modality.
Conclusion
Trans-canal endoscopic excision with tympanoplasty is a precise and efficacious treatment for intractable chronic myringitis associated with low recurrence rate. Histopathological examination of myringitis patch has shed light on the nature of the disease.
References
- Makino K, Amatsu M, Kinishi M, Mohri M (1988) The clinical feature and pathogenesis of myringitis granulosa. Arch Otorhinolaryngol 245: 224-229.
- Blevins NH, Karmody CS (2001) Chronic myringitis: Prevalence, presentation, and natural history. OtolNeurotol 22: 3-10.
- Neilson LJ, Hussain SS (2008) Management of granular myringitis: A systematic review. J Laryngol Otol 122: 3-10.
- Kotikoski MJ, Palmu AA, Huhtala H, Savolainen H, Puhakka HJ (2003) The epidemiology of acute bullous myringitis and its relationship to recurrent acute otitis media in children less than 2 years of age. Int J Pediatr Otorhinolaryngol 67: 1207-1212.
- Chung J, Lee DY, Kim YH (2018) Management of myringitis: Current concepts and review. Laryngoscope. 128: 2157-2162.
- Prakairungthong S, Ungchoomchoke P, Limviriyakul S, Suvarnsit K, Atipas S, et al. (2021) Efficacy of diluted vinegar in treating granular myringitis: A randomised controlled trial. J Laryngol Otol 135: 33-38.
- Kayama C, Goto Y, Shimoya S, Hasegawa S, Murao S, et al. (2006) Effects of gentian violet on refractory discharging ears infected with methicillin-resistant staphylococcus aureus. J Otolaryngol 35: 364-366.
- Littlefield NA, Gaylor DW, Blackwell BN, Allen RR (1989) Chronic toxicity/carcinogenicity studies of gentian violet in Fischer 344 rats: Two-generation exposure. Food Chem Toxicol 27: 239-247.
- Fechner FP, Cunningham MJ, Eavey RD (2002) Laser therapy for refractory myringitis in children. Otolaryngol Head Neck Surg 127:163-168.
- Cheng YF, Shiao AS (2008) Intractable chronic myringitis treated with carbon dioxide laser microsurgery. Arch Otolaryngol Head Neck Surg 134: 152-156.
- Jang CH, Kim YH, Cho YB, Wang PC (2006) Endoscopy-aided laser therapy for intractable granular myringitis. J Laryngol Otol 10:1-3
- El-Seifi A, Fouad B (2000) Granular myringitis: Is it a surgical problem? Am J Otol 21: 462-467.
- Zhang Z, Liu X, Chen S, Zheng Y (2010) Combined tympanic epithelial layer avulsion and overlay myringoplasty for diffuse granular myringitis. J Laryngol Otol 124: 842-845.
- Furukawa T, Watanabe T, Ito T, Kubota T, Kakehata S (2014) Feasibility and advantages of transcanal endoscopic myringoplasty. Otol Neurotol 35: 140-145.
Citation: Chang WT, Chan CH, Chan ABW, Yee Ng IH, Tong MCF (2022) Precision Surgical Treatment for Chronic Myringitis in the Era of 4k Endoscopes. J Otolaryng Head Neck Surg 8: 075.
Copyright: © 2022 Wai Tsz Chang, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

