
Predictors for Early Discharge Planning of Hospitalized Acute Geriatric Patients, a Retrospective Study
*Corresponding Author(s):
Bernhard HoppeUniversity Of Applied Sciences, Birkenweg 10, 64295 Darmstadt, Germany
Tel:+49 1731568440,
Email:bernhard.hoppe@h-da.de
Abstract
Purpose: When treated for an acute disorder, older adults are vulnerable for functional losses and the need of care after discharge. In a specialised geriatric ward, patients get a comprehensive treatment complementary to medical care in order to maintain and improve mobility and Activities of Daily Living (ADL) to facilitate the return to domesticity. The aim of this paper is to identify the relevant assessments at admission to predict the status at discharge for early discharge planning.
Method: In a retrospective cohort study with 351 patients, we analysed the impact of acute geriatric early rehabilitation on the functional outcome after treatment. As a sufficient improvement of ADLs and mobility we defined as a suitable endpoint at least 60 Barthel Points (ADL) and the ability for “Timed-Up-and-Go-Test” (TUG) when discharged from hospital care. To identify relevant predictors in the set of the screening assessments at admission we used linear and logistic regressions as well as odds-ratios.
Results: Statistical analysis shows that all patients benefit significantly from early rehabilitation in ADLs and the physical function. Barthel-Score, walking distance, cognition and handgrip are the strongest predictors for the outcome. Clinical condition, the medical treatment before admission, length of hospitalization, age or gender have no predictive quality.
Keywords
Acute geriatric care; Barthel score; Comprehensive treatment; Discharge planning; Geriatric assessments; Predictor analysis; Timed up and go test
Abbreviations
ADL: Activities of Daily Living
BS: Barthel-Score
BA: Barthel-Score at Admission
BD: Barthel Score at Discharge
CDT: Shulman’s Clock-Drawing-Test
GDS: Geriatric Depression Scale
HG: Handgrip averaged over both hands in kPa
M: Mean
MMSE: Mini-Mental State Examination
SD: Standard Deviation
TUG: Timed-up and Go-Test (in seconds)
TUG A: Timed-up and Go-Test at Admission
TUG D: Timed-up and Go-Test at Discharge
WD: Walking Distance in meter
Introduction
In western countries up to 50% [1] of the admitted patients are 65 years or older and most of them live at home (74% in Germany and 67.5% in OECD25 [2]). However, older patients in hospitals suffer severe risks of functional decline. Early rehabilitation of the elderly along with the clinical treatment in specialized acute geriatric wards, labeled often as Acute Care for the Elderly units (ACE), minimizes these risks. Such a treatment is important to facilitate a return to their previous social and domestic live [1,3,4]. Despite successful medical treatment, many patients need support or even institutional care after discharge. Discharge planning is an important task and should start as early as possible. Hence predictors for the expected level of independence at discharge would be helpful.
To explore the potential of a patient we need a useful and efficient outcome measure. There is a wide variety of outcome measures reported in the literature [5]. Independent or moderately assisted living requires a certain capability in ADLs plus a basic mobility. Outcome measures in a meta-analysis for acute geriatric early rehabilitation use ADL-capacity (BS) as a typical indicator, substantiated in many cases by mobility criteria [5-9]. As a sufficient improvement of ADLs and mobility, we define as a suitable endpoint at least 60 Barthel-Points, which is the approved level of independence for acceptance in a further rehabilitation unit and the ability for an untimed TUG for functional performance.
Methods
Procedures and participants
Participants in this retrospective cross sectional study were 580 randomly chosen patients of the acute geriatric ward of a medium sized hospital in a rural area in Germany from 2009-2019. Reaching the endpoint successfully is meaningful only for patients whose BA is less than 60 to avoid biasing. This applies for 351 of the basic cohort. Patients are typically aged >70 years, have multiple chronical illnesses and an acute disorder. They are transferred from the surgical or internal ward of the hospital or other hospitals nearby. The disorders treated were internal (apoplexy, cardio-vascular disorders, diabetes, pneumonia, infections) or surgical (fractures of femoral neck, pelvis, vertebral bodies and humerus, treated surgically or conservatively) or convalescents after abdominal or cardiac surgery.
During their stay (typically 14 days) patients get, complementary to acute medical care, a comprehensive training in order to maintain and improve mobility and activities of daily living. The rehabilitative training comprises intense activating daily care, physiotherapy, occupational therapy, physical exercise, cognitive training and if needed speech therapy and psychological consulting. Typically, ten multidisciplinary therapeutic training sessions are scheduled per week. The training meets the specific individual deficits of a patient. Nurses, therapists and doctors in the geriatric ward have a special geriatric qualification and meet regularly to discuss the development of the patients.
We use the following assessments, accredited by the geriatric association, at admission and discharge.
Tests applied at admission: Barthel-Score (BS), Timed-up and Go-Test (TUG), Walking Distance (WD) and Handgrip Strength (HG), Shulman’s Clock-Drawing-Test (CDT) and Mini-Mental State Examination (MMSE) and the Geriatric Depression Scale (GDS).
Tests before discharge: for physical function (TUG, HG, WD) and BS.
The Barthel-Score (BS) is a marker for the performance in ADL. A higher score is associated with a greater likelihood of being able to live with a certain degree of independence. A score 60-75 indicates a medium sized impairment. Below 60 there is growing dysfunctionality with falling Barthel-Scores. There is none or only a slight impairment for scores from 80 to 95. Handgrip strength correlates positively with overall physical performance and has a predictive validity for decline in cognition and mobility [10-12]. Handgrip is measured in kPa using the Vigorimeter (KLS Martin), which is as reliable as the JAMAR Dynamometer [13]. In the present study, we consider the averaged pressure of both hands.
TUG-testing results indicate fall risks and measure the impairment of mobility by taking the time in seconds required to stand up from a chair, followed by walking 3 meters, turn around walk back and sit down again. The TUG-performance is measured in seconds and is a quantitative indicator for physical functioning, frailty and falling risk [14,15]. A TUG time more than 12 seconds is predictive for future falls [16-18]. A drawback of the timed TUG-test is that many patients are not able to stand up and therefore are incapable to perform the timed test. Hence, a certain improvement in seconds at discharge is an outcome measure with a large floor effect. Dichotomous Tests (TUG possible or not) also reported in literature [15], avoid this effect. The timed as well as the dichotomous test are significantly associated with functional performance. Patients found able to do the TUG had a lower fall rate as those who failed. We therefore use the dichotomous test as a suitable outcome measure and monitor the TUG-time as well.
The Walking Distance (WD) is an indicator for physical function, cognition and mental status as well as their interrelationship [19,20]. This test accounts for three important aspects of overall functioning. We measure the untimed Walking Distance (WD) in meter. For the assessment of cognition, we use the Mini-Mental State Examination (MMSE) [21] and Shulman’s Clock-Drawing-Test (CDT) [22,23]. MMSE is a screening test for dementia with a maximum score of 30 points. The threshold for no or negligible impairment is 24 points. There are three categories for mild (19-23 points), moderate (10-18 points) and severe deficits for less or equal 9 marks. For performing the Clock-Drawing-Test patients have to draw the dial of an analogous watch with the watch hands set to certain time: 10 past 11. The outcome is assessed with a 6 point inverted scale: 3 or more points indicate cognitive impairment.
The score for the Geriatric Depression Scale (GDS) is determined via individual self-assessment of the patient [24]. 15 questions have to be answered by yes/no. Below 5 points there is no depression, a mild depression is between 5 to 10 points and 11 to 15 points indicate a severe depression. This test is not possible in the case of dementia. In addition, the following characteristics - taken from the hospital records - were included for each patient in the analysis: age, gender, duration of stay in days, the referral from surgical or medical department and operation or conservative treatment.
Endpoint and outcome measures
We use as an outcome target a Barthel-Score of minimum 60 points. As independence needs a certain capability to stand up and walk, the second outcome target is the ability to perform the Timed-Up-and-Go-Test (TUG). Both outcome targets combined form a meaningful endpoint.
Statistical methods
We use SPSS 27 to perform the statistical analysis [25] of the assessment data with a significance-level p <0.05 used throughout. The magnitude of a certain effect is measured using the standardized effect-size parameter f: 0.40 strong, 0.25 medium, 0.10 small [26].
The chi-squared test is used to examine odds-ratios, which quantify the impact of dichotomous measures (e.g., gender) on the outcome. We use linear and logistic regressions to examine the impact of the screening parameters taken at admission on the outcome at discharge. Linear regression analysis comprises correlation of predictors with endpoints. Logistic regression defines a model for the probability to reach a certain condition, here to meet the endpoint, using P = 0.5 as the classification cutoff.
Results
ADLs and other metric scores at admission and discharge
Table 1 shows all metric scores taken at admission. The scores at discharge, only taken for BS, TUG, HG and WD, have significantly improved. Figure 1 shows the improvement of ADLs.
|
|
Scores at admission |
Scores at discharge |
|
||||
|
|
Valid measures |
Range |
M ± SD
|
Median |
M ± SD
|
Median |
p |
|
BA < 60 (points) |
351 |
0 - 55 |
38.9 ± 13.4 |
40 |
60.9 ± 19.8 |
65 |
< 0.05 |
|
TUG a possible (seconds) |
50 |
16 -80 |
29.5 ± 10.1 |
29 |
20.7 ± 9.2 |
19 |
< 0.05 |
|
HG in kPa |
318 |
1- 66 |
26.9 ± 14.4 |
25 |
34.3 ± 15.9 |
33 |
< 0.05 |
|
WD in m |
248 |
1- 100 |
22.7 ± 21.8 |
15 |
158.0 ± 106.3 |
140 |
< 0.05 |
|
GDS-15 |
317 |
0 - 14 |
3.8 ± 2.7 |
3 |
|
||
|
MMSE |
326 |
5 - 30 |
23.3 ± 5.4 |
25 |
|||
|
CDT |
297 |
1 - 6 |
3.4 ± 1.3 |
3 |
|||
|
Age in years |
351 |
65 - 97 |
83.4 ± 6.4 |
83 |
|||
|
Weight in kg |
347 |
36 - 145 |
71.4 ± 16.1 |
69 |
|||
|
Weight female in kg |
250 |
36 - 145 |
68.2 ± 15.4 |
66 |
|||
|
Weight male in kg |
97 |
49 - 112 |
79.9 ± 14.7 |
80 |
|||
|
Hospitalization in days |
351 |
7 - 46 |
18 ± 4 |
18 |
|||
Table 1: Scores at admission and discharge.
 Figure 1: Means of Barthel Scores at Admission (BA), Before Discharge (BD) and BS-improvement (ΔBS) with standard deviations indicated by black lines for 3 BA-groups.
Figure 1: Means of Barthel Scores at Admission (BA), Before Discharge (BD) and BS-improvement (ΔBS) with standard deviations indicated by black lines for 3 BA-groups.
In table 2 we list the improvements of the 164 patients reaching the endpoint in comparison to those (187) who failed. Patients reaching the endpoint had a significant higher BD than those who failed. Patients who were able to do the TUG test at discharge had a higher increase of BS than those who didn’t. Those who didn’t reach the endpoint but were able to do the TUG failed because of an insufficient improvement of BS (-7.5 and 17.5) but the difference in TUG time compared to the successful patients was not significant.
|
Admission and Discharge Scores
|
Admission |
Discharge Reaching endpoint M ± SD
|
Discharge Not Reaching endpoint M ± SD
|
p |
ΔBS BD-BA Reaching endpoint |
ΔBS BD-BA Not reaching endpoint |
p |
|
|
n |
M ± SD
|
|||||||
|
BA < 60 (BS) |
351 |
38.9 ± 13.4 |
74.3 ± 9.1 |
48.8 ± 18.7
|
<0.05 |
28.71± 9.93 |
15.21 ± 13.02 |
<0.05 |
|
TUG A possible TUG D possible seconds |
50 |
29.5 ± 10.1 |
20.5 ± 9.3s |
25.0 ± 7.7s |
>0.05 |
29.78 ± 9.66 |
-7.5 ± 10.61 |
<0.05 |
|
TUG A not possible TUG D possible |
136 |
|
25.0 ± 7.1s
|
29.8 ± 11.3s
|
>0.05 |
28.29±10.04 |
17.5 ± 13.2 |
<0.05 |
Table 2: Mean values of assessment-scores taken at admission and discharge for patients reaching the endpoint and not reaching the endpoint.
Predictors for BD, TUG and endpoint
We analysed the predictors for BD, TUG D and the endpoint with linear and logistic regression. The results in table 3 show the important and significant predictors (Figure 2). Their strength is determined using their corresponding effect sizesf.
|
|
Predictor for BD
|
Predictor for TUG D |
Predictor for endpoint (B>60, TUG D)
|
|||
|
|
F(df,n) |
f |
χ² (df = 1) |
f |
χ² (df=1) |
f |
|
BA |
F (1,348)=433
|
1.11 |
χ² = 68.9 n = 351 |
0.56
|
χ² = 85.67 n = 351 |
0.653
|
|
HG in kPa |
F (1,315)=29.3 |
0.305 |
Not significant |
χ² = 23.7 n = 343 3 |
0.313 |
|
|
WD > 0 in m |
F (1,246)=18.2
|
0.272 |
χ² = 33.0 n = 248 |
0.45 |
χ² = 31.7 n = 248 |
0.443 |
|
MMSE |
F (1,323)= 55.3 |
0.413 |
χ² = 14.7 n = 326 |
0.243 |
χ² = 20.4 n = 326 |
0.305 |
Table 3: Linear regression and logistic regression effect sizes for bivariate analysis of BD for TUG D and endpoint (p < 0.05 for all predictors listed).
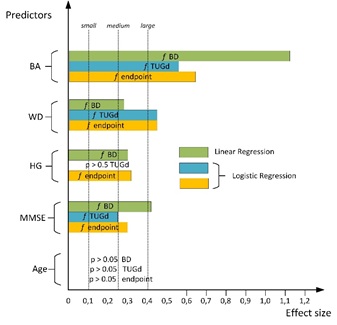 Figure 2: visualizes the results of linear and logistic regression-models of table 3.
Figure 2: visualizes the results of linear and logistic regression-models of table 3.
Strong predictors for BD are BA and MMSE, HG has a medium effect size. Strong predictors for TUG D are BA and WD. For the endpoint, BA and WD have a strong, HG and MMSE a medium effect size. TUG at admission and all other assessment parameters (Table 1) have a non-significant effect (p>0.1) and hence are not in the table.
Age as a confounder?
To rule out age as a confounder for the dominant predictors, we analyze bivariate linear regressions for BA, WD, MMSE and HG with age as the input variable. Age is a significant predictor only for handgrip but with a small effect size (p=0.027, f=0.120).
Odds-ratios for nominal predictors
Some of the admission scores are binary: gender, main diagnosis, admission from the internal or surgical ward with conservative treatment or surgery. To quantify their influence, we investigated Odds-Ratios (Table 4 and Figure 3). Moreover, for rounding up the above findings, we transform metric predictors into binary ones by using the median values taken from descriptive statistics table 1. For CDT, GDS and MMSE the threshold is set to the cut-off between impairment and no impairment. Figure 3 visualizes the results.
|
Predictor A/B |
χ² (df=1); nA/nB |
Chance A |
Chance B |
Odds = Chance A/ Chance B
|
p |
|
BA ≥40 / < 40 |
59.651 212/139 |
1.753 |
0.271 |
3.973 <6.469< 10.630 |
0.000 |
|
WD (m) ≥15/ < 15 |
23.391 116/132 |
2.667 |
0.681 |
2.297 <3.915< 6.671 |
0.000 |
|
HG (kPa) ≥25/<25
|
12.893 164/154 |
1.485 |
0.687 |
1.396 <2.191< 3.483 |
0.001 |
|
MMSE ≥24/ <24 |
14.626 197/129 |
1.318 |
0.542 |
1.535 <2.430< 3.848 |
0.000 |
|
Internal/surgical
|
4.470 148/203 |
1.162 |
0.732 |
1.033 <1.585< 2.433 |
0.035 |
|
Cons./surgery |
4.275 60/143 |
1.143 |
0.602 |
1.030 <1.898< 3.496 |
0.039 |
|
CDT < 3/ ≥3 |
3.723 77/220 |
1.406 |
0.840 |
0.989 <1.673< 2.830 |
0.054 |
|
Female/male
|
2.212; 251/97 |
0.976 |
0.701 |
0.866 <1.391< 2.235 |
0.137 |
|
Weight (kg) > 69 / ≤69 |
5.244 152/195 |
1.202 |
0.730 |
1.073 <1.648< 2.531 |
0.022 |
|
Weight men (kg) > 80/ ≤80 |
2.644 52/45 |
0.529 |
1.048 |
0.221 <0.505< 1.155 |
0.104 |
|
Weight women > 66 / ≤66 |
1.780 108/142 |
1.204 |
0,855 |
0.851 <1.408< 2.328 |
0.182 |
|
Age < 83/≥ 83 |
0.001 161/187 |
0.894 |
0.889 |
0.652 <0.994< 1.516 |
0.978 |
|
GDS < 5/ ≥5 |
0.017 219/98 |
0.991 |
0.960 |
0.641 <1.032< 1.661 |
0.896 |
|
Duration of treatment (days) <18/≥18 |
0.484 146/202 |
0.972 |
0.836 |
0.759 <1.162< 1.783 |
0.487 |
Table 4: Odds-ratios (95%-ranges) for the binary outcome variable TUG D feasible and BD ≥60.
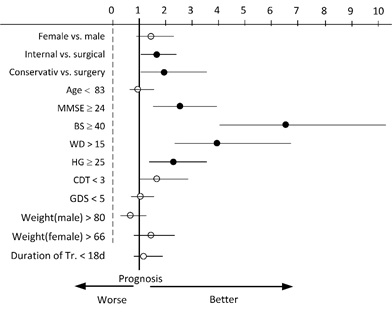 Figure 3: Odds-ratios of predictors for reaching the endpoint calculated for 351 patients with BA < 60. Lines indicate the 95% interval, filled dots are ratios with a significant difference in chances for both groups.
Figure 3: Odds-ratios of predictors for reaching the endpoint calculated for 351 patients with BA < 60. Lines indicate the 95% interval, filled dots are ratios with a significant difference in chances for both groups.
Discussion
We investigated the impact of early in-patient rehabilitation along with medical treatment in a specialized acute geriatric ward. The aim of this paper was to study the improvements of the patient’s condition from admission to discharge using standardized screening parameters taken at admission. In acute geriatric care typically outcome measures [5] combine ADLs with mobility. We use in this study for ADLs at discharge (BD ≥60) and for mobility a successful Timed-Up-and-Go-Test (TUG D = possible). A combination of both form the endpoint, which corresponds to a reasonable level of physical functioning and independence after treatment.
Descriptive statistics showed that the Barthel-score was significantly higher at discharge than at admission, with a strong effect size. Handgrip and Walking Distance also improve significantly at discharge. Patients starting the treatment with a BA between 20 and 55 points have an improvement of more than 20 points, which corresponds to a substantial reduction of the assistance needed after discharge. If 20 points is the average improvement, we see that 40 Barthel-points at admission indicate that a patient may leave the hospital with a mild ADL-impairment (BD ≥60). Patients able to do the TUG at admission have an improvement of 9sec to 20s. Patients, not able to do the TUG ad admission, were able to reach the endpoint with a TUG time of 25 seconds. Their ADL improvement was significantly higher (ΔBS 28.3) than those who failed (ΔBS 17.5).
This confirms the expected relation [5,7] between ADLs and TUG, because both measures reflect the mobility-status of a patient. BS is widely accepted [1,7] as the fundamental measure for functionality in daily living. However, Barthel-testing is less strict in quantifying the transfer capability and walking. In order to find predictors for BS-improvement we use linear regression models and classify the relevance of the significant predictors by effect sizes. As expected, the Barthel score at Admission (BA) has the strongest impact. This is in accordance with the literature [7,8]. MMSE also has a strong and HG a medium effect size. WD follows with a small effect size. Age, weight and duration of treatment are non-significant for BD. These findings are in accordance with a meta-analysis [9], which showed that ADL-improvement in acute geriatric care is not dependent on age or the days of hospitalization.
TUG-testing is a problem for geriatric patients because many cannot stand up und this results in a large floor effect. If the level of assistance needed after discharge is of interest, the dichotomous TUG D is sufficient and has the same predictive quality for fall risks as the timed TUG [15]. Less assistance is required, if a patient can stand up and walk.
Predictors for TUG D were BA and WD with the strongest impact. The known correlation [27] with cognition (MMSE) is also significant but only with a small effect size. Age, weight and duration of treatment are non-significant.
Typical geriatric patients will not achieve normal functional mobility after treatment. The TUG time under the 12 seconds limit stands for normal mobility [16], but no patient was able to perform the TUG under 12 s at admission and only 12 at discharge. These small numbers indicate, that TUG-times are not suitable as criteria for mobility of acute geriatric patients. The meta- analysis [9] also shows large floor-effects and TUG-times at admission of around 30s and an average improvement of 10s and this is in perfect agreement with our results.
Predictors for reaching the endpoint: BA and WD are strong predictors. HG and MMSE only show medium effect strength. Age, weight, GDS and hospitalization in days are not significant. This ranking of the effect sizes maybe interpreted as follows. BA is relevant for BD. Walking is a valid and reliable quantifier for physical function [19,20] and a part of the TUG-test. HG is an indicator for overall static physical strength [8,12] and hence a strong HG favours higher BD, but is less relevant for the TUG which has multifactorial components and a dynamic aspect. MMSE has a strong effect on BD and a medium effect size on the endpoint. This may be either related to moderate impact on physical function, or, more likely, to the small spread of MMSE-scores found in our data. Our patients typically have no relevant impairments in cognition (mean 23.3 ± 5.4, Median 25) and hence small differences in MMSE-scores can only produce limited differences in the outcome.
Odds-Ratios for reaching the endpoint support the ranking of metric predictors by effect sizes. Significant Odds were found for BA ≥40, WD >15m, MMSE ≥24 and HG ≥25 kPa. In case of the surgical patients only conservative treatment is significantly favorable as compared to an operation, and patients admitted from an internal ward have higher Odds than those from a surgical ward. Again BA and WD are most important, followed by MMSE and HG. Note, that age and gender yield non-significant Odds.
Age is expected to be a marker for functional decline and hence maybe confounding. However, bivariate linear regression for BA, WD, MMSE with age as predictor result in non-significant models. HG is the only predictor that exhibits a significant correlation with age as reported already in [28] and declines by 0.29 kPa/(year of age), which is of no clinical relevance. Age is no relevant confounder for the dominant predictors. Even the oldest benefit from the comprehensive treatment and improve their ADLs and mobility significantly as already noted in [9].
Conclusion
As a basic rule, which could be useful in clinical practice, we find that a substantial BA-score of around 40 is the best starting point for the comprehensive treatment. This should be backed up by walking distance of more than 15m. Patients with these competences at admission are very likely to reach a basic level of independence at discharge. We emphasize that some parameters of the patient’s status at admission, which seem to be important at first glance, lack any predictive quality. In particular, these are clinical condition, the medical treatment, length of hospitalization, weight, age or gender. They are non-predictive for increased mobility and independence. Even if the combined endpoint is not achieved, all geriatric patients benefit from acute rehabilitative care of the elderly.
Availability of data and materials
Data are available on request to the author B. Hoppe (bernhard.hoppe@h-da.de)
Ethics approval and Consent to participate
This study was performed in accordance with the Declaration of Helsinki. Written informed consent to the use of their anonymized health data obtained during their stay in the hospital was provided from each participant during the standard procedures at admission. This has been approved by the ethics committee of the Krankenhaus Korbach, Korbach, Hesse, Germany. The study was retrospectively registered on 2nd July 2019 by the ethic commission of the hospital und filed under registration number (MG1/569/770/2019).
Competing Interests
The authors confirm that there are no competing interests.
Authors’ Contribution
AH designed the study and collected the patients’ data. BH analyzed and interpreted the data using statistical methods. AH analyzed the clinical impact of the analysis. Both authors contributed on equal shares in writing the manuscript and have read and approved the final manuscript.
Acknowledgement
We thank Krankenhaus Korbach and in particular the clinical director Dr. A. W. Schneider for the support and encouragement making this study feasible.
References
- Kosse NM, Dutmer AL, Dasenbrock L, Bauer JM, Lamoth CJC (2013) Effectiveness and feasibility of early physical rehabilitation programs for geriatric hospitalized patients: A systematic review. BMC Geriatr 13: 107.
- OECD (2019) Health at a Glance 2019: OECD Indicators. OECD Publishing, Paris, France.
- Fox MT, Sidani S, Persaud M, Tregunno D, Maimets I, et al. (2013) Acute care for elders components of acute geriatric unit care: systematic descriptive review. J Am Geriatr Soc 61: 939-946.
- Baztán JJ, Suárez-García FM, López-Arrieta J, Rodríguez-Mañas L, Rodríguez-Artalejo F (2009) Effectiveness of acute geriatric units on functional decline, living at home, and case fatality among older patients admitted to hospital for acute medical disorders: Meta-analysis. BMJ 338.
- Heldmann P, Werner C, Belala N, Bauer JM, Hauer K (2019) Early inpatient rehabilitation for acutely hospitalized older patients: A systematic review of outcome measures. BMC Geriatr 19: 189.
- Zucchelli A, Vetrano DL, Grande G, Calderón-Larrañaga A, Fratiglioni L, et al. (2019) Comparing the prognostic value of geriatric health indicators: A population-based study. BMC Med 17: 185.
- Burckhardt H, Burger M (2012) Ergebnisse und Prädiktoren der geriatrischen Frührehabilitation im Akutkrankenhaus. Zeitschrift für Gerontologie und Geriatrie 45: 138-145.
- Cohen ME, Marino RJ (2000) The tools of disability outcomes research functional status measures. Arch Phys Med Rehabil 81: 21-29.
- Kwetkat A, Lehmann T, Wittrich A (2014) Geriatrische Frührehabilitation. Zeitschrift für Gerontologie und Geriatrie 47: 372-378.
- Rijk JM, Roos PR, Deckx L, van den Akker M, Buntinx F (2016) Prognostic Value of handgrip strength in people aged 60 years and older: A systematic review and meta-analysis. Geriatr. Gerontol Int 16: 5-20.
- Selakovic I, Dubljanin-Raspopovic E, Markovic-Denic L, Marusic V, Cirkovic A, et al. (2019) Can early assessment of hand grip strength in older hip fracture patients predict functional outcome? PLoS One 14: 0213223.
- Syddall H, Cooper C, Martin F, Briggs R, Sayer AA (2003) Is grip strength a useful single marker of frailty? Age Ageing 32: 650-656.
- Neumann S, Kwisda S, Krettek C, Gaulke R (2017) Comparison of the Grip Strength Using the Martin-Vigorimeter and the JAMAR-Dynamometer: Establishment of Normal Values. In Vivo 31: 917-924.
- Podsiadlo D, Richardson S (1991) The timed "Up & Go": A test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 39: 142-148.
- Large J, Gan N, Basic D, Jennings N (2006) Using the timed up and go test to stratify elderly inpatients at risk of falls. Clin Rehabil 20: 421-428.
- Bischoff HA, Stähelin HB, Monsch AU, Iversen MD, Weyh A, et al. (2003) Identifying a cut-off point for normal mobility: A comparison of the timed 'up and go' test in community-dwelling and institutionalised elderly women. Age Ageing 32: 315-320.
- Kojima G, Masud T, Dendrick D, Morris R, Gawler S, et al. (2015) Does the timed up and go test predict future falls among British community-dwelling older people? Prospective cohort study nested within a randomised controlled trial. BMC Geriatr 15: 38.
- Gates S, Smith LA, Fisher JD, Lamb SE (2008) Systematic review of accuracy of screening instruments for predicting fall risk among independently living older adults. J Rehabil Res Dev 45: 1105-1126.
- Imms FJ, Edholm OG (1981) Studies of gait and mobility in the elderly. Age Ageing 10: 147-156.
- Harada ND, Chiu V, Stewart AL (1999) Mobility-related function in older adults: Assessment with a 6-minute walk test. Arch Phys Med Rehabil 80: 837-841.
- Folstein MF, Folstein SE, McHugh PR (1975) "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12: 189-198.
- Brodaty H, Moore CM (1997) The Clock Drawing Test for dementia of the Alzheimer's type: A comparison of three scoring methods in a memory disorders clinic. Int J Geriatr Psychiatry 12: 619-627.
- Shulman KI, Gold DP, Cohen CA, Zucchero CA (1993) Clock?drawing and dementia in the community: A longitudinal study. Int J Geriatr Psychiatry 8: 487-496.
- Allgaier A-K, Kramer D, Mergl R, Fejtkova S, Hegerl U (2011) Validität der Geriatrischen Depressionsskala bei Altenheimbewohnern: Vergleich von GDS-15, GDS-8 und GDS-4. Psychiatr Praxis 38: 280-286.
- Field A (2013) Discovering Statistics Using IBM SPSS Statistics (4thedn). SAGE Publications, London, UK.
- Cohen J (1992) A power primer. Psychol Bull 112: 155-159.
- Van Patten R, Lee EE, Graham SA, Depp CA, Kim HC, et al. (2020) The Utility of the Timed Up-and-Go Test in Predicting Cognitive Performance: A Cross-Sectional Study of Independent Living Adults in a Retirement Community. J Appl Gerontol 39: 1163-1168.
- Steiber N (2016) Strong or Weak Handgrip? Normative Reference Values for the German Population across the Life Course Stratified by Sex, Age, and Body PLoS One 11: 0163917.
Citation: Hoppe A, Hoppe B (2021) Predictors for Early Discharge Planning of Hospitalized Acute Geriatric Patients, A Retrospective Study. J Gerontol Geriatr Med 7: 091.
Copyright: © 2021 Annette Hoppe, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

