
Prolonged QTc Interval in Stress-Induced Takotsubo Cardiomyopathy
*Corresponding Author(s):
Deepti BhandareDivision Of Cardiology, Advent Health Sebring, Florida, United States
Tel:+1 863386005,
Email:deepti.bhandare@adventhealth.com
Abstract
Takotsubo Cardiomyopathy is a non-ischemic cardiomyopathy characterized by reversible apical ballooning of the left ventricle presenting with a clinical syndrome mimicking acute coronary syndrome in the absence of significant coronary disease. Prolongation of the QTc interval may be either acquired or congenital and poses a significant risk of syncope and sudden cardiac death, regardless of the etiology. Acquired long QTc is generally associated with anti-arrhythmic agents, anti-depressants, or antibiotics, whereas congenital long QT arises from mutations in genes that code for ion channels within myocytes. Herein, we describe a 57-year-old woman who underwent in-patient workup for suspected acute coronary syndrome that revealed takotsubo cardiomyopathy with prolonged QTc.
BACKGROUND
Takotsubo Cardiomyopathy [TCM] is a rare subtype of non-ischemic cardiomyopathies that presents with reversible apical ballooning of the left ventricle. TCM often presents as a clinical syndrome mimicking acute coronary syndrome with ST elevations, T wave inversions, systolic dysfunction and substernal chest pain following profound psychological stress and accounts for approximately 1-2 percent of patients presenting with suspected acute coronary syndrome that is troponin positive. The pathogenesis of TCM is still not well understood but proposed mechanisms involve coronary vasospasm and catecholamine excess.
The finding of transient prolonged QTc in the setting of Takotsubo Cardiomyopathy is a rarely characterized phenomenon that must be investigated further due to the risk of life-threatening arrhythmias, such as torsades de pointes and ventricular fibrillation, associated with it. While prolonged QTc has been previously noted to be associated with Takotsubo Cardiomyopathy, it has only been recognized a handful of times and this case presents a woman with severely prolonged QTc. This case contributes to the growing body of evidence that Takotsubo Cardiomyopathy may present with prolonged QTc interval and as such practitioners must be aware of this potentially life-threatening association.
CASE PRESENTATION
57-year-old female presented to emergency department with complaints of acute, progressive shortness of breath with cough with pinkish productive sputum and diaphoresis for one day. She denied chest pain or palpitations. She denied any fevers and recent travel and sick contacts. Albuterol and Solumedrol breathing treatments were administered en route by EMS. She had a past medical history of chronic bronchitis, hypertension, hyperlipidemia, migraine headaches, depression, anxiety and back pain. She was an active smoker who smokes half a pack per day for the last 30 years. Family history significant for MI in mother at age 65, father with pacemaker. Her home medication included hydralazine 50 mg bid, metoprolol 25 mg daily, furosemide 40 mg Po daily, citalopram 40 mg PO daily, escitalopram 20 mg Po daily.
She reported that she had been very stressed and anxious for the last one week as her husband had met with a car accident. Her first husband had died 30 years ago in a car accident and she had been reliving this trauma. On presentation, her vitals were: temperature 96.2 F, blood pressure 185/74 mm Hg, heart rate 66 beats per minute (bpm), respiratory rate 22 and oxygen saturation of 94% on room air. She appeared in moderate distress, diaphoretic, tachypneic with the use of accessory muscles. She had decreased breath sounds in bilateral lungs along with 2+ pedal edema bilaterally.
INVESTIGATIONS
Initial EKG showed sinus rhythm with T-wave inversions in anterior leads and ST depression in lateral leads with a slightly prolonged QTc, calculated with Bazett formula, at 488 msec [normal is less than 470 msec for females, figure 1. Troponin and pro-BNP were elevated in the emergency department at 0.34 ng/mL [normal is less than 0.04 ng/ml] and 5878 pg/mL [normal is less than 700ng/ml] respectively, prompting admission for non-ST elevation myocardial infarction. Patient was then initiated on IV Lasix, beta-blockers and heparin. Chest X-ray and chest CT performed in the emergency department revealed bilateral pleural effusions but negative for pulmonary embolism. Repeat EKG on admission showed worsening of inverted T waves in anterior and septal leads as well as worsening of QTc at 648 msec. Repeat labs on admission showed worsening of troponin and pro-BNP at 0.46 ng/mL and 24,347 pg/mL respectively. 2-dimensional echocardiogram performed at time of admission revealed a severe systolic dysfunction with an LVEF less than 20% with preserved left ventricular basal function but severely akinetic apical cap, suspicious of apical ballooning syndrome along with mild aortic stenosis. Heart catheterization showed normal coronaries with severely depressed LV function and akinetic left ventricular apex.
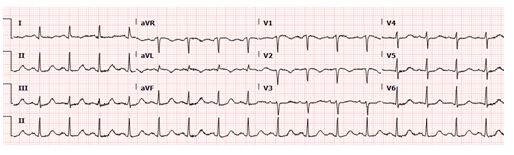 Figure 1: EKG showing normal sinus rhythm, anteroseptal t wave inversions with QTc interval of 488 msec.
Figure 1: EKG showing normal sinus rhythm, anteroseptal t wave inversions with QTc interval of 488 msec.
Her breathing was improving on IV Lasix and BiPap. Admission labs also found her to be severely acidotic with a lactic acid >10. Serum potassium and magnesium were found to be low on admission at 3.3 mmol/L and 1.5 mg/dL, respectively. Her escitalopram and citalopram were discontinued on admission day two because of the known association with prolonged QTc. She was started on spironolactone 25 m PO daily, sacubitril-valsartan 49/51 mg PO BID and metoprolol succinate 50 mg PO daily.
By admission day two, her repeat echo showed improved systolic function with an LVEF of 30-35% and small pericardial effusion which remained largely unchanged on a repeat echo performed the next day. The longest QTc on EKG was recorded on admission day three at 708 msec, figure 2. Potassium was kept above 4.5 mmol/L and magnesium was kept above 2.0 mg/dL throughout the remainder of her stay in the hospital. Upon discharge, EKG showed improved but still prolonged QTc at 628 msec, figure 3. Her prolonged QTc was managed with beta blockers and making sure that her heart rate was dropping below 60 bpm and correcting the electrolytes. Despite several days of severely prolonged QTc and Takotsubo Cardiomyopathy, there were no episodes of PVCs or ventricular tachycardia recorded. Patient was discharged home after five days in the hospital with a lifevest for prevention of sudden cardiac death and beta blockers.
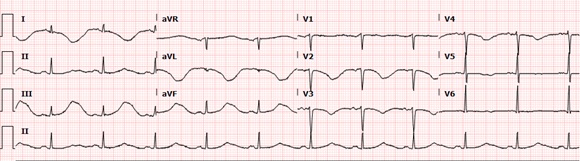 Figure 2: EKG showing normal sinus rhythm, prolonged QTc interval of 708msec.
Figure 2: EKG showing normal sinus rhythm, prolonged QTc interval of 708msec.
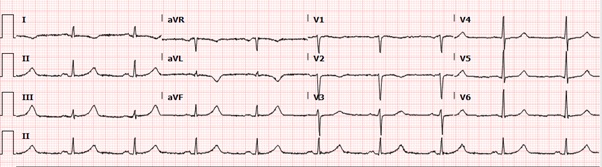
Figure 3: EKG showing normal sinus rhythm, prolonged QTc of 628 msec.
DIFFERENTIAL DIAGNOSES
Acute coronary syndrome, ischemic cardiomyopathy, NSTEMI, Prinzmetal angina, Long QT Syndrome and QT prolonging medications
OUTCOME AND FOLLOW-UP
Follow-up echocardiogram in three weeks showed a normalized ejection fraction of 55-60%. Follow-up EKG at the same time showed complete resolution of the QTc but the T-wave inversions persisted. Her lifevest was discontinued and she was maintained on heart failure medications which included metoprolol, sacubitril-valsartan and aldosterone.
DISCUSSION
Takotsubo Cardiomyopathy (TCM) is a rare subtype of the non-ischemic cardiomyopathies, known as a stress cardiomyopathy. TCM presents as transient regional left ventricular systolic dysfunction with apical ballooning, mimicking Acute Coronary Syndrome (ACS); however, the area of wall hypomotility extends beyond that perfused by a single coronary artery [1]. TCM has a predilection for women over men, occurring at a rate of 89.9 percent in women, according to the International Takotsubo Registry and affects post-menopausal women disproportionately [2]. TCM has an overall prevalence of 1-2 percent in patients presenting with troponin-positive ACS or suspected ST-elevation MI [3]. The pathogenesis behind TCM is not well understood; however, some postulated mechanisms include catecholamine excess, microvascular dysfunction and coronary artery vasospasm [4,5]. The role of catecholamines in the development of TCM seems to be supported by the fact that it is associated with profound physical or emotional stress, suggesting that TCM may be caused by catecholamine-induced coronary spasm, resulting in stunning of the myocardium or direct myocardial toxicity [6,7]. Evidence for the role catecholamines play in development of TCM comes from studies in which participant’s serum catecholamines were measured and found to be elevated [4,8]. When catecholamine elevations are compared between those with stress cardiomyopathy and those with acute coronary syndrome, plasma catecholamines were significantly higher in the patients with stress. However, elevation in catecholamines is not always present and some studies have reported normal levels [9].
While catecholamine excess appears to be one of the most common pathogenetic features of stress cardiomyopathy, some studies have observed evidence of coronary vascular dysfunction which may be catecholamine-induced. Examples include evidence of multifocal coronary vasospasm on coronary angiography and abnormal myocardial perfusion that resolves with myopathy resolution [10,11]. The fact that stress cardiomyopathy appears to have a predilection for postmenopausal women may be more than coincidence and various mechanisms have been discovered which may explain the association between postmenopausal women and stress cardiomyopathy. Postmenopausal women with a history of stress cardiomyopathy were found to have impaired endothelium function, excessive vasoconstriction, and augmented sympathetic activation in response to mental stress compared with postmenopausal controls as well as abnormal coronary response to either acetylcholine and/or adenosine in majority of women with stress cardiomyopathy [12,13].
Takotsubo cardiomyopathy has also been associated with several electrocardiographic changes, including ST segment elevations like acute ST-elevation MI, often in the anterior precordial leads [14]. Studies have also shown an association with ST depression, T wave inversions, and prolonged QT [2,4,15]. QT prolongation in stress cardiomyopathy was associated with life-threatening ventricular arrhythmias in up to 8 percent of cases in one study [16]. Mayo Clinic has established four criteria that must be met for the diagnosis of stress cardiomyopathy, consisting of transient LV systolic dysfunction, absence of obstructive coronary disease or evidence of acute plaque rupture, new ECG changes or elevated cardiac troponins and absence of pheochromocytoma or myocarditis [17,18].
The QT prolongation in TCM is postulated to result from the reduced repolarization reserve and intramyocyte calcium overload. The mechanisms described as pause-dependent, a long-short sequence that characteristically triggers QT prolongation [19]. Kinori et al., reported that patients with TCM-associated QT prolongation were at a greater risk for torsades de pointes and mortality than TCM patients without QT prolongation [20]. The finding of transient prolonged QT in the setting of Takotsubo Cardiomyopathy is a rarely characterized phenomenon that must be investigated further due to the risk of life-threatening arrhythmias, such as torsades de pointes and ventricular fibrillation, associated with it. While prolonged QT has been previously noted to be associated with Takotsubo Cardiomyopathy, it has only been recognized a handful of times and this case presents a woman with severely prolonged QTc. This case contributes to the growing body of evidence that Takotsubo Cardiomyopathy may present with prolonged QT and as such practitioners must be aware of this potentially life-threatening association.
LEARNING POINTS
• Takotsubo cardiomyopathy is a non-ischemic stress-induced cardiomyopathy associated with transient apical ballooning that mimics acute coronary syndrome
• Long QT has both congenital and acquired causes; acquired causes are commonly antibiotics and antipsychotic medications; however, Takotsubo must also be recognized as an important cause of long QT
REFERENCES
- Sato H. Tateishi H, Uchida T (1990) Takotsubo-type cardiomyopathy due to multivessel spasm. In: Kodama K, Haze K, Hon M (eds.). linical aspect of myocardial injury: From ischemia to heart failure. Kagakuhyouronsha, Tokyo, Japan.
- Templin C, Ghadri JR, Diekmann J, Napp LC, Bataiosu DR, et al. (2015) Clinical Features and Outcomes of Takotsubo (Stress) Cardiomyopathy. N Engl J Med 373: 929-938.
- Kurowski V, Kaiser A, von Hof K, Killermann DP, Mayer B, et al. (2007) Apical and midventricular transient left ventricular dysfunction syndrome (tako-tsubo cardiomyopathy): Frequency, mechanisms, and prognosis. Chest 132: 809-816.
- Wittstein IS, Thiemann DR, Lima JA, Baughman KL, Schulman SP, et al. (2005) Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med 352: 539-548.
- Paur H, Wright PT, Sikkel MB, Tranter MH, Mansfield C, et al. (2012) High levels of circulating epinephrine trigger apical cardiodepression in a β2-adrenergic receptor/Gi-dependent manner: A new model of Takotsubo cardiomyopathy. Circulation 126: 697-706.
- Gianni M, Dentali F, Grandi AM, Sumner G, Hiralal R, et al. (2006) Apical ballooning syndrome or takotsubo cardiomyopathy: A systematic review. Eur Heart J 27: 1523-1529.
- Nef HM, Möllmann H, Kostin S, Troidl C, Voss S, et al. (2007) Tako-Tsubo cardiomyopathy: Intraindividual structural analysis in the acute phase and after functional recovery. Eur Heart J 28: 2456-2464.
- Akashi YJ, Nakazawa K, Sakakibara M, Miyake F, Musha H, et al. (2004) 123I-MIBG myocardial scintigraphy in patients with “takotsubo” cardiomyopathy. J Nucl Med 45: 1121-1127.
- Madhavan M, Borlaug BA, Lerman A, Rihal CS, Prasad A (2009) Stress hormone and circulating biomarker profile of apical ballooning syndrome (Takotsubo cardiomyopathy): Insights into the clinical significance of B-type natriuretic peptide and troponin levels. Heart 95: 1436-1441.
- Tsuchihashi K, Ueshima K, Uchida T, Oh-mura N, Kimura K, et al. (2001) Transient left ventricular apical ballooning without coronary artery stenosis: A novel heart syndrome mimicking acute myocardial infarction. Angina Pectoris-Myocardial Infarction Investigations in Japan. J Am Coll Cardiol 38: 11-18.
- Ito K, Sugihara H, Katoh S, Azuma A, Nakagawa M (2003) Assessment of Takotsubo (ampulla) cardiomyopathy using 99mTc-tetrofosmin myocardial SPECT--comparison with acute coronary syndrome. Ann Nucl Med 17: 115-122.
- Martin EA, Prasad A, Rihal CS, Lerman LO, Lerman A (2010) Endothelial function and vascular response to mental stress are impaired in patients with apical ballooning syndrome. J Am Coll Cardiol 56: 1840-1846.
- Patel SM, Lerman A, Lennon RJ, Prasad A (2013) Impaired coronary microvascular reactivity in women with apical ballooning syndrome (Takotsubo/stress cardiomyopathy). Eur Heart J Acute Cardiovasc Care 2: 147-152.
- Parkkonen O, Allonen J, Vaara S, Viitasalo M, Nieminen MS, et al. (2014) Differences in ST-elevation and T-wave amplitudes do not reliably differentiate takotsubo cardiomyopathy from acute anterior myocardial infarction. J Electrocardiol 47: 692-699.
- Ogura R, Hiasa Y, Takahashi T, Yamaguchi K, Fujiwara K, et al. (2003) Specific findings of the standard 12-lead ECG in patients with 'Takotsubo' cardiomyopathy: Comparison with the findings of acute anterior myocardial infarction. Circ J 67: 687-690.
- Madias C, Fitzgibbons TP, Alsheikh-Ali AA, Bouchard JL, Kalsmith B, et al. (2011) Acquired long QT syndrome from stress cardiomyopathy is associated with ventricular arrhythmias and torsades de pointes. Heart Rhythm 8: 555-561.
- Bybee KA, Kara T, Prasad A, Lerman A, Barsness GW, et al. (2004) Systematic review: Transient left ventricular apical ballooning: A syndrome that mimics ST-segment elevation myocardial infarction. Ann Intern Med 141: 858-865.
- Prasad A, Lerman A, Rihal CS (2008) Apical ballooning syndrome (Tako-Tsubo or stress cardiomyopathy): A mimic of acute myocardial infarction. Am Heart J 155: 408-417.
- Imran TF, Rahman I, Dikdan S, Shah R, Niazi OT, et al. (2016) QT Prolongation and Clinical Outcomes in Patients with Takotsubo Cardiomyopathy. Pacing Clin Electrophysiol 39: 607-611.
- Samuelov-Kinori L, Kinori M, Kogan Y, Swartzon M, Shalev H, et al. (2009) Takotsubo cardiomyopathy and QT interval prolongation: Who are the patients at risk for torsades de pointes? J Electrocardiol 42: 353-357.
Citation: Gammon T, Finer C, Bhandare D (2020) Prolonged QTc Interval in Stress-Induced Takotsubo Cardiomyopathy. J Non Invasive Vasc Invest 5: 023.
Copyright: © 2020 Christa Finer, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

