
Psoriasiform Secondary Syphilis: A Pitfall in Diagnosis
*Corresponding Author(s):
Satiti Retno PudjiatiDepartment Of Dermatology And Venereology, Nursing And Public Health Universitas Gadjah Mada/ RSUP Dr. Sardjito Yogyakarta, Indonesia
Tel:+62 0274560700,
Email:satiti_rp@ugm.ac.id
Abstract
Secondary syphilis in Acquired Immune Deficiency Syndrome (AIDS) patient’s have variety of skin manifestations. Failure to recognize the manifestations of secondary syphilis can cause delaying the therapy. The recognition of the characteristics of skin lesions as well as serology examination and histopathology help the physicians for making the diagnosis. A 24-year-old male who was diagnosed with HIV previously came with chief complaint of scaly red plaques on the palms and soles. The similar lesions were also notedover the face especially the perioral region.Patient also noted to have also alopecia on the eyebrows and eyelashes. Patient was diagnosed with psoriasis vulgaris from previous physician and treated with unknown therapy. Serological examination revealed reactive TPHA and high titer of VDRL. Skin biopsy was done and it has features of psoriasis but without pathognomonic signs. The patient then was treated with single dose of benzathine penicillin G 2,4 million units which provided excellent improvement.Secondary syphilis is called "great imitator" because of its broad manifestations. It has been widely reported that secondary syphilis has been misdiagnosed as psoriasis and seborrheic dermatitis. Characteristics of the lesion, serological examination and histopathology play significant role in establishing the diagnosis.
Keywords
HIV; Psoriasiform syphilis; Secondary syphilis
Introduction
Syphilis is a disease caused by the spirochaete Treponema pallidum subspecies pallidum which is almost exclusively sexually transmitted [1]. It is estimated that there are 6 million new cases of syphilis per year globally in individuals aged 15-49 years [2]. The incidence of syphilis in southeast Asia and the western pacific is equal to 2,9 million cases [3]. Secondary syphilis occurs 3-12 weeks after the appearance of the primary syphilis chancre [1]. Secondary syphilis is characterized by maculopapular skin eruption, condyloma latum in the intertriginous area, lymphadenopathy with various of systemic and neurological symptoms [4]. While atypical clinical features are mimicking hypertrophic lichen planus, papularand follicular rash, vesicular rash, corymbiform rash and psoriasis [5]. Several cases of secondary syphilis mimicking psoriasis vulgaris and palmoplantar psoriasis have been reported [6-10]. Reports of several studies showed 29.6% of the cutaneous manifestations of syphilis present as atypical features and sometimes misdiagnosed as other diseases. Failed to recognize the secondary syphilis can lead to misdiagnosis and delaying the therapy. Previously, skin biopsy was rarely performed to confirm the diagnosis of secondary syphilis. However, because it can mimic other diseases, skin biopsy should be done in suspected cases especially those with HIV/AIDS [11,12].
Case Report
A 24-year-old male, came to the dermatology and venereology outpatient department in Dr. Sardjito Hospital with the chief complaint of multiple erythematous scaly plaques. Two months prior to the consultation, the patient was noted to have of erythematous patches covered with thick whitish scales on the palms and soles that spread to other body regions rapidly. The lesions were asymptomatic. The patient went to a physician, and was diagnosed with psoriasis and he was given unknown topical therapy which provided no relief. The lesions then increased in number and spreading to elbows, knees, legs and perioral area. The patient also noted have alopecia on eyebrows and eyelashes.Three weeks before consultation, patient was diagnosed with AIDS with Cluster of Differentiation (CD4) + of 41 cells/μl and started ARV (Anti Retro Viral) treatment with Fixed Drug Combination (FDC) of Tenofovir, Lamivudine, Efavirenz (THE) regimen. The patient denied prior history of genital and anal ulcer (Figure 1).
 Figure 1: Skin lesions on hands befor (a) and after (b) therapy.
Figure 1: Skin lesions on hands befor (a) and after (b) therapy.
On physical examination, patient appeared well, vital signs were within normal limits with no palpable lymph nodes. There were multiple erythematous plaques with white scales over palms and soles. The similar lesions were noted also over the cheek, perioral, chin, dorsal of extremities, elbows, knees and lower back. There were no auspitz sign, karsvlek sign and koebner phenomenon. Patient also noted to have alopecia over the eyebrows and eyelashes.
On this point, the serological examination of Treponema Pallidum Haemagglutination Assay (TPHA) was reactive and Venereal Disease Research Laboratory (VDRL) had high titer of 1:512. Skin biopsy from the lesion of right elbow showed parakeratosis and orthokeratosis with psoriasiform epidermis, spongiosis and exocytosis of lymphocytes and neutrophils. There was thinning of the suprapapillary plate with vascular dilatation in the papillae dermis. In the dermis, there is a mixed infiltrate of lymphohistiocytes, neutrophils and plasma cells, especially perivascular with of blood vessel proliferation and swollen stroma. The histopathological examination has more features of psoriasis but no munromicroabcess and kogoj spongio form pustules was found. Hence, we diagnosed this patient as a case of psoriasiform secondary syphilis (Figure 2).
 Figure 2: Skin lesions on feet before (a) and after (b) therapy.
Figure 2: Skin lesions on feet before (a) and after (b) therapy.
The patient was given was a single dose of intramuscular benzathine penicillin G 2,4 million units. Patient noted to have excellent improvement of the skin lesions during 2-week-follow up after therapy with significant decreasing of VDRL titer. The patient was scheduled to have serological evaluation 1 month after therapy, but unfortunately the patient was lost to follow up.
Discussion
Syphilis is a disease that was first recognized in Europe on 15th century. It is caused by Treponema pallidum subspecies pallidum, bacteria ranging in size from 0.15μm to 6μm-15μm, these bacteria grow slowly and cannot be cultured up to today. The course of syphilis, whether untreated or treated, can be unpredictable [13]. The disease also considered as “great imitator” because of its varied presentation and can mimic other diseases. Diagnosing syphilis can be challenging even for experienced doctors [8].
Secondary syphilis has diverse clinical findings. It can appear as maculopapular form, papulosquamous, lichenoid, condyloma lata and patchy alopecia. The distribution of the lesions is generalized, bilateral, or locally affects oral region, palms and soles. There may be generalized lymphadenopathy as well as systemic symptoms such as sore throat, malaise, headache, fever and myalgia. The skin lesions are generally non-pruritic except for the follicular variant of secondary syphilis (Figure 3).
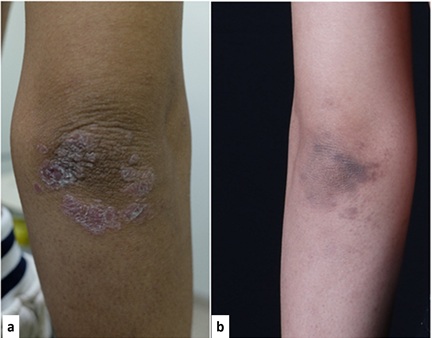 Figure 3: Skin lesion on elbow before (a) and after (b) therapy
Figure 3: Skin lesion on elbow before (a) and after (b) therapy
Secondary syphilis can manifest as loss of eyebrows and eyelashes. This condition can occur and the pathogenesis is thought to be the same as moth-eaten alopecia in syphilis patients. Without treatment, secondary syphilis lesions can either spontaneously heal without scarring, or become advanced disease like neurosyphilis and has cardiovascular complications [1,6,13,14]. In this patient, erythematous plaques with thickened white scales were found on the elbows, palms and soles, which was clinically typical in psoriasis and probably causing the misdiagnosis previously.
Skin biopsy was rarely performed in patient with secondary syphilis since there are no pathognomonic findings and this disease has broad variations of the histopathological features. Some papers said that the typical histopathologic findings of syphilis are obliterated endarteritis and dense infiltrate of plasma cells, lymphocytes, macrophages, and mononuclear leukocytes [12]. The rare histopathologic findings are psoriasiform hyperplasia, which is more frequently seen in advanced secondary syphilitic lesions. Lichenoid tissue reactions and mixed infiltrate of superficial and deep dermis is highly suggestive of syphilis [15,16]. Serological work up is the most common method used for syphilis screening, diagnosis, and treatment follow-up. In our case, TPHA was reactive with VDRL titer of 1:512, which strengthen the diagnosis of secondary syphilis (Figure 4).
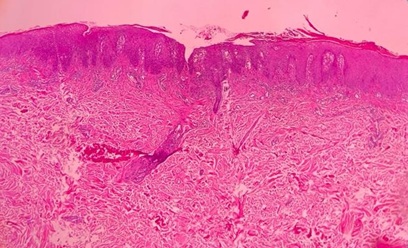 Figure 4: Histopathology result of the lesion on the right elbow.
Figure 4: Histopathology result of the lesion on the right elbow.
The treatment of choice for syphilis is intramuscular injection of benzyl benzathine penicillin-G. Treatment of primary, secondary, and early latent syphilis requires a single dose of 2.4 million units, whereas advanced latent syphilis requires a total of 7.2 million units divided by 3 doses, given every 7 days. Our patient was treated with intramuscular injection of benzyl benzathine penicillin-G (BBPG), 2.4 million units of a single dose which provided improvement of the skin lesions and decreasing of VDRL titer.
References
- Kang S; Amagai M, Bruckner AL, Enk AH, Margolis DJ, et al. (2019) Fitzpatrick’s Dermatology 9thedn. Kang S; Amagai M (ed.). Mc Graw Hill, New York, USA.
- Kojima N, Klausner JD (2018) An Update on The Global Epidemiology of Syphilis. Physiol Behav. 176: 139-148.
- Chan R (2011) Sexually transmitted infections in Asia and the Pacific - An epidemiological snapshot. Sex Transm Infect 87: 2010-2011.
- Baughn RE, Musher DM (2005) Secondary syphilitic lesions. Clin Microbiol Rev 18: 205-216.
- Ivars Lleó M, Clavo Escribano P, Menéndez Prieto B (2016) Atypical Cutaneous Manifestations in Syphilis. Actas Dermosifiliogr 107: 275-283.
- Keerthana B, Sruthy SR, Thomas J, Ravi D, Manoharan D (2017) Secondary Syphilis Masquerading Psoriasis Vulgaris-A Rare Case Report. WORLD J Pharm Med Res 3: 365-366.
- Solak B, Kara R, Erdem T (2016) Palmoplantar syphilis misdiagnosed and treated as palmoplantar psoriasis for 2 years. J Fam Med Prim Care 5: 506.
- Sahin MT, Ozturckan S, Temiz P (2018) Secondary syphilis mimicking palmoplantar psoriasis: The reemerging of “the great imitator.” J Am Acad Dermatol 79: 255.
- Gianfaldoni S, Tchernev G, Wollina U, Gianfaldoni R, Lotti T (2017) Secondary syphilis presenting as palmoplantar psoriasis. Open Access Maced J Med Sci 5: 445-447.
- Peng RR, Shang S, Chen J, Shi M, Long FQ (2019) Delayed onset and protracted course of psoriasis-like secondary syphilitic lesions in a HIV-seropositive man who has sex with men: A case report. Acta Derm Venereol 99: 1197-1198.
- McMillan A, McQueen A, McLaren C (1996) A histopathological study of secondary syphilis. J Eur Acad Dermatology Venereol 7: 235-239.
- Rotaru M, Iancu G (2016) Diagnostic Difficulties in Secondary SyphilisAssociated With Psoriasis Vulgaris -Clinical Case. Dermatovenerologia.
- Ghanem KG, Ram S, Rice PA (2020) The modern epidemic of syphilis. N Engl J Med 382: 845-854.
- Hook EW (2017) Syphilis. Lancet 389: 1550-1557.
- Patterson JW (2016) Weedon’s Skin Pathology (4th edn). Patterson JW (ed.). Elsevier, Charlottesville, USA.
- Balagula Y, Mattei PL, Wisco OJ, Erdag G, Chien AL (2014) The great imitator revisited: The spectrum of atypical cutaneous manifestations of secondary syphilis. Int J Dermatol 53: 1434-1441.
Citation: Pudjiati SR, Valentine AT, Kurniawati C, Trisnowati N (2020) Psoriasiform Secondary Syphilis: A Pitfall in Diagnosis. J Clin Dermatol Ther 6: 066.
Copyright: © 2021 Satiti Retno Pudjiati, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

