
Psoriasis and Covid-19: A Precise Survey and Meta Analysis
*Corresponding Author(s):
Yeyen Jani Sari DabukkeDepartment Of Medicine, University Of Methodist, Indonesia
Email:dabukkeyeyen23@yahoo.com
Abstract
Introduction: Psoriasis influences around 2% of the grown-up populace. Systemic treatments for direct to serious psoriasis have been connected to an expanded chance of upper respiratory viral tract disease. It is undetermined in the event that having psoriasis itself, having co morbidities related with psoriasis, or efficient medications for psoriasis clarify this relationship with COVID-19.
Method: This precise survey incorporates looking the Google Scholar, PubMed and Web of Science databases utilizing the catchphrases psoriasis, coronavirus and COVID-19. The look was supplemented by manual looking of reference records of included articles. The look was upgraded in December 2019.
Result: the current writing may give a few clues for security contemplations. Ordinary immunosuppressive treatments such as methotrexate and cyclosporine, and anti-tumor corruption calculate specialists ought to not be favored due to expanded hazard of contamination, particularly in high-risk regions. The utilize of cyclosporine may posture extra hazard due to the side impact of hypertension, which has been detailed to be related with defenselessness to serious COVID-19.
Conclusion: the current writing has given no conclusive prove that biologics increment the chance of COVID-19, withdrawal of these operators ought to be saved for patients with COVID-19 side effects. The treatment approach ought to be personalized, considering the points of interest and drawbacks for each case independently.
Keywords
Coronavirus; COVID-19; Psoriasis
Introduction
Agreeing to the World Health Organization (WHO), a unused sort of coronavirus called extreme intense respiratory disorder coronavirus-2 (SARS-CoV-2), causing viral pneumonia, was distinguished in Wuhan, China, in December 2019 with Coronavirus infection 2019 (COVID-19) contamination [1], the WHO articulated on 11 Walk 2020 that this worldwide plague was a widespread; this was moreover the date upon which the primary case of COVID-19 disease in Turkey was detailed by the Service of Health [2,3]. Agreeing to the WHO’s definition of COVID-19, all PCR-positive patients were acknowledged as affirmed COVID-19.
Psoriasis may be a common unremitting provocative skin infection related with noteworthy dismalness amplifying past the cutaneous manifestations. The infection influences around 2% to 3% of the populace worldwide, and its administration requires qualified experts to supply high-quality care. Corona virus illness (COVID-19) could be a exceedingly infectious respiratory disease caused by serious intense respiratory disorder coronavirus 2 (SARS-CoV-2). COVID-19 episode, which caused thousands of passings, has been pronounced a widespread by the World Health Organization on Walk 2020 [4]. The widespread has been detailed to alter the course of numerous maladies, and psoriasis isn't absolved from the affect of the outbreak [5,6].
Psoriasis may be a unremitting provocative malady with a around the world recurrence of around 2% to 3%. Elderly psoriasis patients and/or patients utilizing ordinary immunosuppressive regimens and biologic specialists are at higher chance for irresistible maladies. But despite some reports around psoriasis and COVID-19, there's instability concerning results of disease in patients with psoriasis or those treated with immunosuppressive therapies [6,7]. The auxiliary point was to assess clinical characteristics of psoriasis patients with COVID-19 and compare rates for patients who gotten or did not get immunosuppressive or organic treatments.
Methods
This study using systematic review and meta analysis that search using keyword psoriasis, coronavirus and COVID-19 in Google Scholar, PubMed and Web of Science. After final screening the author analysize 3 articles (Figure 1). The summarize of the articles are in table 1.
|
Author |
Origin |
Method |
Method |
Result |
Outcome |
|
Ozaras R |
Infection |
Case rep |
2020 |
Psoriasis is an immune-mediated |
Covid-19 patients may show highlights of |
|
Ömer Kutlu |
Department of |
Case repo |
2020 |
A 71-year-old lady with no |
The worsening of psoriasis in this
|
|
Ayse |
Department of |
Literature Review |
2020 |
Immunosuppressive and |
The disease dangers postured by the |
Table 1: Summarize Association Psoriasis and Covid-19.
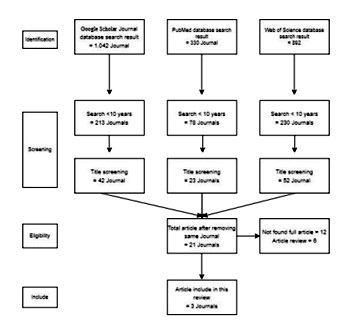 Figure 1: Flow Chart for Screening Systematic Review.
Figure 1: Flow Chart for Screening Systematic Review.
The Affect of Widespread on the Course of Psoriasi
The COVID-19 wide spread has modified the approach to all patients requiring near contact amid a visit, counting dermatologic meetings. The healthcare framework was overpowered in numerous nations, and numerous centers may not adapt with the tremendous number of patients. Patients with psoriasis were not excluded from this circumstance and had as it were restricted get to to required healthcare settings in numerous nations. Numerous centers were able to preserve planned medications for as it were chosen patients [3].
Constrained accessibility of dermatology care administrations caused worsening of preexisting cases of psoriasis, whereas unused cases fizzled to be analyzed. “Stay at home” orders issued by numerous specialists to constrain the spread of the disease were another reason for less patients applying for outpatient.
Enthusiastic stretch is another figure that will act as a catalyst for the onset and exacerbation of psoriasis [8]. Kutlu and Metin proposed that the burden of push incited by the COVID-19 widespread might raise the number of psoriasis cases requesting dermatology visits [9]. A later web-based think about exploring the affiliation of open air movement limitatio and wage misfortune with patientreported results of psoriasis amid the COVID- 19 widespread appeared that 43.7% of 926 patients depicted moderate-to-much declining of psoriasis. Open air action confinement was found to be emphatically related with the compounding of psoriasis, stretch, and uneasiness and discouragement. Moreover, misfortune was related with the compounding of psoriasis, stretch, and uneasiness and depression [10]. Maximizing the psychosocial bolster accessible to patients with psoriasis amid the widespread may play a critical part in controlling malady movement.
Patients with COVID-19 may appear characteristics of hyper inflammation caused by the overproduction of cytokines. Biomarkers of irritation such as C-reactive protein and ferritin have been found essentially lifted in patients with COVID- 19 [11]. Given the vital part of aggravation within the pathogenesis of psoriasis, it can be proposed that hyperinflammation status caused by COVID-19 may moreover change the course of psoriasis. In their arrangement of 52 patients, Kutlu and Metin found that 9.6% of patients with COVID-19 who were already conceded to the dermatology outpatient clinic had psoriasis. They concluded that patients with psoriasis may be more powerless to COVID-19.9 Ozaras et al detailed a case of psoriasis declined conceivably due to COVID 19. The creators suggested that hyperinflammation status created by COVID 19 itself might compound psoriasis [12-20].
Management Therapy of Psoriasis within the Period of COVID-19
Acitretin has anti-inflammatory properties and restrains cell separation without immunosuppressive impacts. In their cohort consider, Dommasch, et al. found that patients with psoriasis on acitretin treatment appeared no expanded chance of viral or respiratory infection [20]. Caselli, et al appeared that retinoids may have antiviral impacts on human herpes virus [21]. The impacts of retinoids on SARS-Cov-2 stay obscure. In spite of the fact that acitretin has not been demonstrated secure in patients with COVID- 19, it can be favored amid the widespread since it have no immunosuppressive impacts.
Both methotrexate and cyclosporine are related with an expanded chance of contamination. The generally recurrence of contracting pneumonia in patients with psoriasis utilizing methotrexate has been detailed to be 0.8% [22]. Cyclosporine as it were somewhat increments the hazard of respiratory tract diseases. Be that as it may, the most antagonistic impacts of cyclosporine, such as hypertension and renal brokenness, may posture more serious dangers for patients contracted COVID-19. It ought to be famous that patients with hypertension are more inclined to create extreme COVID-19 infection [23]. Suddenly, Wilde detailed that cyclosporine unequivocally represses in vitro replication of MERS- coronavirus, whereas its in vivo impacts stay unknown [24].
In spite of the affect of these immunosuppressive operators on the course of COVID-19 is clearly obscure, a few dermatology social orders have suggested to pulled back or suspend immunosuppressive medicines within the case of COVID-19 conclusion until the understanding recuperates from the disease. In any case, the choice has been cleared out to the participation between the persistent and doctor in charge, considering the advantages/ disadvantages for each case separately [25, 26].
Psoriasis and Anti-IL Therapies
Biologics repress immune-mediated pathways counting unmistakable cytokines. In this manner, they may posture a conceivable hazard of upgraded affectability to contaminations. In any case, there's no clear prove supporting the withdrawal of biologics for most patients with psoriasis due to the hazard of disease. A few creators have not prescribed the withdrawal of tumor corruption figure alpha (TNFα) inhibitors and anti-IL biologics due to “likely moderate risk” within the case of gentle viral symptoms [27]. Other creators have proposed shirking of TNFα inhibitors for patients with cutaneous illnesses in locales with tall disease rates and cessation of all natural specialists within the case of presentation to COVID-19 cases [28]. In any case, whether cessation of immunomodulatory medications may improve the chance of cytokine storm is remained obscure.
A few thinks about detailed comparable dangers of contaminations in patients with psoriasis getting biologic operators. In a consider exploring the hazard of genuine contamination in patients with psoriasis getting biologics, the most noteworthy hazard has been detailed for infliximab. The creators found no noteworthy increments within the chance of genuine disease for etanercept, adalimumab, or ustekinumab compared with nonbiologic systemic treatments or methotrexate only [29]. Another ponder has appeared no noteworthy contrast between the biologics and other systemic treatments in terms of the chance of genuine infection [30].
In a later think about, counting 515 patients with psoriasis on biologics, psoriasis declined in 9 of the 27 (33.3%) patients who cleared out their medicines. None of the 488 patients who survive treatment portrayed any COVID- 19-related side effects, supporting the security of biologic operators in patients with psoriasis [31]. In a cross-sectional, questionnaire-based think about, the creators found that COVID-19 information avoids biologics cessation. The creators concluded that dermatologists ought to educate their patients around COVID-19 to maintain a strategic distance from their misfortune of compliance [32].
In a multicenter consider, the creators detailed that 23 patients with psoriasis on biologics had COVID-19 side effects but they did not halt treatment. The creators did not watch a more extreme course of suspected COVID-19 signs in patients who kept up treatment [33]. In their case arrangement counting four COVID-19 patients with psoriasis on natural drugs, the creators found that as it were one understanding, who was on guselkumab, shown a extreme shape of COVID-19. Another quiet, who was on IL-12/23 inhibitor ustekinumab, appeared as it were gentle indications. The other two cases did not appear any indications. The creators concluded that natural drugs may play a defensive work against the onset and the course of the infection [34]. On the other hand, Benhadeu, et al. detailed advancement of COVID-19 side effects taking after guselkumab infusion in a quiet with psoriasis [35].
Messina, et al. moreover detailed a case of COVID-19 in a understanding with psoriasis on IL-23 inhibitor guselkumab. The understanding appeared as it were gentle side effects and the creators concluded that IL-23/IL-17 pathway restraint may not be pernicious within the setting of COVID-19 infection [36]. Balestri, et al. detailed a understanding who was contaminated amid the acceptance regimen of IL-17 inhibitor ixekizumab. The quiet was tried positive for SARS-CoV-2 taking after contact with a COVID-positive persistent. The persistent was totally asymptomatic, in spite of the fact that he proceeded the treatment as already scheduled [37]. Considering that the impedances of IL-17/23 pathway may have useful results in COVID-19, ixekizumab is being explored for the treatment of COVID-19 infection [36].
In a expansive cohort consider counting 1193 patients with psoriasis on biologics and little particles, the creators found that patients on biologics were at a more noteworthy chance to test positive for COVID-19 and to be hospitalized. In any case, they detailed no expanded hazard of seriously care unit affirmation or death [38]. In a review multicenter think about counting 206 patients with psoriasis on biologics, the creators found no noteworthy number of hospitalizations or passings from COVID- 19 [39]. In another review think about, counting 980 patients with psoriasis on biologics, the creators have found no early flag of an expanded hospitalization or passing from COVID-19 [40]. At long last, in a phone consultation-based think about counting 168 patients with psoriasis on biologics, the creators did not watch a tall recurrence of COVID-19 or related symptoms [41].
review multicenter think about counting 206 patients with psoriasis on biologics, the creators found no noteworthy number of hospitalizations or passings from COVID- 19 [39]. In another review think about, counting 980 patients with psoriasis on biologics, the creators have found no early flag of an expanded hospitalization or passing from COVID-19 [40]. At long last, in a phone consultation-based think about counting 168 patients with psoriasis on biologics, the creators did not watch a tall recurrence of COVID-19 or related symptoms [41].
Conclusion
The COVID 19 widespread has contrarily influenced the administration of numerous illne sses, and psoriasis isn't absolved from this circumstance. Patients' failure to get to satisfactory healthcare administrations and pus h burden caused exacerbations in psoriasis cases. We accept that it is fundamental to closely screen patients with psoriasis and give elective healthcare apparatuses, such as phone interviews and teledermatology, when fundamental. Giving psychosocial bolster to the patients and their families may moreover have useful impacts in controlling the malady movement. The author suggests that classical immunosuppressive operators such as methotrexate, cyclosporine, and TNFα inhibitors ought to be dodged particularly in high-risk regions. Considering that ponder has given no conclusive prove that biologics increment the hazard of COVID-19, withdrawal of these specialists ought to be saved for patients with COVID-19 indications. The conclusion between psoriasis and COVID- 19 in table 1.
Conflicts of Interests
The author declares no conflict of interest. The funding sponsors had no role in the writing of the manuscript and in the decision to publish it.
References
- Kizilyel O, Akdeniz N, Metin MS, Elmas OF (2019) Investigation of oxidant and antioxidant levels in patients with psoriasis. Turk J Med Sci 49: 1085-1088.
- Gran F, Kerstan A, Serfling E, Goebeler M, Muhammad K (2020) Current developments in the immunology of psoriasis. Yale J Biol Med 93: 97- 110.
- Atzori L, Mugheddu C, Addis G, Sanna S, Satta R, et al. (2020) Psoriasis health care in the time of the coronavirus pandemic: insights from dedicated centers in Sardinia (Italy). J Eur Acad Dermatol Venereol 34: 247-248.
- WHO (2020) Naming the coronavirus disease (covid-19) and the virus that causes it. Geneva, Switzerland.
- Wu Z, McGoogan JM (2020) Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA 323: 1239- 1242.
- Abdelmaksoud A, Goldust M, Vestita M (2020) COVID-19 and psoriasis: Is it time to limit treatment with immunosuppressants? A call for action. Dermatol Ther 33: 13298.
- Ebrahimi A, Sayad B, Rahimi Z (2020) COVID-19 and psoriasis: biologic treatment and challenges. J Dermatolog Treat Page no: 1- 5.
- Sathyanarayana Rao TS, Basavaraj KH, Das K (2013) Psychosomatic paradigms in psoriasis: psoriasis, stress and mental health. Indian J Psychiatry 55: 313-315.
- Kutlu Ö, Metin A (2020) Dermatological diseases presented before COVID-19: are patients with psoriasis and superficial fungal infections more vulnerable to the COVID-19? Dermatol Ther 33: 13509.
- Kuang Y, Shen M, Wang Q, Xiao Y, Lv C, et al. (2020) Association of outdoor activity restriction and income loss with patient-reported outcomes of psoriasis during the COVID-19 pandemic: a web-based survey. J Am Acad Dermatol 83: 670-672.
- Henry BM, de Oliveira MHS, Benoit S, Plebani M, Lippi G (202) Hematologic, biochemical and immune biomarker abnormalities associated with severe illness and mortality in coronavirus disease 2019 (COVID-19): A meta-analysis. Clin Chem Lab Med 58: 1021- 1028.
- Ozaras R, Berk A, Ucar DH, Duman H, Kaya F, et al. (2020) Covid-19 and exacerbation of psoriasis. Dermatol Ther Page no: 13632.
- Balak DM, Hajdarbegovic E (2017) Drug-induced psoriasis: clinical perspectives. Psoriasis (Auckl) 7: 87- 94.
- FDA (2020) US Food and Drug Administration.
- Said A, Bock S, Lajqi T, Muller G, Weindl G (2014) Chloroquine promotes IL-17 production by CD4+ T cells via p38-dependent IL-23 release by monocyte-derived Langerhans-like cells. J Immunol 193: 6135- 6143.
- Sachdeva M, Mufti A, Maliyar K, Lytvyn Y, Yeung J (2020) Hydroxychloroquine effects on psoriasis: a systematic review and a cautionary note for COVID-19 treatment. J Am Acad Dermatol 83: 579-586.
- Megarbane B, Scherrmann JM (2020) Hydroxychloroquine and azithromycin to treat patients with COVID-19: both friends and foes? J Clin Pharmacol 60: 808- 814.
- Saxena VN, Dogra J (2010) Long-term oral azithromycin in chronic plaque psoriasis: a controlled trial. Eur J Dermatol 20: 329- 333.
- Huang SW, Chen YJ, Wang ST, Ho L-W, Kao J-K, et al. (2016) Azithromycin impairs TLR7 signaling in dendritic cells and improves the severity of imiquimod-induced psoriasis-like skin inflammation in mice. J Dermatol Sci 84: 59- 70.
- Dommasch ED, Kim SC, Lee MP, Gagne JJ (2019) Risk of serious infection in patients receiving systemic medications for the treatment of psoriasis. JAMA Dermatol 155: 1142.
- Caselli E, Galvan M, Santoni F, Alvarez S, de Lera AR, et al. (2008) Retinoic acid analogues inhibit human herpesvirus 8 replication. Antivir Ther 13: 199- 209.
- West J, Ogston S, Foerster J (2016) Safety and efficacy of methotrexate in psoriasis: a meta- analysis of published trials. PLoS One 11: 0153740.
- Karadag AS, Aslan Kayiran M, Lotti T, Wollina U (2020) Immunosuppressive and immunomodulator therapy for rare or uncommon skin disorders in pandemic days. Dermatol Ther 33: 13686.
- de Wilde AH, Raj VS, Oudshoorn D, Bestebroer TM, van Nieuwkoop S, et al. (2013) MERS-coronavirus replication induces severe in vitro cytopathology and is strongly inhibited by cyclosporin A or interferon-α treatment. J Gen Virol 94: 1749- 1760.
- American Academy of Dermatology Association (2020) Managing your practice through the COVID-19 outbreak.
- International Psoriasis Council (2020) Statement on the coronavirus (COVID-19) outbreak.. Accessed 27. Price KN, Frew JW, Hsiao JL, Shi VY (2020) COVID-19 and immunomodulator/immunosuppressant use in dermatology. J Am Acad Dermatol 82: 173- 175.
- Conforti C, Giuffrida R, Dianzani C, Di Meo N, Zalaudek I (2020) COVID-19 and psoriasis: is it time to limit treatment with immunosuppressants? A call for action. Dermatol Ther Page no: 13298.
- Yiu ZZN, Smith CH, Ashcroft DM, Lunt M, Walton S, et al (2018) Risk of serious infection in patients with psoriasis receiving biologic therapies: a prospective cohort study from the British Association of Dermatologists Biologic Interventions Register (BADBIR). J Invest Dermatol 138: 534- 541.
- Kalb RE, Fiorentino DF, Lebwohl MG, Toole J, Poulin Y, et al. (2015) Risk of serious infection with biologic and systemic treatment of psoriasis: results from the Psoriasis Longitudinal Assessment and Registry (PSOLAR). JAMA Dermatol 151: 961- 969.
- Burlando M, Carmisciano L, Cozzani E, Parodi A (2020) A survey of psoriasis patients on biologics during COVID-19: a single Centre experience. J Dermatolog Treat.
- Bragazzi NL, Riccò M, Pacifico A, Malagoli P, Kridin K, et al. (2020) COVID-19 knowledge prevents biologics discontinuation: Data from an Italian multicenter survey during RED-ZONE declaration. Dermatol Ther 33: 13508.
- Carugno A, Gambini DM, Raponi F, Vezzoli P, et al. (2020) COVID-19 and biologics for psoriasis: a high-epidemic area experience - Bergamo, Lombardy, Italy. J Am Acad Dermatol 83: 292- 294.
- Conti A, Lasagni C, Bigi L, Pellacani G (2020) Evolution of COVID-19 infection in 4 psoriatic patients treated with biological drugs. J Eur Acad Dermatol Venereol 34: 360-361.
- Benhadou F, Del Marmol V (2020) Improvement of SARS-CoV2 symptoms following Guselkumab injection in a psoriatic patient. J Eur Acad Dermatol Venereol 34: 363-364.
- Messina F, Piaserico S (2020) SARS-CoV-2 infection in a psoriatic patient treated with IL-23 inhibitor. J Eur Acad Dermatol Venereol 34: 254-255.
- Balestri R, Rech G, Girardelli CR (2020) SARS- CoV-2 infection in a psoriatic patient treated with IL-17 inhibitor. J Eur Acad Dermatol Venereol 34: 357-358.
- Damiani G, Pacifico A, Bragazzi NL, Malagoli P (2020) Biologics increase the risk of infection and hospitalization, but not ICU admission and death: real-life data from a large cohort during red-zone declaration. Dermatol Ther Page no: 13475.
- Gisondi P, Facheris P, Dapavo P, Piaserico S, Conti A, et al. (2020) The impact of COVID-19 pandemic on patients with chronic plaque psoriasis being treated with biologic therapy: the northern Italy experience. Br J Dermatol 183: 373-374.
- Gisondi P, Zaza G, Del Giglio M, Rossi M, Iacono V, et al. (2020) Risk of hospitalization and death from COVID-19 infection in patients with chronic plaque psoriasis receiving a biologic treatment and renal transplant recipients in maintenance immunosuppressive treatment. J Am Acad Dermatol 83: 285-287.
- Megna M, Ruggiero A, Marasca C, Fabbrocini G (2020) Biologics for psoriasis patients in the COVID-19 era: more evidence, less fears. J Dermatolog Treat 31: 328-329.
- Megna M, Napolitano M, Patruno C, Fabbrocini G (2020) Biologics for psoriasis in COVID-19 era: what do we know? Dermatol Ther 33: 13467.
Citation: Dabukke YJS (2022) Psoriasis and Covid-19: A Precise Survey and Meta Analysis. J Clin Dermatol Ther 8: 095.
Copyright: © 2022 Yeyen Jani Sari Dabukke, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

