
Psychological State and Threatened Preterm Delivery- The Impact of Progesterone Therapy
*Corresponding Author(s):
Elena DakovicUniversity Clinic For Gynecology And Obstetrics Narodni Front, Belgrade, Serbia
Tel:+381 652916793,
Email:djakovicelena7@gmail.com
Abstract
Background: The individual psychological status is another risk factor in threatened preterm delivery.
Aims: To determine how depression, anxiety, and stress influence pregnancy outcome and condition of the newborn, and the impact of progesterone therapy on pregnant woman’s psychological status in threatened preterm delivery.
Methods: Forty-one pregnant women with the signs of threatened preterm birth and forty controls during their third trimester filled out three questionnaires: the socio-economic survey, the Depression, Anxiety and Stress Scale (DASS) and the Edinburgh Postnatal Depression Scale (EPDS). Five days after the introduction of progesterone therapy the study group filled the DASS and EPDS again. The outcomes were the gestational week at delivery, birth weight of the neonate and admission to the neonatal intensive care unit.
Results: Higher scores on DASS and EPDS predicted a delivery in earlier gestational weeks. High anxiety scores during pregnancy were associated with lower birth weight of the neonates. Pregnant women with high anxiety and stress scores more often delivered neonates who were admitted to the intensive care unit. The values of scores on the DASS and EPDS were significantly lower on the fifth day after the introduction of progesterone therapy.
Conclusion: The symptoms of depression, anxiety, and stress are associated with preterm delivery, newborns’ lower birth weight and admission to the intensive care unit. The introduction of progesterone therapy can postpone preterm delivery by positively influencing the psychological status of a pregnant woman.
Keywords
Anxiety; DASS; Depression; EPDS; Preterm delivery; Stress
INTRODUCTION
At the beginning of the twenty-first century we are still faced with the enigma of preterm delivery, which incidence is not reduced. Moreover, it is in a slight increase because of the introduction of assisted reproductive technologies and a higher prevalence of multiple gestations [1]. Imminent preterm delivery represents the activation of the labor process between the 20th and 37th weeks of gestation when the fetus weighs between 500 to 2500g and it has not reached maturity. Several risk factors may initiate preterm labor and delivery. Previous preterm birth, twins or higher-order pregnancies, and certain anomalies of the reproductive organs are 6-8 times more predisposed for preterm birth. In population groups with low socioeconomic status, the Relative Risk (RR) is three times higher. Other minor preterm labor risk factors (such as malnutrition, age under 17 or over 40 years, hard physical work, pyelonephritis, bacterial vaginosis, recurrent miscarriages, smoking and anemia) can compound and, in that way, increase the RR [2]. However, one-third of all cases of preterm birth are still not determined. The psychological state of pregnant women is a growing field of preterm delivery investigation. The main focus is the possible influence of traumatic events, birth outcomes and the postpartum period of previous pregnancies. Today, it is known that depression, anxiety and stress during pregnancy are very important factors associated with preterm labor. Depression is a mental disorder, characterized by depressed mood, loss of interest or pleasure, guilt with low self-esteem, insomnia, loss of appetite and lack of energy and poor concentration. The depression occurs in women with equal frequency during and beyond the pregnancy, but 14.5% of women have their first episode of depression during pregnancy [3]. Recent articles report a high percentage of postnatal paternal depression (28%) that negatively affects early father-child interactions. Counseling and psychotherapy before birth could prepare future parents for this demanding role [4]. Serbian authors compared depressive symptoms during pregnancy and postpartum.
In high-risk pregnancies, there was a threefold increase in the incidence of postpartum depression. Women who had had antenatal depressive symptoms were at a 10-fold risk of developing postpartum depression [5]. Anxiety is a condition characterized by a sense of inner restlessness, timidity, fear that something terrible has happened and the presence of psychosomatic tension. Anxiety has long been considered an important cause of preterm delivery and low birth weight [6]. Also, studies confirm that a high level of anxiety during pregnancy frequently affects the commencement of prenatal and postpartum depression [7]. Stress is defined as a physiological, emotional or behavioral response to a threatening situation. Acute and chronic stress (distress) increase cortisol levels and reduce blood flow to the uterus. The resulting hypo-oxygenation slows fetal growth and increases uterine irritability leading to contractions [8]. Additionally, based on “fetal origins hypothesis” prenatal environmental exposures that include a maternal psychological state (depression, anxiety and stress) can have sustained effects on fetal behavior and child development at the biochemical level [9]. Linkage of progesterone treatment and postpartum depression is controversial. Hilgers and associates showed the results according to which the intensity of all postpartum depressive symptoms decreased after treatment with natural progesterone [10]. Contrary, in women on contraceptive progesterone (synthetic progesterone derivatives) during the lactation period, Relative Risk (RR) for the occurrence of postpartum depression was 2.56 compared to placebo [11]. The authors of this article focused on the third trimester of pregnancy and psychological symptoms in preterm labor. Study aims were to determine: are the symptoms of depression, anxiety, and stress associated with preterm delivery, and a possible linkage of progesterone therapy with score changes on the Scale of Depression, Anxiety and Stress (DASS) and the Edinburgh Scale of Postnatal Depression (EPDS) in preterm delivery.
STUDY METHODOLOGY
The duration of this prospective study was eighteen months - from January 2015 till June 2016. Forty-one cases and forty controls included pregnant women in their third trimester (after the 28th gestational week). The Ethical Committee at the Faculty of Medicine, University of Belgrade had approved, and all the participants signed a document of informed consent. The information collection was from the patients’ records, with the clinic’s management permission. The exclusion criteria were: participants under the age of 18; unfamiliar with Serbian language and writing; patients with a history of psychiatric illness; drug, alcohol, and illegal substances abuse; positive cervical and vaginal swabs; values of C - reactive protein over 10U/L and anemia with hemoglobin levels under 80g/L. The study group was admitted to our clinic with the diagnosis of preterm labor - more than four contractions during 20 minutes, cervical shortening less than 25mm (measured by vaginal ultrasound) and/or uterine bleeding. There were no cases of PPROM (Premature Preterm Rupture of Membranes). The most important inclusion criterion was the absence of intrauterine infection, proved by microbiological and laboratory analyses. Participants of the control group had no clinical signs of preterm labor. They were admitted for a regular checkup due to gestational diabetes and/or hypertension. This was a case-control study for three independent variables: body mass index, age and satisfaction with health care during pregnancy. The association between psychological symptoms and preterm labor was tested only in the study group. At admittance, in both groups, the personal history and socioeconomic interview covered: age, height, and weight before pregnancy (to calculate the body mass index -BMI), satisfaction with family and state support for pregnant women, as well as data about the course of previous pregnancies [12]. The obstetric examination included palpation and microbiological swabs of the cervix and vagina. Ultrasound examination confirmed the gestational age, fetal number (single or twin pregnancy) and growth, Doppler measurements in umbilical and uterine vessels, position and maturity of the placenta and amniotic fluid index. At admittance, all the participants also completed two psychometric tests: the DASS and the EPDS [13,14]. The authors came to the idea to use two parallel tests because EPDS did not describe somatic changes that are common during the third trimester of pregnancy (difficulty to relax, difficulty in swallowing and dyspepsia, sense of heart rate increase, “heart missing a beat", sweating, etc.,). These symptoms often overlap psychological disorders and mask the onset of depression during the third trimester (between 28th and 37th week of gestation).
In the study group contractions were stopped by acute intravenous tocolysis - fenoterol 2 ampules of 5 mg and verapamil 1 ampule of 40 mg in 500 ml of 0.9% saline solution - slow intravenous infusion for 24 hours. The next day (Day 1) we administered two forms of systemic progesterone: one dose (250 mg) depot intramuscular injection of 17 α-OH progesterone caproate, followed by oral micronized progesterone (P4) - ovule of 200 mg, two or three times a day, depending on the frequency and intensity of the contractions, measured by Cardiotocography (CTG). The depot - progesterone administration and psychometric tests were repeated as above mentioned (DASS and EPDS) on the fifth day (Day 5) in the study group. The following outcomes were observed: whether the delivery was preterm or at term, mode of delivery, fetal weight at birth and the admission to the neonatal intensive care unit. Psychological assessment instruments: DASS contains 42 questions divided into three groups (14 each) about the symptoms of depression, anxiety and stress. This questionnaire wasn’t previously used in Serbia. The authors got it from Mr. Zoran Protulipac Psych, MAPS, who kindly translated it to Serbian from the original English version developed in Australia.
Participants evaluate their symptoms during the past seven days on the symptoms intensity scale (Likert Scale: from 0, 1, 2 or 3 which indicated how much the statement applied to the patient - 0 - did not apply at all; 1- applied to some degree or some of the time; 2- applied to a considerable degree or a good part of the time; 3 - applied very much or most of the time). Depression is present if the score is higher than 28, more than 20 points confirm anxiety and score that is higher than 34 confirms the presence of severe stress [13]. The original EPDS was developed by Cox, Holden and Sagowsky as a screening instrument for postnatal depression. The EPDS contains ten statements specific to depressive symptoms. Each item has four possible responses, which are scored from 0 to 3, and the period estimated is seven days. A total score of the scale could be from 0 to 30, where the cut-off value of 13 and above indicates a high level of depression symptoms. Scores of 10-12 indicate a moderate level of depression symptoms [14]. The EPDS was translated to the Serbian language and validated in 2015. It showed good internal consistency in evaluating both, prenatal and postpartum depressive symptoms. The psychometric properties of this translated version are the same as the original English version [15]. Using descriptive and analytical methods we determined Body Mass Index (BMI), age, depression, anxiety and stress as risk factors (independent variables). Data are expressed as the mean ± standard deviation for continuous variables or as percentages where appropriate. The significance of risk factors impact on the main outcomes: week of delivery, birth weight of the neonate and the admission to Neonatal Intensive Care Unit (NICU) were tested by Chi-square test or t-test (one sample- the study group before and after progesterone therapy). Correlation tests were applied in assessing the correlation between exposure to risk factors and the outcomes. Using a two-tailed alpha probability (p) <0.05 were considered significant.
All statistical analyses were carried out using the Statistical Package for the Social Sciences (SPSS) 20.0 software (SPSS Inc., Chicago, IL, USA). In all applied analytical methods the level of significance was 0.05 while the power of the tests estimated at 80%.
RESULTS
We examined eighty-one female patients (41 cases and 40 controls); the average age was 34.5 years (Median 34.0; SD 5.2). The youngest woman was 19 and the oldest 44 years old. The average age was 35.1 in the study group and 32.7 years in controls and this difference was statistically significant (t = 2.035; p <0.05). Patients of the study group were hospitalized between the 28th and 37th week, the average gestation was 32 weeks (Table 1). Although the values of BMI didn’t significantly differ between groups (p =0.797), the participants with higher BMI before pregnancy gave birth to children with birth weight below 2500 grams and this difference was statistically significant (Figure 1). The satisfaction with social support (rating of good, very good and excellent) was 70.0%. The participants of the study group were more satisfied than controls (82.9% and 72.5%) and this difference was statistically significant (χ2 = 16.114; p < 0.01) (Figure 2). There was no statistically significant difference between the study and control group in the scores of depression, anxiety, stress and EPDS on admission (t was less than 1.96 and p greater than 0.05 in all cases). The analysis of the scores after 5 days was not performed in the controls since we did not administer progesterone therapy to them. Patients of the study group were analyzed by obstetric indications for admission to a high - risk pregnancy ward- twenty-six (63.4%) had isolated diagnosis of preterm labor while the remaining 15 (36.6%) had additional risk factors: preeclampsia (7.3%), preceding placenta (7.3%) and fetal intrauterine growth restriction (9.8%). There were also five participants with twin pregnancies (12.2%). These additional risk factors indicated a Cesarean section in 25 (61.0%) cases, while 16 (39.0%) delivered vaginally. Thirty-one participants (75.6%) of the case group delivered prematurely, of which 25 (80.6%) by Cesarean section and 6 (19.4%) vaginally; mean of the week at delivery was 33.6 (SD 2.5). Ten of the cases (24.4%) had a term delivery. There were no preterm deliveries in the control group. Five neonates in the study group were of very low birth weight (below 1500 g), eighteen (43.9%) were between 1500 and 2500 g and eighteen over 2500 g. Higher values of anxiety on the 5th day after the introduction of progesterone therapy resulted in having neonates of lower birth weight (Figure 3). Twenty-one premature neonates (67.7%) were admitted to NICU (Table 2a). In these cases, there were higher anxiety and stress scores measured on Day 5 (Table 2b). On admission, we observed a significant correlation of BMI with the age and the scores of anxiety, depression and EPDS. Pregnant women with a higher BMI were older and had higher scores of anxiety, depression, and EPDS in both groups (Table 3). Anxiety and stress scores on the 5th day after introducing progesterone therapy were in a negative correlation with the gestational week at the time of delivery (Figures 4 and 5). The authors confirmed the association of all three psychological risk factors with preterm labor and delivery. In the study group, there was a significant decrease in both, DASS (depression and anxiety) and EPDS scores on the fifth day of progesterone therapy. The most significant decrease in scores was registered on the EPDS (Figure 6).
1a.
|
Group |
N |
Mean |
Std. Deviation |
Std. Error Mean |
|
|
BMI
|
study |
41 |
23.090 |
3.0198 |
0.4716 |
|
control |
40 |
22.893 |
3.8443 |
0.6078 |
|
|
Gestanional week |
study |
41 |
31.961 |
2.5646 |
0.4005 |
|
control |
40 |
33.137 |
2.3962 |
0.3789 |
|
|
Age
|
study |
41 |
35.171 |
4.5547 |
0.7113 |
|
control |
40 |
32.725 |
6.1602 |
0.974 |
|
1b.
|
Independent Samples T test |
|||
|
|
t |
df |
p |
|
BMI
|
0.258 |
79 |
0.797 |
|
Gestational week
|
-2.132 |
79 |
0.036 |
|
Age
|
2.035 |
79 |
0.045 |
Table 1: Significance of difference in BMI, gestational week and age between groups.
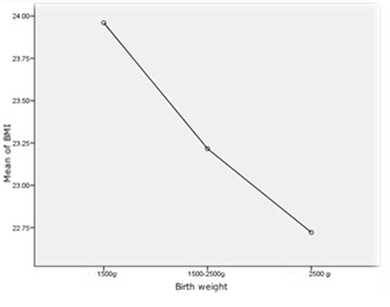 Figure 1: The association of BMI with birth weight in both groups.
Figure 1: The association of BMI with birth weight in both groups.
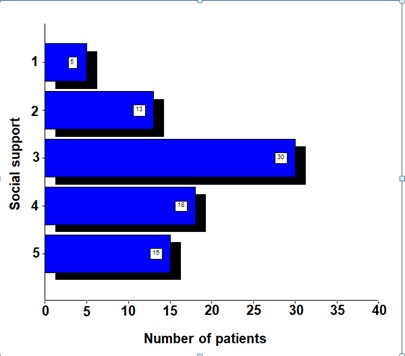 Figure 2: Satisfaction of pregnant women with the social support of the state.
Figure 2: Satisfaction of pregnant women with the social support of the state.
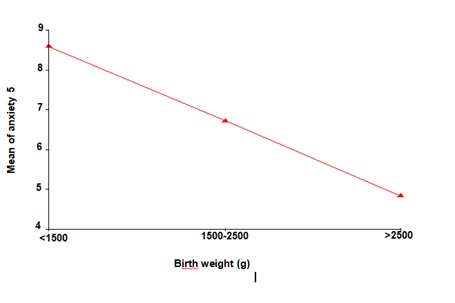 Figure 3: Dependence of neonatal birth weight on anxiety scale score (Day 5) in preterm delivery- the study group.
Figure 3: Dependence of neonatal birth weight on anxiety scale score (Day 5) in preterm delivery- the study group.
|
Scores |
Admission to NICU |
n |
Mean |
SD |
SE |
|
anx1
|
No |
20 |
6.75 |
5.93 |
1.32 |
|
Yes |
21 |
9.23 |
5.03 |
1.09 |
|
|
dep1
|
No |
20 |
4.00 |
3.67 |
0.82 |
|
Yes |
21 |
6.66 |
4.95 |
1.08 |
|
|
str1
|
No |
20 |
10.25 |
6.19 |
1.38 |
|
Yes |
21 |
13.42 |
5.72 |
1.24 |
|
|
epds1
|
No |
20 |
8.10 |
3.44 |
0.77 |
|
Yes |
21 |
9.71 |
3.46 |
0.75 |
|
|
anx5
|
No |
20 |
4.75 |
3.59 |
0.80 |
|
Yes |
21 |
7.42 |
3.51 |
0.76 |
|
|
dep5
|
No |
20 |
3.15 |
2.66 |
0.59 |
|
Yes |
21 |
4.47 |
2.80 |
0.61 |
|
|
str5
|
No |
20 |
7.70 |
4.34 |
0.97 |
|
Yes |
21 |
11.51 |
5.50 |
1.20 |
|
|
epds5
|
No |
20 |
6.85 |
3.60 |
0.80 |
|
Yes |
21 |
7.42 |
3.66 |
0.80 |
Table 2a: DASS and EPDS scores on the first and fifth day of admission and the receiving of neonates to intensive care unit - the study group.
|
|
Statistical parameters |
||
|
Scores |
t |
df |
p |
|
anx1 |
1.449 |
39 |
0.155 |
|
dep1 |
1.951 |
39 |
0.058 |
|
str1 |
1.707 |
39 |
0.096 |
|
epds1 |
1.495 |
39 |
0.143 |
|
anx5 |
2.412 |
39 |
0.021* |
|
dep5 |
1.552 |
39 |
0.129 |
|
str5 |
2.491 |
39 |
0.017* |
|
epds5 |
0.509 |
39 |
0.613 |
Table 2b: Analyses of psychometric scores on the first and fifth day of admission and the receiving of neonates to intensive care unit–the study group.
s*p <0.05
|
Parameters |
anx1 |
dep1 |
str1 |
epds1 |
Weeks of birth |
Birth weight |
Age |
|
|
BMI
|
r |
0.354 |
0.293 |
0.127 |
0.228 |
0.104 |
-0.087 |
0.251 |
|
p |
.001** |
.008** |
0.257 |
.041* |
0.519 |
0.590 |
.024* |
|
|
n |
81 |
81 |
81 |
81 |
41 |
41 |
81 |
|
|
Weeks of admission
|
r |
-.224 |
-.114 |
-.097 |
-.201 |
0.161 |
0.283 |
-0.104 |
|
p |
.045* |
0.311 |
0.389 |
0.072 |
0.316 |
0.073 |
0.356 |
|
|
n |
81 |
81 |
81 |
81 |
41 |
41 |
81 |
|
|
anx1
|
r |
0.664 |
0.743 |
0.638 |
-0.214 |
-0.208 |
0.186 |
|
|
p |
.000** |
.000** |
.000** |
0.179 |
0.192 |
0.097 |
||
|
n |
81 |
81 |
81 |
41 |
41 |
81 |
||
|
dep1
|
r |
0.664 |
0.711 |
0.8 |
-0.297 |
-0.03 |
0.32 |
|
|
p |
.000** |
.000** |
.000** |
0.059 |
0.851 |
.004** |
||
|
n |
81 |
81 |
81 |
41 |
41 |
81 |
||
|
str1
|
r |
0.743 |
0.711 |
0.701 |
-0.27 |
-0.135 |
0.083 |
|
|
p |
.000** |
.000** |
.000** |
0.087 |
0.4 |
0.464 |
||
|
n |
81 |
81 |
81 |
41 |
41 |
81 |
||
|
epds1
|
r |
0.638 |
0.8 |
0.701 |
-0.146 |
-0.036 |
0.286 |
|
|
p |
.000** |
.000** |
.000** |
0.362 |
0.824 |
.010** |
||
|
n |
81 |
81 |
81 |
41 |
41 |
81 |
Table 3: The correlations of DASS and EPDS scores with anthropometric indicators (BMI and age), weeks of admission and weeks of birth.
*p
r=correlation coefficient; p=p value; n=number of subjects
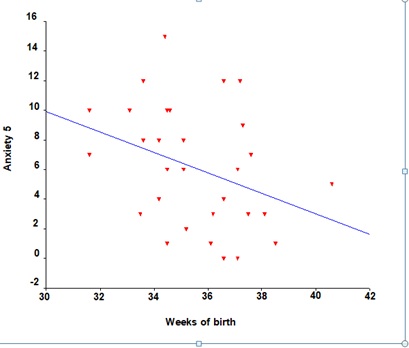 Figure 4: Association of anxiety scores on the 5th day of progesterone therapy and gestational week at the time of delivery.
Figure 4: Association of anxiety scores on the 5th day of progesterone therapy and gestational week at the time of delivery.
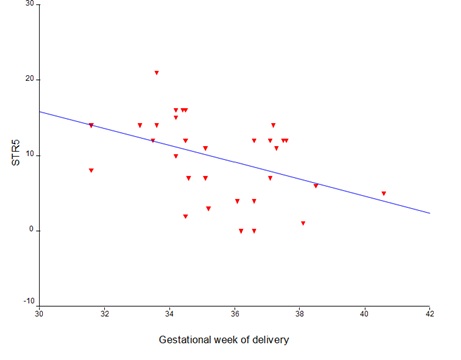 Figure 5: Relationship between stress-test scores on the 5th day of progesterone therapy and gestational week at the time of delivery.
Figure 5: Relationship between stress-test scores on the 5th day of progesterone therapy and gestational week at the time of delivery.
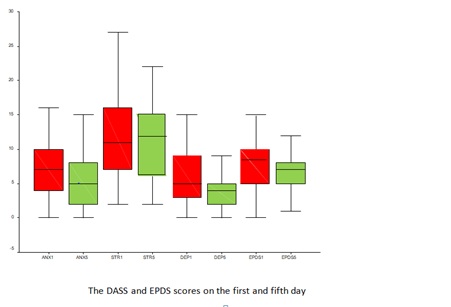 Figure 6: The average DASS and EPDS scores on the first day of addition and after the introduction of progesterone therapy.
Figure 6: The average DASS and EPDS scores on the first day of addition and after the introduction of progesterone therapy.
DISCUSSION
According to the World Health Organization recommendation state politics need to integrate mental health care into primary health care [16]. The main limitation of this study is the use of a small and convenient sample of women from a mostly Caucasian area of Europe, who were hospitalized in a tertiary health center. There is a need for a larger, placebo to progesterone study, placed in a primary care, to exclude possible anxiety and stress caused by the hospitalization itself. Nevertheless, the comeback of therapy with natural progesterone raises the topics of its influence on the psychological status of pregnant women in preterm labor.
The age and BMI of pregnant women, as well as satisfaction with social support, were the main demographic characteristics analyzed in our sample and control. Older age and a higher BMI before pregnancy were associated with higher anxiety, depression, and EPDS scores, while there was no correlation between the age and BMI with the stress scores on admission. Contrary, an African study emphasized younger maternal age as the risk factor for depression [17]. Analyzing the satisfaction with social support, our results show that 70.0% of pregnant women were satisfied (rating of good, very good and excellent). In our study, we emphasized that higher satisfaction with social support in the study group was the result provided by the care and efforts of health professionals during hospitalization. The individual psychological status of a pregnant woman is an important risk factor in imminent preterm delivery. DASS and EPDS represent reliable and cost-effective screening instruments. The DASS questionnaire covered and distinguished symptoms of all three disorders: depression, anxiety and stress [18]. Psychological questionnaire scores at two-time intervals (at the time of admission to the hospital and on the 5th day after progesterone therapy introduction) in our study group showed a highly significant correlation of these psychological risk factors with preterm delivery. Straub et al., in their study showed a significant relationship between antenatal depressive symptoms and preterm birth. It was independent of the maternal age, race/ethnicity, prior preterm delivery and insurance status [19]. There were 31 (73.2%) preterm and 10 (26.8%) term deliveries in our study group. The depression scores on admission and the anxiety and stress scores on the fifth day after progesterone introduction were negatively correlated with the duration of pregnancy. The higher had been the scores of DASS and EPDS, the earlier was the week of delivery. Findings of 39 peer-reviewed studies published in English between 1980 and 2013 indicate that antenatal distress during pregnancy increases the likelihood of preterm birth [20]. Vice versa, increased depression and anxiety scores are significantly more common in threatened preterm birth- for depression the Relative Risk (RR) is 2 and for anxiety 2.7 [21]. Increased depression, anxiety and stress scores during pregnancy were significantly associated with the lower birth weight of premature neonates. The percentage of neonates with lower birth weight was 15% in pregnancies without psychological disorders and even 32% (p <0.05) when DASS scores were elevated [22]. In the study group, only elevated anxiety scores on the fifth day since the progesterone therapy introduction were predictors of delivering neonates with significantly lower birth weight. A prospective study involving 110 pregnant women confirmed a significant association of chronic maternal stress with fetal tachycardia and the intrauterine growth restriction [23]. The observed outcome of our study was also the admission to the neonatal intensive care unit. Newborns of the mothers with higher anxiety and stress scores on the fifth day of progesterone therapy were more often admitted to the neonatal intensive care unit. Kumar and Harkiran in a review article emphasized that children of mothers who were stressed during pregnancy are at increased risk of having impaired emotional and cognitive development later in life [24]. Reviewing 83 reports published between 1977 and 2013, Accortt and colleges found that prenatal depression more consistently influenced low birth weight (50% of the studies) than preterm delivery (25% of the studies) [25]. During the late eighties of the twentieth century, French scientists confirmed steroid genesis in the Central Nervous System (CNS) that was independent of supra-renal and gonadal feedback mechanisms. Pregnenolone, 20 α-OH pregnenolone and progesterone are the main neurosteroids found in humans [26]. Allopregnanolone, a metabolite of natural progesterone (formed in the liver), acts as a neurosteroid. It alters neuronal excitability in the CNS through a membrane-bound - Gamma-Amino-Butter Acid (GABA-A), via a non-genomic mechanism. The influx of chlorine ions into the neuron lowers its excitability, by causing hyperpolarization of the membrane. This event occurs in several milliseconds to seconds [27]. During late pregnancy in rats, allopregnanolone modulates Hypothalamic-Pituitary Axis (HPA) responses to stressful stimuli [28]. In this study, there was a highly significant reduction in the DASS and EPDS scores on the fifth day of progesterone therapy. Progesterone therapy was most effective in reducing the EPDS scores. The latest research was focused on the impact of positive emotions and optimism on the length of pregnancy. Significant fall in optimism and an increase in depressive and anxiety symptoms were observed eight weeks before premature labor (RR-relative risk was 1.5), while in women with term deliveries, no such occurrence was detected. Psychological factors during the first and second trimester affected neither the length of pregnancy nor the birth weight of the neonate [29]. In a study of Serbian authors, self-esteem and optimism were in a highly negative correlation with the postpartum depression [30].
CONCLUSION
According to the results of this study, DASS and EPDS can be the screening instruments for depression, anxiety and stress in preterm labor. Older maternal age and higher BMI before pregnancy predict higher scores on the DASS and EPDS. There is a highly significant association between the elevated DASS and EPDS scores and preterm delivery. The anxiety of a pregnant woman predicts a significantly lower birth weight of the neonate. Anxiety and stress during pregnancy are important predictors of admission to the neonatal intensive care unit. In this study, progesterone therapy was associated with reduced scores on the DASS and EPDS after 5 days for women who experienced preterm labor. Future studies should obtain information from different ethnicity groups, because the expression of emotional problems depends on many aspects: culture, religion, morals, etc., The influence of other tocolytics on psychological status could be an interesting topic for new research. Providing adequate medical and psychological support would contribute to a favorable outcome of the preterm delivery. Positive experience and trust built with the health care system would support couples for having more children.
ACKNOWLEDGEMENT
The authors declare no conflicts of interest.
REFERENCES
- Muglia LJ, Katz M (2010) The enigma of spontaneous preterm birth. N Engl J Med 362: 529-535.
- Guinn DA, Gibbs RS (2003) Preterm labor and delivery. In: Danforth DN, Scott JR (eds.). Scott: Danforth's Obstetrics and Gynecology (9thend). Lippincott Williams & Wilkins, Philadelphi, USA.
- Vismara L (2017) Perspectives on perinatal stressful and traumatic experiences. European Journal of Trauma & Dissociation 1: 111-120.
- Sethna V, Murray L, Netsi E, Psychogiou L, Ramchandani PG (2015) Paternal Depression in the Postnatal Period and Early Father-Infant Interactions. Parent Sci Pract 15: 1-8.
- Dmitrovic BK, Dugali? MG, Balkoski GN, Dmitrovic A, Soldatovic I (2014) Frequency of perinatal depression in Serbia and associated risk factors. Int J Soc Psychiatry 60: 528-532.
- Halbreich U (2005) The association between pregnancy processes, preterm delivery, low birth weight, and postpartum depressions--the need for interdisciplinary integration. Am J Obstet Gynecol 193: 1312-1322.
- Correia LL, Linhares MB (2007) Maternal anxiety in the pre- and postnatal period: A literature review. Rev Lat Am Enfermagem 15: 677-683.
- Gaynes BN, Gavin N, Meltzer-Brody S, Lohr KN, Swinson T, et al. (2005) Perinatal depression: Prevalence, screening accuracy, and screening outcomes. Evid Rep Technol Assess 119: 1-8.
- Kinsella MT, Monk C (2009) Impact of maternal stress, depression and anxiety on fetal neurobehavioral development. Clin Obstet Gynecol 52: 425-440.
- Hilgers TW (2006) Postpartum depression. In: Hilgers TW (ed.). The Medical and Surgical Practice of NaProTECHNOLOGY. Pope Paul VI Institute Press, Omaha, USA.
- Lawrie TA, Hofmeyr GJ, De Jager M, Berk M, Paiker J, et al. (1998) A double-blind randomised placebo controlled trial of postnatal norethisterone enanthate: The effect on postnatal depression and serum hormones. Br J Obstet Gynaecol 105: 1082-1090.
- Rudge CV, Calderon IM, Dias A, Lopes GP, Barbosa AP, et al. (2009) Design and validity of a questionnaire to assess sexuality in pregnant women. Reprod Health 6: 12.
- Crawford JR, Henry JD (2003) The Depression Anxiety Stress Scales (DASS): Normative data and latent structure in a large non-clinical sample. Br J Clin Psychol 42: 111-131.
- Cox JL, Holden JM, Sagovsky R (1987) Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry 150: 782-786.
- Odalovic M, Tadic I, Lakic D, Nordeng H, Lupattelli A, et al. (2015) Translation and factor analysis of structural models of Edinburgh Postnatal Depression Scale in Serbian pregnant and postpartum women - Web-based study. Women Birth 28: 31-35.
- WHO (2010) Mental health and development: Targeting people with mental health conditions as a vulnerable group. WHO Press, Geneva, Switzerland.
- Hartley M, Tomlinson M, Greco E, Comulada WS, Stewart J, et al. (2011) Depressed mood in pregnancy: prevalence and correlates in two Cape Town peri-urban settlements. Reprod Health 8: 9.
- Lovibond PF, Lovibond SH (1995) The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther 33: 335-343.
- Straub H, Adams M, Kim JJ, Silver RK (2012) Antenatal depressive symptoms increase the likelihood of preterm birth. Am J Obstet Gynecol 207: 329.
- Staneva A, Bogossian F, Pritchard M, Wittkowski A (2015) The effects of maternal depression, anxiety, and perceived stress during pregnancy on preterm birth: A systematic review. Women Birth 28: 179-193.
- Bener A (2013) Psychological distress among postpartum mothers of preterm infants and associated factors: A neglected public health problem. Braz J Psychiatry 35: 231-236.
- Din ZU, Ambreen S, Iqbal Z, Iqbal M, Ahmad S (2016) Determinants of Antenatal Psychological Distress in Pakistani Women. Noro Psikiyatr Ars 52: 152-157.
- Shafizadeh M, Mehdizadeh M (2009) Relationship Between Maternal Distress with Fetus Growth Rate: Mediator Role of Heart Rate. J Applied Sci 9: 193-196.
- Kumar N, Harkiran PK (2017) Effect of Prenatal Maternal Stress on Foetal Outcome and its Long Term Consequences: A Review of Literature. EC Gynaecology 3.6: 432-438.
- Accortt EE, Cheadle AC, Dunkel Schetter C (2015) Prenatal depression and adverse birth outcomes: An updated systematic review. Matern Child Health J 19: 1306-1337.
- Schumacher M, Robert F, Baulieu EE (1999) [Neurosteroids: Trophic effects in the nervous system]. J Soc Biol 193: 285-292.
- Wang M (2011) Neurosteroids and GABA-A Receptor Function. Front Endocrinol (Lausanne) 2: 44.
- Brunton PJ, Russell JA (2011) Allopregnanolone and suppressed hypothalamo-pituitary-adrenal axis stress responses in late pregnancy in the rat. Stress 14: 6-12.
- Pesonen AK, Lahti M, Kuusinen T, Tuovinen S, Villa P, et al. (2016) Maternal Prenatal Positive Affect, Depressive and Anxiety Symptoms and Birth Outcomes: The PREDO Study. PLoS One 11: 0150058.
- Fazlagi? A, Soleša-Grijak ? (2011) Optimizam i emocionalna inteligencija kod postpartalne depresije. Sažetak radova. VII dani primenjene psihologije.a
Citation: Dakovic E, Jurišic A, Rudic Biljic Erski I, Mihajlovic S, Džatic Smiljkovic O, et al. (2020) Psychological State and Threatened Preterm Delivery- The Impact of Progesterone Therapy. J Reprod Med Gynecol Obstet 5: 047.
Copyright: © 2020 Elena Dakovic, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

