
Quality of Telehealth Services in Delivery of Paediatric Surgical Care in Australia: A Systematic Literature Review
*Corresponding Author(s):
Josephine De CostaRoyal Darwin Hospital, Northern Territory, Australia
Email:josephinedecosta@gmail.com
Abstract
Introduction: Telehealth services are commonly used in many aspects of medicine to improve access to medical care for populations in rural and remote regions, and can and do play an important role in ensuring equitable access to paediatric surgery in Australia’s more rural and remote areas. The aim of this paper was to provide an overview of current literature on the use of telehealth services within paediatric surgery, with a secondary objective being to demonstrate the accuracy of initial diagnoses made via telehealth as compared to FTF (pre-operative) diagnoses.
Methodology: A systematic review of the literature regarding use of telehealth in paediatric surgery from 2008-2018.
Results: Six articles were included in the final review. Orthopaedic issues and cases of possible undescended testes were some of the most common diagnoses referred by telehealth. Referrals for cases of possible undescended testes were both the most common cause of referral but also the most common misdiagnosis. One study of orthopaedic referrals found that 86% of all closed fractures were transferred to a tertiary centre despite 45% of these not requiring manipulation under anaesthesia or surgical fixation.
Conclusion: Telemedicine can and does play an important role in providing paediatric surgical services, particularly in areas that are as geographically vast as Queensland and Western Australia. Where local staff are adequately trained and experienced, diagnoses made via telehealth have a high level of concordance with those made FTF and pre-operatively.
Introduction
Australia has a surface area of 7.6 million squared kilometres and a population of 24.6 million people [1-3]. However, as of 2011, only 18% of children under the age of 14 lived in major cities, with 40% living in inner and outer regional areas and the remaining 45% living in remote and very remote areas [4]. Despite this, the vast majority of paediatric surgical services are concentrated in the major capital cities. This means that a large proportion of children seen within these centres must travel from their homes, often for significant distances, for surgical services. This can cause significant disturbance to them and to their family’s lives, in the form of time taken for travel, as well as through indirect costs such as for travel, food, and lodgings [5].
The Royal Australasian College of Surgeons’ 2017 position paper on Surgery in Children notes that the workforce of specialised paediatric surgeons has not grown in proportion to the increasing demand for services in specialised paediatric hospitals. Within the paper, they recommend in particular that, where appropriate, low-complexity patients be seen and managed by non-specialists (such as general surgeons) in local facilities [6].
Telehealth services are commonly used in many aspects of medicine to improve access to medical care for populations in rural and remote regions, and can and do play an important role in ensuring equitable access to paediatric surgery in Australia’s more rural and remote areas. Surgical services provided via telehealth may incorporate a pre-surgical consult (to assess and book new patients), as well as post-operative follow-up. Currently, telehealth paediatric surgical services are relatively common in Australia and play a particularly important role in physically larger states with large rural and remote populations such as Queensland, Western Australia, and the Northern Territory. One example of this is the Queensland Telepediatric Service (QTS), which connects clinicians based at Brisbane’s Royal Children’s Hospital with over 100 regional and remote Queensland hospitals, and carried out 20,000 remote consultations from 2000-2014, including numerous paediatric surgery consults [7]. Telemedical services also have important ramifications for the possible teaching of rural and remote surgeons, non-specialist doctors, and trainees [8-10]. However, these services should only be introduced if they provide a level of quality equivalent to that provided by tertiary centres in Face-To-Face (FTF) consultations. The aim of this paper was therefore to provide an overview of current literature on the use of telehealth services within paediatric surgery, with a secondary objective being to demonstrate the accuracy of initial diagnoses made via telehealth as compared to FTF (pre-operative) diagnoses.
Methodology
This study consists of a systematic review of the literature regarding use of telehealth in paediatric surgery. Literature searches were performed on 28 October 2018 using Medline (via OvidSP), with MESH search terms (“paediatric surgery” OR “pediatric surgery” OR (surgery or “general surgery” AND paediatric* OR pediatric*) AND (telehealth OR telemedicine)). Results were restricted to English-language, peer-reviewed journal articles published after 1 January 2008 (giving a total of ten years prior to the search for publication; this was felt to be an acceptable period given the likely changes in technology and developments within telehealth technology within the last decade). No other inclusion or exclusion criteria were used. A total of 14 articles were found in the initial search, with four excluded on the basis of the abstract for irrelevance to the topic (Figure 1). Four articles were excluded for irrelevance after full-text perusal.
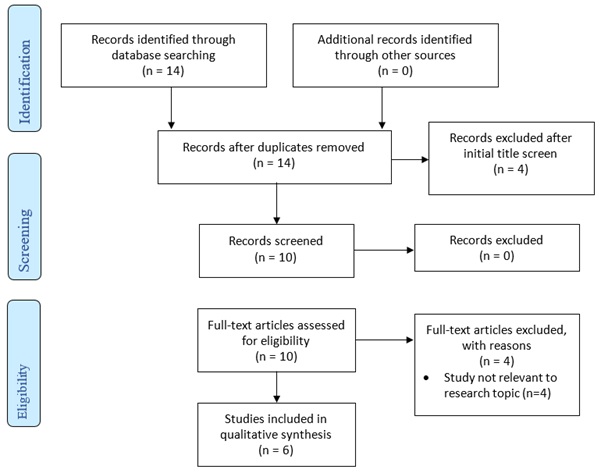
Figure 1: Search Strategy.
The final six articles underwent assessment for risk of bias using an appropriately modified version of the National Heart, Lung and Blood Institute’s Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies (Table 1). This checklist was used as each of the studies included in this analysis comprised a retrospective review and/or audit of prior use of telemedicine for provision of paediatric surgical services. Each of the six articles had a high score using this tool, indicating an overall low risk of bias and high-quality for each of the papers.
|
|
[1] |
[13] |
[2] |
[12] |
[3] |
[11] |
|
1. Was the research question or objective in this paper clearly stated? |
√ |
√ |
√ |
√ |
√ |
√ |
|
2. Was the study population clearly specified and defined? |
√ |
√ |
√ |
√ |
√ |
√ |
|
3. Was the participation rate of eligible persons at least 50%? |
√ |
√ |
√ |
√ |
√ |
√ |
|
4. Were all the subjects selected or recruited from the same or similar populations (including the same time period)? Were inclusion and exclusion criteria for being in the study prespecified and applied uniformly to all participants? |
√ |
√ |
√ |
√ |
√ |
√ |
|
5. Was a sample size justification, power description, or variance and effect estimates provided? |
Χ |
Χ |
Χ |
Χ |
Χ |
Χ |
|
6. Was the timeframe sufficient so that one could reasonably expect to see an association between use of telehealth and outcome if it existed? |
√ |
√ |
√ |
√ |
√ |
√ |
|
7. Where exposure and use of telehealth varied, did the study examine different levels of the exposure as related to the outcome (e.g., categories of exposure, or exposure measured as continuous variable)? |
Χ |
√ |
√ |
Χ |
√ |
Χ |
|
8. Were the exposure measures (independent variables) clearly defined, valid, reliable, and implemented consistently across all study participants? |
√ |
√ |
√ |
√ |
√ |
√ |
|
9. Was the exposure(s) assessed more than once over time? |
Χ |
√ |
√ |
Χ |
√ |
Χ |
|
10. Were the outcome measures (dependent variables) clearly defined, valid, reliable, and implemented consistently across all study participants? |
√ |
√ |
√ |
√ |
√ |
√ |
|
11. Were the outcome assessors blinded to the exposure status of participants? |
Χ |
Χ |
Χ |
Χ |
Χ |
Χ |
|
12. Was loss to follow-up after baseline 20% or less? |
√ |
√ |
√ |
√ |
√ |
√ |
|
13. Were key potential confounding variables measured and adjusted statistically for their impact on the relationship between exposure(s) and outcome(s)? |
Χ |
Χ |
Χ |
Χ |
Χ |
Χ |
Table 1: Assessment of risk of bias using the quality assessment tool for observational cohort and cross-sectional studies.
Results
A total of six articles were included in the final review. Two directly compared initial diagnosis made at telehealth appointments with final pre-operative assessments and diagnoses, and four reviewed the overall service provision and use of telehealth versus Face-To-Face (FTF) assessments, as well as follow-up reviews within the relevant paediatric surgical service.
The two studies which analysed concordance between initial diagnoses via telehealth and pre-operative FTF diagnoses showed very high agreement between the two, from 94% for general surgical cases to 99% of paediatric otolaryngology cases [1,11]. 93% of cases included in Smith et al., paper had definitive surgical management which correlated to the initial videoconference plan, with four of the five cases that had change in management having only minor changes to their treatment plan [11].
Although search criteria did not limit findings to Australian research, four of the studies included look exclusively at services provided through the QTS [1-3,11], which conducted almost 4,000 tele-consultations in a thirteen-year period from 2001-2014 [2]. In looking at the provision of paediatric surgery sub-specialties [2], Smith et al., review of the telehealth consults of the QTS found that 50% of consults were in relation to paediatric burns, general surgical problems comprised 21%, ear, nose and throat 19%, orthopaedics 9% and vascular anomalies 2% over a thirteen-year period [2].
Of all the general paediatric cases studied by Brownlee et al. [1], referrals for cases of possible undescended testes were both the most common cause of referral (accounting for 17% of all general paediatric surgery referrals through the QTS in their 11-month study period as well as in Smith’s 12-month study period in 2011-2012 [2]) but also the most common misdiagnosis, with only 7 of 15 orchidopexies booked via telediagnosis being completed [1]. Of the eight procedures which did not go ahead, three were cancelled following normal testicular examination pre-operatively, one was converted from laparoscopic to inguinal orchidopexy as the testis was palpable inguinally, and four were converted from inguinal orchidopexy to laparoscopy plus first-stage Fowler-Stephens procedure as testes were impalpable pre-operatively [1]. By contrast, Canon, who studied the use of telemedical follow-up of paediatric urological surgery - including hypospadias review - found that video telemedical follow-up was not associated with poorer outcomes, including for hypospadias which requires a relatively high level of visualisation of the surgical field [12].
Rowell, studying use of telehealth for paediatric orthopaedic surgery in Western Australia, found that 86% of all closed fractures were transferred to a tertiary centre despite 45% of these not requiring manipulation under anaesthesia or surgical fixation, meaning that they could easily have been managed by local staff with adequate radiological imaging supported via telehealth services with orthopaedic specialists at tertiary centres [3]. They also noted that 26 out of 27 K-wire removals were performed after transfer to a tertiary centre, though this is a procedure that could be easily performed by local staff with adequate experience in conducting clinical physical assessments [3]. Interestingly, 58% of the cases whose initial presentation to an orthopaedic specialist was via telehealth had the remainder of their care conducted via telemedicine, with no need for FTF consultation [3].
In considering the logistical advantages of telehealth, Canon in Arkansas found that for every 37km further from a tertiary health centre, a patient’s family was 111% more likely to use telehealth services [12]; Rowell found that 40% of patients using telehealth services had diagnosed cerebral palsy, intellectual disability, or congenital syndromes, demonstrating that telehealth may provide key advantages for this group of patients and their families in accessing paediatric surgical healthcare [13].
Discussion
The above results show that telemedicine can and does play an important role in providing paediatric surgical services, particularly in areas that are as geographically vast as Queensland and Western Australia.
However, the safety and efficacy of telehealth services can be dependent upon the clinical acumen and procedural skills of the local staff at the remote health centre where the patient is being seen. Certainly, complex patients requiring multidisciplinary team input will not be appropriate for telemedical services. However, even simpler procedures may not always be appropriate or adequately performed to be done exclusively reliant on telehealth, if the diagnosis rests in large part on subtle clinical signs that can only be picked up physically by either the local clinician in the remote setting, or a paediatric surgeon in a FTF consult. This is evident in Brownlee et al., experience with UDT and the change in management plans for multiple orchidopexies. Examination of testes requires a relatively significant level of experience with both normal and abnormal anatomy and as a result remote local staff may not have a high enough caseload to ensure clinical accuracy. This could be managed either through increased training of local staff, or a lower threshold for organising FTF consults for possible UDT patients. However, as Brownlee et al note, this is a particular problem when considering the rates of false negatives (ie patients who are recorded as having normal testes when in fact they have UDT), as referring all remote patients for FTF is not logistically or financially feasible [1].
Management of non-complex, closed fractures may also represent an area where increased training of local staff in orthopaedic management, coupled with increasing access to local radiological services, could result in significant cost savings. This could be achieved by minimising the number of transfers to tertiary centres for non-operative non-manipulative orthopaedic management.
As this review selected for English-language articles published after 2008, selection bias may be present. It is important to acknowledge that five of the studies included relate to Australian services, with four of them relating to a single service (the QTS), meaning that these results may not in fact be generalisable to other services. Finally, all included studies were retrospective, resulting in possible selection and recall bias.
Conclusion
Telemedicine can and does play an important role in providing paediatric surgical services, particularly in areas that are as geographically vast as Queensland and Western Australia. Where local staff are adequately trained and experienced, diagnoses made via telehealth have a high level of concordance with those made FTF and pre-operatively. Telehealth services can also cover a wide range of paediatric surgery subspecialties. This has important ramifications for paediatric surgical services worldwide, with the potential for evidence-based efficient systems to be implemented within and between countries, facilitating delivery of services in low-resource settings where paediatric surgical services may not be otherwise available.
References
- Brownlee GL, Caffery LJ, McBride CA, Patel B, Smith AC (2017) Telehealth in paediatric surgery: Accuracy of clinical decisions made by videoconference. J Paediatr Child Health 53: 1220-1225.
- Smith AC, Garner L, Caffery LJ, McBride CA (2014) A review of paediatric telehealth for pre- and post-operative surgical patients. J Telemed Telecare 20: 400-404.
- Rowell PD, Pincus P, White M, Smith AC (2014) Telehealth in paediatric orthopaedic surgery in Queensland: A 10-year review. ANZ J Surg 84: 955-959.
- NHRC (2018) Demography. The Little Book of Rural Health Numbers.
- Bator EX, Gleason JM, Lorenzo AJ, Kanaroglou N, Farhat WA (2015) The burden of attending a pediatric surgical clinic and family preferences toward telemedicine. J Pediatr Surg 50: 1776-1782.
- Royal Australasian College of Surgeons (2017) Position Paper: Children in Surgery. Royal Australasian College of Surgeons, Melbourne, Australia.
- McDonald K (2014) Telehealth for kids racks up major milestone. Pulse+IT.
- Numanoglu A (2017) Using telemedicine to teach paediatric surgery in resource-limited countries. Pediatr Surg Int 33: 471-474.
- Holland AJ, Soundappan SVS, Oldmeadow W (2008) Videoconferencing surgical tutorials: Bridging the gap. ANZ J Surg 78: 297-301.
- Bruns NE, Irtan S, Rothenberg SS, Bogen EM, Kotobi H (2016) Trans-Atlantic telementoring with pediatric surgeons: Technical considerations and lessons learned. J Laparoendosc Adv Surg Tech A 26: 75-78.
- Smith AC, Dowthwaite S, Agnew J, Wootton R (2008) Concordance between real-time telemedicine assessments and face-to-face consultations in paediatric otolaryngology. Med J Aust 188: 457-460.
- Canon S, Shera A, Patel A, Zamilpa I, Paddack J, et al. (2014) A pilot study of telemedicine for post-operative urological care in children. J Telemed Telecare 20: 427-430.
- Rimal D, Fu JHH, Gillett D (2017) Our experience in using telehealth for paediatric plastic surgery in Western Australia. ANZ J Surg 87: 277-281.
Citation: de Costa J (2021) Quality of Telehealth Services in Delivery of Paediatric Surgical Care in Australia: A Systematic Literature Review. Archiv Surg S Educ 3: 032.
Copyright: © 2021 Josephine de Costa, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

