
Quaternary Prevention and / or Hypermedicalization. Fragility (Disease) and / or Lobbying
*Corresponding Author(s):
Colucci GMedOnLine-Statte, Statte (TA), Italy
Email:drgcolucci@libero.it
Abstract
Approximately 15-20% of patient-doctor meetings are defined by the latter as difficult. Difficult patients are defined as those who elicit strong negative emotions from their physicians. If not acknowledged and managed correctly, these feelings can lead to diagnostic errors, unpleasant confrontations, and troublesome complaints or legal claims. There are no difficult patients but difficult relationships due to characteristics of the patient, the doctor and / or influences of the society.
Aim of the study: Evaluate the relationship of the Difficult Patient (DP) with the Over Medicalization (OM) and how much it can affect the Clinical Practice (CP) and Public Spending (PS).
Materials and methods: Workgroup of the vocational training of general practice of Apulia Region has developed an evaluation form on DP and OM, which was administered to Doctors, who attended the General Practice’s (GP) office.
Results: 121 participating doctors. In the abscissae we have formulated three Items (excessive use and little use of health services, excess of medicines causes damage to health, use of validated medical practices can potentially be harmful and cause waste) in ordinate 9 items with various personalities of patients: 47.1% the patient was hypochondriac; 36.4% psychological; 27.3% were demanding. 35.5% believe that over-medicalization is observed in chronic degenerative diseases. The evidence of overdiagnosis: 42.2% dementia; 33.9% hypertensive heart disease; 32.2% greater depression. The causes of over-medicalization: 60.3% lack of GP integration and specialist; 58.7% defensive medicine; 55.4% request for pcs.
Conclusion: From the observations of the colleagues it emerged that collaboration between the various health figures (GP and specialists) is opportune to better identify the DP.
Introduction
The scientific community has defined in the last fifty years the definition of prevention by differentiating it into three main categories in relation to the clinical status of the subjects on which to implement it as well as the objectives to be pursued, thus defining primary, secondary and tertiary prevention [1,2]. The WONCA (World Organization of Family Doctors) defined these 3 categories of prevention in the International Dictionary of General/Family Practice (2003) as: 1) Primary Prevention: correcting lifestyles and performing an early diagnosis; 2) Secondary Prevention: treating diseases and/or comorbidities; 3) Tertiary Prevention: rehabilitation and management of multimorbidities and polytherapy. Recently, however, we have witnessed an increasing interference of society and the media on health management and health promotion, encouraging periodic screening and follow-up campaigns.
This drive sometimes too vehemently, added to a defensive medicine that often leads to a hypermedicalization of health conditions not yet pathological, has brought out the concept of Quaternary prevention, initially proposed by Marc Jamoulle, defined as a condition of malaise of the patient in the absence of a full-blown picture of actually defined disease (Figure 1). In fact, many patients may feel ill without having a well-defined disease and may be subject to an increased risk of being harmed by overtesting and hypermedicalization. In fact, patients and physicians tend to overestimate the benefits and underestimate the harms of preventive and curative interventions [3,4]. The concept of quaternary prevention should therefore always be present in the mind of the Doctor whenever he intervenes on the patient with / without disease in causing damage.
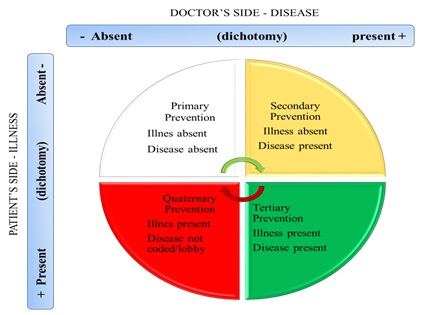 Figure 1: Model of different categories of prevention in the relational model proposed by Marc Jamoulle. Modified through the study performed [5].
Figure 1: Model of different categories of prevention in the relational model proposed by Marc Jamoulle. Modified through the study performed [5].
The Wonca defines quaternary prevention as the set of actions taken to identify the patient at risk of hypermedicalization, to protect him from new medical invasions and to suggest interventions, which are ethically acceptable. The questions that must therefore be asked concern the topicality of the definition of quaternary prevention and the dimensions of the phenomenon; the usefulness of its definition in protecting patients from medical harm; the inevitability of such a concept in good clinical practice. In this sense, in fact, the outpatient visits performed daily in the general medicine clinic are defined as difficult in 15-20% of cases. In most cases these difficulties arise from a bad doctor-patient relationship and these relationships can result, if not recognized and managed correctly, in diagnostic errors, unpleasant comparisons and annoying complaints or legal claims. There are no difficult patients but difficult relationships due to clinical characteristics of the patient, the doctor and/or societal influences. Objectives of the study: to evaluate the relationship of the Difficult Patient with Over Medicalization and how much it can influence clinical practice and Public Spending.
Materials And Methods
The working group of the Professional Training of General Medicine of the Puglia Region has developed an evaluation sheet (Figures 2 and 3) to define the difficult patient and the over medicalization. The card was administered to doctors in training during the three-year course for General Medicine, after they had attended the General Medicine (MG) clinic for 12 months. In the card it was asked to express a judgment about the possible overuse of health services, excessive medication causing damage to health, and the use of medical practices suited to the guidelines. This judgment was related to the different personalities of the patients, stratified in 9 different types: hypochondriac, non-cooperating, suffering from psychological disorders, resorting to non-medical channels of information, excessive recourse to the doctor, demanding, suspicious, cunning, and other. We also asked which were the diseases with the greatest impact on public spending, which diseases with over-diagnosis and what were the causes of over-medicalization.
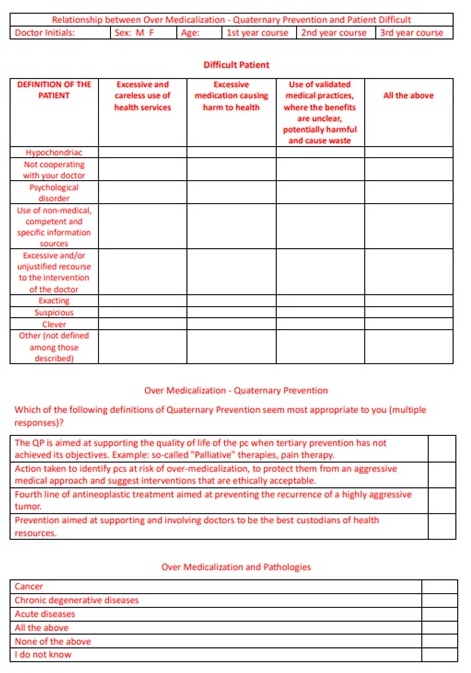
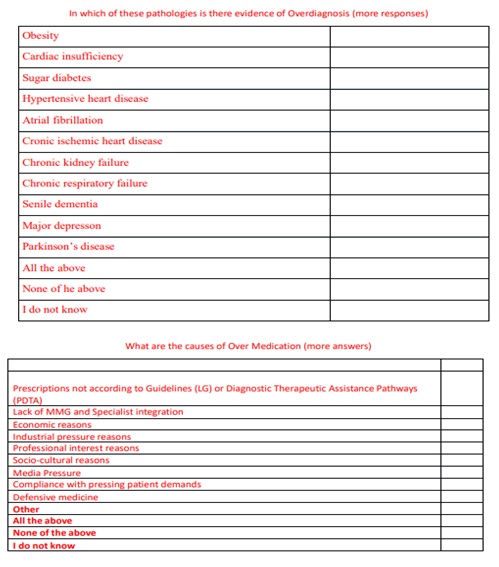 Figures 2 and 3: Questionnaire administered to doctors in the general medicine training course.
Figures 2 and 3: Questionnaire administered to doctors in the general medicine training course.
Results
The questionnaire was submitted to 121 doctors (M 38 31.4%) attending the specific training course in general medicine during the three-year period (assisted population 180,000 total); 42 attended the first year of the course, 43 the second and 36 the third table 1. First, the difficult patient was characterized in relation to behavioral characteristics. Subsequently, we evaluated the methods of access and use of the drugs of the patients who attended our clinic, evaluating specifically: 1) an excessive and unwise use of health services; 2) excess of medicines causing harm to health; 3) use of validated medical practices, where the benefits are unclear, potentially harmful and cause waste. The results showed that the patients who use health services excessively were those who already went to the MMG with excessive frequency (51.2% of cases), followed by the hypochondriac with 38.8%. 2) non-cooperators in 28.9% of cases, those who had psychological disorders in 24.8% (Table 2).
|
Course year |
N°Number (percent) |
|
First year |
42 (34.7) |
|
Second year |
43 (35.5) |
|
Third year |
36 (29.7) |
Table 1: Study participants per year of training.
|
Patient Definition |
N° |
Excessive and careless use of health services |
Excess of medicines causes harm to health |
Use of validated medical practices, where the benefits are unclear, potentially harmful and cause waste |
All |
|
Hypochondriac |
118 (97.5) |
47 (38.8) |
16 (13.2) |
7 (5.8) |
57 (47.1) |
|
Non-collaborative |
116 (95.9) |
27 (22.3) |
35 (28.9) |
39 (32.2) |
25 (20.7) |
|
Suffering from psychological disorders |
109 (90.1) |
23 (19.0) |
30 (24.8) |
18 (14.9) |
44 (36.4) |
|
Using non-medical information channels |
116 (95.9) |
15 (12.4) |
19 (15.7) |
62 (51.2) |
29 (24.0) |
|
Excessive appeal to medical services |
116 (95.9) |
62 (51.2) |
26 (21.5) |
10 (8.3) |
30 (24.8) |
|
Exacting |
110 (90.9) |
45 (37.2) |
15 (12.4) |
23 (19.0) |
33 (27.3) |
|
Suspicious |
110 (90.9) |
25 (20.7) |
29 (24.0) |
33 (27.3) |
26 (21.5) |
|
Clever |
102 (84.3) |
45 (37.2) |
10 (8.3) |
29 (24.0) |
25 (20.7) |
|
Other |
23 (19.0) |
0 |
2 (1.7) |
2 (1.7) |
21 (17.4) |
Table 2: Difficult patient definition and clinical approach.
We asked if the over-medicalization was mainly due to acute, chronic degenerative and / or tumor pathologies with the following results: acute pathologies 17.4%; chronic/degenerative 35.5%; tumor 11.6%; all the previous 46.3%. Among the chronic pathologies those that were the cause of over-medicalization were in descending order of frequency: Senile dementia 42.2%; Hypertensive heart disease: 33.9%; Major depression 32.2% as can be seen from table 3 which lists the pathologies of those at greatest risk of frailty according to the “Charlson Comorbidity Index” [6,7].
|
Chronic diseases |
N°Number (percent) |
|
Obesity |
12 (9.9) |
|
Cardiac insufficiency |
17 (14.1) |
|
Sugar diabetes |
20 (16.5) |
|
Hypertensive heart disease |
41 (33.9) |
|
Atrial fibrillation |
7 (5.8) |
|
Cronic ischemic heart disease |
10 (8.3) |
|
Chronic kidney failure |
21 (17.4) |
|
Chronic respiratory failure |
22 (18.2) |
|
Senile dementia |
51 (42.2) |
|
Major depresson |
39 (32.2) |
|
Parkinson’s disease |
1 (0.8) |
|
All the above |
11 (9.1) |
|
None of the above |
19 (15.7) |
|
I do not know |
8 (6.6) |
Table 3: Over medicalization and pathologies.
To the question of what are the causes of over-medicalization of uncodified quaternary prevention / strong powers, they answered as follows: non-integration between health figures 60.3%; defensive medicine 58.7%; request for patients 55.4%; no LG or PDTA: 38.0%; mass average 36.4% (Table 4).
|
Diseases |
N°Number (percent) |
|
No Guidelines (GL) or Diagnostic Therapeutic Assistance Pathways (DTAP) |
46 (38.0) |
|
No integration |
73 (60.3) |
|
Economic reasons |
40 (33.1) |
|
Industrial pressure reasons |
15 (12.4) |
|
Professional interest reasons |
15 (12.4) |
|
Socio-cultural reasons |
27 (22.3) |
|
Media |
44 (36.4) |
|
Patient requests |
67 (55.4) |
|
Defensive medicine |
71 (58.7) |
|
Other |
2 (1.7) |
|
All the above |
33 (37.3) |
|
None of the above |
0 |
|
I do not know |
0 |
Table 4: Causes of over medication.
Discussion
In primary prevention it is mandatory to perform preventive interventions to have important benefits on mass health. But there are interventions that involve significant damage. For example, in the latest mass anti-COVID vaccination of particular interest are the events of myocarditis and pericarditis, particularly within 7 days of the second dose of the primary series, with a higher risk in adolescents and young adult males. Data available from short-term follow-up suggest that most individuals have had resolution of symptoms, although no information is yet available on potential sequelae in the long run [8]. In addition, very often hematochemical tests (such as tumor biomarkers) are performed in primary prevention, an error also from a clinical point of view. Of course, in undergoing such tests there are certainly false positives and this leads to an increase in unjustified expenditure for unnecessary investigations. Even in cardiovascular diseases (Obesity, Arterial Hypertension, Diabetes Mellitus) reducing the cut off index transforms a cohort of people at risk into patients with full-blown pathology. This involves growth of comorbidities, polypharma therapy, exposure to adverse effects, interaction with other drugs, liver and kidney damage [9].
The consequence of such attitudes leads to medical care which is too interventional and to a greater risk of adverse events, this is quaternary prevention. Often the guidelines, especially in General Medicine, are based on trials with a small number of enrolled subjects, or in different contexts for geolocation, social and anthropological culture. Medical science of the territory we has the greatest potential database that provides real life data, therefore able to formulate guidelines and Diagnostic Therapeutic Assistance Pathways (PDTA) in collaboration with Hospitalists and Universities.
The mass media have a considerable influence on our profession, starting with the economy, on the one hand the industries that incentivize the prescription of expensive drugs, on the other the administration that pushes for non-prescription, both for the resistance of antibiotic therapy and for the prescription of off-label drugs. Finally, defensive medicine - all those actions that a doctor decides to implement with the aim of defending and protecting himself from any harmful damage to the patient that could result from medical negligence. Defensive medicine can be positive (commissive) or negative, also called omissive. All this is quaternary prevention. In today's society, gender identity undergoes throughout its life, divided into decades, pathologies that are first of an acute nature (in childhood) and then turn into chronic (cardiovascular risk) and neoplasms, genomic diseases that over time become self-limiting, finally terminal.
As we have shown, the prevention of overdiagnosis or the prevention of excessive treatment is amenace of our society. Therefore, every patient can be in each of these quadrants [10-12]. The new WONCA review on Quaternary Prevention is: “Action taken to protect people (people/people/patients) from interventions that could cause more than benefit.” Wagner H states “The concept of quaternary prevention is nothing more than the systematization of the concept of “first do no harm” in our clinical practice; clinical care must be ensured and those who practice excessive medicine must be protected” [13]. The last point to be addressed is digitalization. It is the conversion process that, applied to the measurement of a physical phenomenon, determines its transition from the field of continuous values to that of discrete values. This process is now commonly synthesized in terms of the transition from analog to digital in audio, video, images and text. This means the end of the doctor-patient relationship and the practical clinic. Society is not ready for the abrupt transition, but the process must be slow and over time.
Conclusion
Quaternary prevention has many limitations. It takes a lot of studies to improve our ordinary work. We present (Table 5) a decalogue to improve the Health System.
|
Pro |
Contro |
|
Implement in the last years of University the practical internship at the MdF |
Low participation and interest in General Medicine |
|
The Order of Doctors supreme body to re-establish the Deontological Code |
Conflict between Specialists |
|
In the communication > Enoxpatia |
Empathy only |
|
Excellent practical clinic for diagnosis and therapy |
Reduce Health Spending |
|
Clinic dedicated to chronic diseases (with the different health figures) |
Reduce health spending |
|
Do not perform high-cost instrumental investigations |
Defensive medicine |
|
A new and different culture of difficult patient management |
Examine with other colleagues the various types of difficult patients and possible therapy |
|
Coordinate the execution of examinations and therapies in comorbidities |
Lack of integration between specialist figures |
|
Adoption of standardized protocols |
Compliance with pressing patient demands |
|
Telemedicine Yes |
Telemedicine No |
Table 5: How to improve General Medicine?
References
- World Health Organization (WHO) WHO traditional medicine. In: Chinitz DP, Rodwin VG (eds.). On Health Policy and Management (HPAM): Mind the theory-policy-practice gap. Int J Health Policy Manag 3: 3613.
- Harrison C, Britt H, Miller G, Henderson J (2013) Prevalence of chronic conditions in Australia. PLoS One 8: 67494.
- Lykkegaard J, Larsen PV, Paulsen MS, Søndergaard J (2014) General practitioners’ home visit tendency and readmission-free survival after COPD hospitalisation: A Danish nationwide cohort study. NPJ Prim Care Respir Med 24: 14100.
- Laux G, Kuehlein T, Rosemann T, Szecsenyi J (2008) Co- and multimorbidity patterns in primary care based on episodes of care: Results from the German CONTENT project. BMC Health Serv Res 8: 14.
- Soler JK, Okkes I, Wood M, Lamberts H (2008) The coming of age of ICPC: celebrating the 21st birthday of the International Classification of Primary Care. Fam Pract 25: 312-317.
- Robusto F, Colucci E, Dell’Aquila L, Colucci V, D’Ettore A, et al. (2015) Il ruolo della Medicina Generale nel management della depressione minore e delle comorbilità negli anziani: Sviluppo di una checklist di sintomi per la diagnosi differenziale. Minerva Psichiatrica 56: 61-69.
- Robusto F, Lepore V, D'Ettorre A, Lucisano G, De Berardis G, et al. (2016) The drug derived complexity index (DDCI) predicts mortality, unplanned hospitalization and hospital readmissions at the population level. PloS One 11: 0149203.
- FDA (2022) Cardio2022 Vac2022 Med2022 Farma2022. FDA, Maryland, USA.
- Bentzen N (2003) Wonca Dictionary of General/Family Practice. PH3C, Copenhagen, Denmark.
- Tomljenovic L, Shaw CA (2013) Human papillomavirus (HPV) vaccine policy and evidence-based medicine: are they at odds? Ann Med 45: 182-193.
- Wolinsky H (2005) Disease mongering and drug marketing. Does the pharmaceutical industry manufacture diseases as well as drugs? EMBO Rep 6: 612-614.
- Mariño MA (2015) Incidentalomas: Conceito, relevância e desafios para a prática médica. Revista brasileira de medicina de família e comunidade 35.
- Kuehlein T, Sghedoni D, Visentin G, Gérvas J, Jamoulle M (2010) Quaternary prevention: A task of the general practitioner. Prim Care.
Citation: Colucci G, Robusto F, Colucci E, Zamparella M, Montorsi S, et al. (2022) Quaternary Prevention and / or Hypermedicalization. Fragility (Disease) and / or Lobbying. J Gerontol Geriatr Med 8: 144.
Copyright: © 2022 Colucci G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

