
Racial Differences in the Emotional Impact and Coping Strategies Employed by Older Adults during the COVID-19 Pandemic in Arkansas
*Corresponding Author(s):
Gohar AzharDepartment Of Geriatrics, Donald W. Reynolds Institute On Aging, University Of Arkansas For Medical Sciences, 4301 W. Markham Street, #798, Little Rock, AR 72205, United States
Tel:+1 5016865821,
Email:azhargohar@uams.edu
Abstract
We examined different stressors reported by older adults residing in Central Arkansas. During the COVID-19 pandemic. An anonymous survey was administered to 118 older adults (55+). Decreased social activities outside the home was the most common stressor reported (77%), followed by shortage of items at the grocery store and inability to shop (57%), inability to visit places of worship (51%), attend recreational activities (50%), or travel out of state (45%). Caucasian-American/White (CA) appeared more stressed by their inability to go to the gym compared to AA respondents (30% vs 4% p < 0.01). Talking with friends was favored more by CA compared with AA respondents (69% vs 40% p < 0.01). AAs found COVID-19 media reports more useful compared with CAs (76% vs 42% p < 0.01). A higher percentage of AAs regarded telehealth visits with favorably compared with CA (55% vs 39% p < 0.01). Overall, older adult AAs appeared to be more resilient and adaptable during the COVID-19 pandemic. Racial differences in perspectives and coping strategies will need further study to develop programs supporting diverse groups of individuals during a pandemic or other stressful conditions or events.
Keywords
Aged; COVID-19; Race; Resilience; Social isolation; Stress
Introduction
The imminent fear of contracting COVID-19, along with widespread social disruption created by efforts to limit its spread, such as lockdowns and social distancing, has significantly increased the prevalence of stress, anxiety and depression worldwide [1-5]. People’s perception and experience of social isolation can vary, along with their emotional response depending on their age, past experiences and other factors [6]. Older adults are particularly susceptible to isolation. Both loneliness and social isolation, particularly at an advanced age, can have negative effects on physical and mental health and quality of life [7]. In any global pandemic, anxiety regarding one’s health and other aspects of daily life, such as how to get groceries or what to do if a family member becomes ill, can become significantly pronounced [8]. During the Covid-19 epidemic, social distancing and the anxiety of infection created similar obstacles with grocery store owners and health clinics keeping their doors closed. Individuals over 80 are more vulnerable to loneliness at baseline, which is exacerbated in times of disaster [7-9]. Furthermore, the prevalence of increased depressive and anxiety-related symptoms among older adults during the COVID-19 pandemic saw an early correlation with the stringency of government restrictions [10].
The pandemic also had a significant impact on the number of patient clinic visits. Existing data shows that as the initial government restrictions began, overall patient visits to providers dropped by almost 60% starting in the middle of March [11]. Patients over the age of 75 had an initial decline in clinic visits of 70%, the largest decline of any other age group. Mental health weekly visits, in particular, declined by 15% from weeks 10 through 52 (Mid-March through December 2020) compared to baseline visit totals during the first week of March 2020. While in-person visits declined sharply, telehealth visits rapidly began to increase, reaching a peak of approximately 12-13% of total healthcare visits by mid-April 2020 [11]. Psychiatric telehealth visits quickly became the most common type of patient visit for telemedicine, with visits increasing over 260% from March through May 2020 compared to the same time period in 2019 [11,12]. Racial differences have been observed regarding stress and resilience between African-American/Black (AA) and Caucasian-American/White (CA) populations in the U.S. during COVID-19. In spite of facing income and health disparities, African-Americans (AAs) remained more resilient, optimistic and having better overall mental health than Caucasian-Americans (CAs) throughout the COVID-19 pandemic, with the largest differences seen between low-income AAs and low-income CAs [13].
Unlike some other parts of the world, the current U.S. population has not experienced a serious epidemic or pandemic necessitating widespread government action and restrictions, as in the case of SARS or Ebola [11,12]. The most comparable experience in the U.S. has been with large-scale social disruptions and public health emergencies from natural disasters. After hurricanes Katrina and Rita in 2005, a study was performed to characterize the effects of natural disasters on VA-associated nursing home patients over 65. Over 60% of the study’s respondents reported symptoms of psychological distress that persisted long after the patients evacuated safely and were preparing to return home [7].
On March 20, 2020, the Arkansas Department of Health issued directives to close schools, gyms, indoor entertainment venues, and shut down dine-in restaurants. Local and state social distancing rules and curfews followed.13 Research has demonstrated that one of the best interventions healthcare providers can share with an aging population amid a disaster is to provide education from trusted sources of information, like the Centers for Disease Control (CDC) and World Health Organization (WHO) [14]. The purpose of this study was to evaluate the burden of stress from COVID-19 and social distancing restrictions on older adults, aged 55 years and older. In addition, we looked for any differences between African-American/Black (AA) and Caucasian-American/White (CA) older adults regarding COVID-19 isolation stress and various coping strategies that were utilized during the COVID-19 pandemic in Central Arkansas. The results of the survey from our study will be used to evaluate common stressors, predict popular coping strategies, and develop targeted educational programs.
Methods
- Participants and procedure
This was a cross-sectional, convenience sample study design. An anonymous survey was administered between May 2020 and December 2021. During this time, the state of Arkansas was under various Executive Orders and directives that closed businesses, public and private venues, limited occupancy and travel, and mandated social distancing [13]. The survey questions targeted the burden of stress and anxiety in older adults to determine how they were generally coping with the mental, physical and social burdens of stay-at-home recommendations and social distancing due to the COVID-19 pandemic. The survey consisted of yes/no, multiple-select and open-ended questions along with demographic information. The University of Arkansas for Medical Sciences (UAMS) Institutional Review Board reviewed and approved the study and consent form prior to soliciting respondents for survey participation (IRB #261078).
All adults aged 55 and older were eligible to participate in the study, inclusive of all ethnicities, races and genders. Recruitment was done through flyers posted around the UAMS campus and at the UAMS Reynolds Institute on Aging. Previous study participants willing to be contacted about new studies were also contacted via phone or email. Interested respondents were mailed a copy of the survey or emailed a link to complete an electronic version via Google Forms. If preferred, respondents could complete the survey by telephone with study staff. All demographic information collected from the survey was self-reported by respondents. Following completion of the survey, respondents were sent a package of educational materials from the CDC and WHO about coping strategies and COVID-19 via e-mail or the US postal service.
- Data analysis
Study data were collected and managed using REDCap electronic data capture tools hosted at UAMS [15]. Respondents were not required to answer every question if they were unable or unwilling to do so, or if they unintentionally overlooked a question. Unanswered questions were not unexpected. Responses were summarized with frequencies and percentages. Comparisons of responses from AAs and CAs were tested with chi-square tests (or chi-square exact for categories with sparse counts) or Mann Whitney U (for ordinal variables). A significance level of 0.05 was applied to two-sided hypotheses for the tests. Analyses were performed using SAS version 9.4. Figures were generated using Graph Pad Prism 10.
Results
- Demographics
Initially, a total of 118 individuals aged 55 years and older responded to the COVID-19 Emotional Impact Survey. Twelve respondents of either mixed parentage (more than one race), extremely low frequency, or unknown race were excluded from analysis, given the objective to test differences by race. This left an analysis dataset of sample size of 106, 81 CAs and 25 AAs. The majority of respondents were CA (76%), female (80%), educated (completed a trade school, university, or higher) (56%), and retired (70%) (n=106) (Table 1). Thirty percent respondents indicated that they lived alone, and 16% reported coming from a disadvantaged background. Approximately 12% of all respondents reported being disabled and 13% indicated that they lived in a medically underserved community. Over half the respondents lived in an urban area (58%) while almost one-third lived in rural settings (29%). This finding was more pronounced among AA respondents, in which 68% reported living in an urban setting compared to 56% CAs. Relatedly, only 12% AAs reported living in rural settings compared to 35% CAs, the only significant racial group difference in demographics (Table 1, p < 0.05).
|
|
Total N (%) n=1061 |
(CA) N (%) n=81 |
(AA) N (%) n=25 |
P-value² |
|
Race |
|
|
|
|
|
African-American/Black (AA) |
25 (24%) |
– |
– |
– |
|
Caucasian-American/White (CA) |
81 (76%) |
– |
– |
– |
|
Gender |
|
|
|
Pχ=0.58 |
|
Female |
85 (80%) |
64 (79%) |
21 (84%) |
|
|
Male |
21 (20%) |
17 (21%) |
4 (16%) |
|
|
Education |
|
|
|
PMWU=0.19 |
|
Graduate/Post-Graduate |
38 (36%) |
30 (37%) |
8 (32%) |
|
|
Completed Trade School or University |
21 (20%) |
18 (22%) |
3 (12%) |
|
|
Some Trade School or University |
28 (26%) |
22 (27%) |
6 (24%) |
|
|
High School or Less |
19 (18%) |
11 (14%) |
8 (32%) |
|
|
Occupation |
|
|
|
Pχ-exact=0.13 |
|
Retired |
74 (70%) |
60 (74%) |
14 (56%) |
|
|
Employed |
28 (26%) |
19 (23%) |
9 (36%) |
|
|
Unemployed |
4 (4%) |
2 (2%) |
2 (8%) |
|
|
Living Arrangements |
|
|
|
|
|
Living Alone |
32 (30%) |
24 (30%) |
8 (32%) |
Pχ=0.82 |
|
Disadvantaged Background |
17 (16%) |
10 (12%) |
7 (28%) |
Pχ-exact=0.11 |
|
Disabled |
13 (12%) |
7 (9%) |
6 (24%) |
Pχ-exact=0.074 |
|
Living in Medically Underserved Area |
14 (13%) |
9 (11%) |
5 (20%) |
Pχ-exact=0.31 |
|
Urban Setting |
62 (58%) |
45 (56%) |
17 (68%) |
Pχ=0.27 |
|
Rural Setting |
31 (29%) |
28 (35%) |
3 (12%) |
Pχ=0.030* |
|
Other Setting |
13 (12%) |
8 (10%) |
5 (20%) |
Pχ-exact=0.29 |
|
Covid-19 Testing |
|
|
|
|
|
Tested for COVID-19 |
32 (30%) |
22 (27%) |
10 (40%) |
Pχ=0.22 |
|
Ever Positive for COVID-193 |
9 (28%) |
5 (23%) |
4 (40%) |
Pχ-exact=0.41 |
Table 1: Demographics.
1Initially, a total of 118 respondents initially responded. However, given the comparison of non-sparse race categories, African-American/Black and Caucasian-American/White, only the 106 reporting these races were included in the analysis.
2Race comparisons of education level were performed by Mann Whitney U Test (PMWU), rather than by Chi square. All others were performed by Chi-square (Pχ) or Chi-square exact (Pχ exact) as described in methods.
3The denominator for “Ever positive for COVID-19” is based on the 32 who were tested for COVID-19.
*P-value < 0.05
- COVID-19 testing
In our study, 32 (30%) respondents were tested for COVID-19 and only nine (28%) of those tested, were positive (Table 1). There was no significant racial difference between the number of respondents who underwent COVID-19 testing or who had a positive COVID-19 test result.
- Sources of stress
Respondents were asked a total of three questions related to sources of COVID 19 isolation stress, coping strategies, and media coverage related to COVID-19. Respondents were asked, “What has stressed you the most about social distancing because of the virus (check all that apply)?” The most frequently cited source of stress was decreased social interactions with friends and family outside the home, selected by 77% respondents (Figure 1). Shortages at the grocery store or restrictions on shopping were cited by 57% respondents. Three additional stressors that were frequently cited included the inability to attend places of worship (51%); engage in fewer group-oriented recreational activities (50%); and travel out of state (45%). Fear of losing a job or financial stress was perceived by only 8% respondents with no significant difference between AAs and CAs. Interestingly, only 15% respondents experienced stress from being unable to see their doctors, as reported by 16% CAs and 12% AAs.
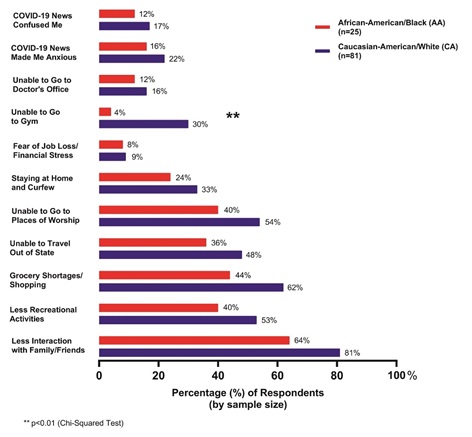 Figure 1: Sources of stress during COVID-19 Isolation.
Figure 1: Sources of stress during COVID-19 Isolation.
In addition to restrictions, news related to COVID-19 was a source of anxiety or confusion for roughly a third of respondents. When asked, “How have the TV and newspaper articles on the coronavirus affected you?” 38% reported feeling anxious and 29% reported feeling confused. Though not significant, interesting differences were observed between the two racial groups. Twenty-two percent CAs experienced anxiousness due to news coverage of COVID-19 versus just 16% AAs. In addition, 17% CA respondents indicated that COVID-19 news coverage made them feel confused in contrast to only 12% of their AA counterparts. Overall, results seemed to suggest a general tendency for more CAs to cite sources of stress than AAs. Nonetheless, the only significant difference in COVID-19 stressors we observed was the inability to go to the gym, reported by 30% CA respondents surveyed and only 4% AA respondent (Figure 1, p < 0.01).
- Coping Strategies during COVID-19 Isolation
To understand coping strategies the survey asked, “What has helped you deal with stress during the social distancing period (check all that apply)?” The most common response was “Talking with Friends”, selected by 62% respondents (Figure 2). This was followed by “Sought Family Support” and “Exercise/Physical Activity”, reported by 57% and 42% respondents, respectively. Thirty-five percent respondents used social media as a coping strategy during COVID-19 isolation. Similarly, 37% respondents engaged in writing, music, art, and/or reading to cope during COVID-19 isolation periods. Half (50%) of those surveyed found TV and newspaper coverage of COVID-19 useful for coping during COVID-19 isolation.
“Talking with Friends” was a preferred coping strategy for 69% CA respondents, a sharp contrast to just (40%) AA respondents (Figure 2, p < 0.01). Furthermore, a highly significant racial difference was observed regarding TV and newspaper coverage of COVID-19. Seventy-six percent AAs found media sources useful, differing greatly from 42% CAs who agreed (Figure 2, p < 0.01).
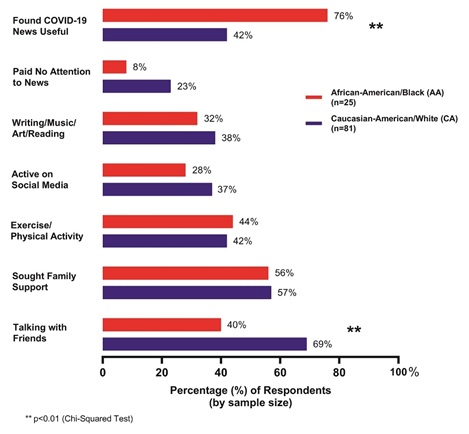 Figure 2: Responses for stress coping mechanisms during COVID-19 isolation.
Figure 2: Responses for stress coping mechanisms during COVID-19 isolation.
- Perspectives on telehealth and adaptability
Of the 41 (39%) respondents who reported using telehealth for their clinic visits, 39 respondents, 28 CAs and 11 AAs, answered the follow-up question, “How do you feel about those visits compared to face-to-face visits?” (Figure 3). Differences between AAs and CAs were markedly noticeable. Half of the CAs were dissatisfied with telehealth visits whereas none of those in the AA cohort experienced any unease with telehealth. Forty-five percent AA respondents rated telehealth visits as “New and Exciting” versus only 11% of their CA peers. Lastly, 55% AAs agreed that “Telehealth is the same as a Face-to-Face Visit” compared to 39% CAs. The distribution of selections among the three aforementioned options differed significantly between the AA and CA cohorts (Figure 3, p < 0.01).
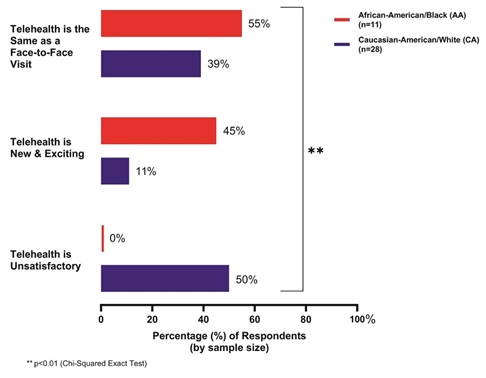 Figure 3: Opinions on the use of telehealth.
Figure 3: Opinions on the use of telehealth.
Discussion
The COVID-19 pandemic has brought about additional stressors that have an impact on emotional health. Some of the stressors include social isolation, financial issues, commodity shortages, confusion and lack of understanding of the virus. Our study highlights the coping strategies in response to the COVID-19 pandemic in older adults, both in terms of specific stressors and in stress coping strategies. Although it has been suggested that isolation from social distancing measures can potentially affect mental health in a number of ways, the psychological impacts of compulsory isolation, such as social distancing and stay-at-home orders, are not yet well understood [16]. It is important to note that quarantine requirements may have both an acute and chronic impact on mental health, particularly in those who are perceived to be in higher risk groups, such as those with lower income and/or education, older adults or those who have been more impacted by the economic consequences of COVID-19 [17].
- General differences in the impacts of COVID-19 related stress
We might infer that the consequences of government mandates play a role in raising psychological stress. Benke et al., [17] found that increased lockdown restrictions were associated with higher mental health impairments [16]. Similarly, Whitehead et al. observed that stay-at-home orders were associated with higher anxiety and increased financial concerns [17]. However, state and/or local stay-at-home mandates are not the only cause of increased stress or other mental health symptoms. For example, Whitehead et al. noted that primary sources of stress among older adults included generalized anxiety regarding the pandemic itself, restrictions, daily life changes due to the pandemic and overall well-being [17]. Kivi et al., found that older adults generally seemed to report high rates of well-being, but those who tended to worry more also had a greater tendency to identify with lower states of well-being [18,19]. Thus, there appears to be variability in how the pandemic has affected various populations. In our study, the most commonly reported stressful factor among older adults was a reduction in their social activities. Other studies have also found a subsequent decrease in social activities resulting from COVID-19 social distancing requirements [16,17,19,20].
A number of studies have found that although stress and/or anxiety due to the COVID-19 pandemic and its repercussions has increased among all ages, older adults typically experience lower psychological stress and/or anxiety than do younger adults [21-25]. Despite these differences, the vulnerability of older adults regarding health impacts from COVID-19 cannot be discounted. High vulnerability persists among older adults due to significantly elevated health risks associated with COVID-19 virus infections, such as a propensity to suffer more severe symptoms and experience other potential complications [26].
- Racial differences in coping methods, resilience and adaptability
Overall, AA and CA respondents differed in the number of stressful social isolation factors they experienced, with AAs choosing a lower number of stressors and reduced severity of those stressors compared to CAs. These results seem contrary to a few other COVID-19 stress related studies that looked at racial differences in adults and found that AA respondents experienced a greater number of COVID-19 related stressors than their CA counterparts [27,28]. These studies also reported lower levels of emotional impacts on mental health due to stress. Our results seem to be in agreement with the finding of CAs reporting higher mental health impacts in response to COVID-19-related stressors [27,28]. However, it should be noted that with regard to stressors, our survey question referred more specifically to the stressors associated with social isolation and therefore may not be a true measure of comparison. Although both AAs and CAs in our study reported decreased social interaction as the most stressful factor associated with COVID-19 social isolation, CAs cited this factor at a significantly higher frequency than AAs. CA respondents more often reported that not being able to access places of worship and difficulties in accessing exercise facilities such as gyms were among their highest stressors. CA respondents relied on talking with friends most often and at a significantly higher rate than AA subjects, who most frequently depended on family support as a way of coping with the stress from COVID-19 isolation.
There have been a number of observations during the COVID-19 pandemic, which have begun to shed light on coping and resilience. For example, it has been theorized and observed that older adults tend to be more resilient than younger adults [29-31]. It has also been noted that more frequent use of proactive coping methods led to increased general knowledge which lowered COVID-19-related stress, particularly among older adults [29]. This may partly explain the reason we observed nearly half of the respondents in our study reporting that news media sources were useful in dealing with stress during the COVID-19 pandemic. We found that AA respondents were more likely to find this information useful, which perhaps helped mitigate the degree of anxiety (such as having a better understanding of how to protect oneself from the virus). Carstensen has stated that one advantage of aging is that it allows the individual to witness events and situations that occur and evolve over a period of years or decades. Additionally, the effects of these experiences cannot be recognized or evaluated during times of extreme environmental changes [31,32]. Resilience has been suggested to be a positive predictor of mental health during the COVID-19 pandemic [32].
Results from our study suggest that AAs exhibited greater resilience during the pandemic even though a higher percentage of AA respondents had a family member who tested positive for the COVID-19 virus when compared with CA respondents. With difficult experiences throughout life, often coupled with lower socioeconomic status, AAs might have inculcated greater tolerance and capacity to withstand stressful events during the pandemic. Older adults may place a higher level of importance on emotional well-being and emotional goals because of their more limited perception of time. Therefore, they focus more on their emotionally close relationships [31,32]. These close family ties also seemed to be reflected in coping strategies used by AAs, who relied more on family support versus CAs. In our study, AAs appeared to adapt more easily to the changes during the pandemic, and viewed telehealth visits with physicians more favorably than CAs, who often expressed much more dissatisfaction with telehealth. This is contrary to some studies during COVID-19, in which AAs underutilized telehealth compared to CAs [33].
In our study, it appeared that our respondents relied heavily on social forms of support in order to cope with the COVID-19 pandemic - be it from family members or friends. Within current literature, social factors have been observed as seemingly crucial forms of coping with significant stressors associated with larger-scale traumatic events in societies. Two studies have identified two key social factors associated with coping, which positively affected older adults who had experienced tsunami events. Both studies found that cultural and faith-based aspects of coping were beneficial for adults aged 60 and over in managing their mental health and well-being, both which had greatly been impacted due to traumatic experiences of living through tsunami disasters and the long-term repercussions [34,35]. Almazan et al., concluded that cultural factors, such as detailed knowledge that is brought from multi-generational experiences of traumatic events, could have a positive influence on resilience and adapting to major changes. In this respect, social forms of support and cultural aspects can be interwoven [35,36]. It is unknown as to what extent cultural factors, prior trauma or social determinants of health may have played in coping strategies among the subjects from our study. There are a few studies that have explored AA resilience and suggested that it reflects their sustained ability to survive a century or more of social injustice and environmental adversities [36]. Further studies will need to be performed to delineate these factors and identify the unique strengths and adaptability of older AA adults.
Limitations
Surveys can be subject to individual interpretation and/or misunderstanding among respondents. We did not systematically study all the social determinants of health and cultural factors, which could have impacted coping strategies [37-39]. Respondents may not remember precise details of events and/or past feelings or experiences with great clarity. Thus, volunteer bias and/or recall bias might have occurred to some extent [40,41].
Conclusion
In this study, we examined how stress from social isolation and social distancing restrictions in Arkansas, during the COVID-19 pandemic, affected the physical and mental health of older adults, with a particular focus on the emotional impacts and race. Studies on mental health impacts from the COVID-19 pandemic are increasing, but understanding the impact is still in a stage of infancy. The pandemic has been an ever-changing situation, which has affected the global population in some manner. Therefore, we must study a diverse population and tease out differences in the coping strategies of people from different backgrounds, races and ethnicities. Future study findings may serve as valuable tools to improve therapeutic approaches in maintaining health, adaptability and resilience during times of emotional stress in people of all different backgrounds as a result of societal crises.
Author Contributions
Gohar Azhar, M.D.: Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; drafting the work or revising it critically for important intellectual content; final approval of the version to be published; agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Micah Smith, M.D.: Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; drafting the work or revising it critically for important intellectual content.
Elizabeth Eoff, M.D.: Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work.
Melodee Harris, Ph.D.: Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work.
Regina Gibson, Ph.D.: Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work.
James R Perry, B.S.: Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; drafting the work or revising it critically for important intellectual content; final approval of the version to be published.
Karen Coker, Ph.D.: Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; drafting the work or revising it critically for important intellectual content.
Patricia Savary, B.S.: Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; drafting the work or revising it critically for important intellectual content; final approval of the version to be published.
Kenneth Alderson, B.S.: Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work.
Taylor Zhang, B.S.: Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work.
Jeanne Wei, M.D., Ph.D.: Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work.
Data Statement
The data has not been previously presented orally or by poster at scientific meetings.
Disclosures
The authors report no conflicts with any product mentioned or concept discussed in this article. The authors disclosed received financial support for the research, authorship, and/or publication of this article in part from the Donald W. Reynolds Institute on Aging at the University of Arkansas for Medical Sciences (UAMS).
Supplementary Materials
The original data, along with other data collection tools used in this study are available to other researchers for replication purposes and can be accessed upon request by contacting the corresponding author via email or phone.
References
- Zhu K, Niu Z, Freudenheim JL, Zhang ZF, Lei L, et al. (2021) COVID-19 related symptoms of anxiety, depression, and PTSD among US adults. Psychiatry Res 301: 113959.
- McCormack GR, Doyle-Baker PK, Petersen JA, Ghoneim D (2021) Perceived anxiety and physical activity behaviour changes during the early stages of COVID-19 restrictions in community-dwelling adults in Canada: A cross-sectional study. BMJ Open 11: 050550.
- Choi EPH, Hui BPH, Wan EYF (2020) Depression and anxiety in Hong Kong during COVID-19. Int J Environ Res Public Health 17: 3740.
- Kim DM, Bang YR, Kim JH, Park JH (2021) The prevalence of depression, anxiety and associated factors among the general public during COVID-19 pandemic: A cross-sectional study in Korea. J Korean Med Sci 36: 214.
- Wang C, Pan R, Wan X, Tan Y, Xu L, et al. (2020) Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health 17: 1729.
- Moore RC, Lee AY, Hancock JT, Halley MC, Linos E (2021) Age-related differences in experiences with social distancing at the onset of the COVID-19 pandemic: A computational and content analytic investigation of natural language from a social media survey. JMIR Hum Factors 8: 26043.
- Claver M, Dobalian A, Fickel JJ, Ricci KA, Mallers MH (2013) Comprehensive care for vulnerable elderly veterans during disasters. Arch Gerontol Geriatr 56: 205-213.
- Gusmano MK, Rodwin VG (2006) The elderly and social isolation. Testimony to Committee on Aging, NYC Council, USA.
- Sharma D, Clune S, Blair L (2015) Radicalising the designer: Combating age-related loneliness through radical-digital interventions. Summer Cumulus Conference associated with the Politecnico di Milano.
- Voss G, Paiva AF, Delerue Matos A (2021) A study of the association between the stringency of covid-19 government measures and depression in older adults across Europe and Israel. Int J Environ Res Public Health 18: 8017.
- Mehrotra A, Chernew ME, Linetsky D, Hatch H, et al. (2021) The Impact of COVID-19 on Outpatient Visits in 2020: Visits Remained Stable, Despite a Late Surge in Cases. The Commonwealth Fund.
- Ridout KK, Alavi M, Ridout SJ, Koshy MT, Harris B, et al. (2021) Changes in diagnostic and demographic characteristics of patients seeking mental health care during the early COVID-19 pandemic in a large, community-based health care system. J Clin Psychiatry 82: 20.
- Graham C, Chun Y, Hamilton B, Roll S, Ross W, et al. (2022) Coping with COVID-19: Differences in hope, resilience, and mental well-being across U.S. racial groups. PLoS One 17: 0267583.
- Husch Blackwell (2021) Arkansas: State-by-State COVID-19 Guidance. Husch Blackwell, Missouri, USA.
- Banks L (2013) Caring for elderly adults during disasters: improving health outcomes and recovery. South Med J 106: 94-98.
- Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, et al. (2019) The REDCap consortium: Building an international community of software platform partners. J Biomed Inform 95: 103208.
- Benke C, Autenrieth LK, Asselmann E, Pané-Farré CA (2020) Lockdown, quarantine measures, and social distancing: Associations with depression, anxiety and distress at the beginning of the COVID-19 pandemic among adults from Germany. Psychiatry Res 293: 113462.
- Whitehead BR, Torossian E (2021) Older adults’ experience of the COVID-19 pandemic: A mixed-methods analysis of stresses and joys. Gerontologist 61: 36-47.
- Kivi M, Hansson I, Bjälkebring P (2021) Up and about: Older adults’ well-being during the COVID-19 pandemic in a Swedish longitudinal study. J Gerontol B Psychol Sci Soc Sci 76: 4-9.
- Emerson KG (2020) Coping with being cooped up: Social distancing during COVID-19 among 60+ in the United States. Rev Panam Salud Pública 44: 81.
- Kotwal AA, Holt-Lunstad J, Newmark RL, Cenzer I, Smith AK, et al. (2021) Social Isolation and Loneliness Among San Francisco Bay Area Older Adults During the COVID-19 Shelter-in-Place Orders. J Am Geriatr Soc 69: 20-29.
- Kowal M, Coll-Martín T, Ikizer G, Rasmussen J, Eichel K, et al. (2020) Who is the Most Stressed During the COVID-19 Pandemic? Data From 26 Countries and Areas. Appl Psychol Health Well Being 12: 946-966.
- Ebrahimi OV, Hoffart A, Johnson SU (2021) Physical distancing and mental health during the COVID-19 pandemic: Factors associated with psychological symptoms and adherence to pandemic mitigation strategies. Clin Psychol Sci 9: 489-506.
- Varma P, Junge M, Meaklim H, Jackson ML (2021) Younger people are more vulnerable to stress, anxiety and depression during COVID-19 pandemic: A global cross-sectional survey. Prog Neuropsychopharmacol Biol Psychiatry 109: 110236.
- Klaiber P, Wen JH, DeLongis A, Sin NL (2021) The ups and downs of daily life during COVID-19: Age differences in affect, stress, and positive events. J Gerontol B Psychol Sci Soc Sci 76: 30-37.
- Pasion R, Paiva TO, Fernandes C, Barbosa F (2020) The AGE effect on protective behaviors during the COVID-19 outbreak: Sociodemographic, perceptions and psychological accounts. Front Psychol 11: 561785.
- Zeng F, Deng G, Cui Y, Zhang Y, Dai M, et al. (2020) A predictive model for the severity of COVID-19 in elderly patients. Aging (Albany NY) 12: 20982-20996.
- Bui CN, Peng C, Mutchler JE, Burr JA (2021) Race and ethnic group disparities in emotional distress among older adults during the COVID-19 pandemic. Gerontologist 61: 262-272.
- Goldmann E, Hagen D, Khoury EE, Owens M, Misra S, et al. (2021) An examination of racial and ethnic disparities in mental health during the Covid-19 pandemic in the U.S. South. J Affect Disord 295: 471-478.
- Pearman A, Hughes ML, Smith EL, Neupert SD (2021) Age Differences in Risk and Resilience Factors in COVID-19-Related Stress. J Gerontol B Psychol Sci Soc Sci 76: 38-44.
- Verhage M, Thielman L, de Kock L, Lindenberg J (2021) Coping of older adults in times of Covid-19: Considerations of temporality among Dutch older adults. J Gerontol B Psychol Sci Soc Sci 76: 290-299.
- Carstensen LL (2019) Integrating cognitive and emotion paradigms to address the paradox of aging. Cogn Emot 33: 119-125.
- Li F, Luo S, Mu W, Li Y, Ye L, et al. (2021) Effects of sources of social support and resilience on the mental health of different age groups during the COVID-19 pandemic. BMC Psychiatry 21: 16.
- Smith CB, Bhardwaj AS (2020) Disparities in the use of telehealth during the COVID-19 pandemic. Clin Oncol 38: 87.
- Soonthornchaiya R, Tuicomepee A, Romano JL (2019) Impacts of tsunami disaster in Thai elderly survivors. Ageing Int 44: 154-169.
- Almazan JU, Cruz JP, Alamri MS, Albougami ASB, Alotaibi JSM, et al (2019) Coping Strategies of Older Adults Survivors Following a Disaster: Disaster-Related Resilience to Climate Change Adaptation. Ageing Int 44: 141-153.
- Taylor HA Jr, Washington-Plaskett T, Quyyumi AA (2020) Black Resilience - Broadening the Narrative and the Science on Cardiovascular Health and Disease Disparities. Ethn Dis 30: 365-368.
- Hahn RA (2021) What is a social determinant of health? Back to basics. J Public Health Res 10: 2324.
- Wolfson JA, Leung CW, Kullgren JT (2020) Food as a critical social determinant of health among older adults during the coronavirus disease 2019 (COVID-19) Pandemic. JAMA Health Forum 1: 200925.
- Airhihenbuwa CO, Iwelunmor J, Munodawafa D, Ford CL, Oni T, et al. (2020) Culture matters in communicating the global response to COVID-19. Prev Chronic Dis.
- Sedgwick P (2013) Questionnaire surveys: sources of bias. BMJ 347: f5265.
Citation: Azhar G, Smith M, Eoff E, Harris M, Gibson R, et al. (2024) Racial Differences in the Emotional Impact and Coping Strategies Employed by Older Adults during the COVID-19 Pandemic in Arkansas. J Gerontol Geriatr Med 10: 221.
Copyright: © 2024 Gohar Azhar, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

