
Recanalization of Acute Mesenteric Artery Occlusion by Percutaneous Transluminal Angioplasty Followed by Stent Implantation
*Corresponding Author(s):
João Lucas O’ConnellDepartment Of Cardiology, Federal University Of Uberlândia, Uberlândia, Brazil
Tel:+55 34996651159,
Email:oconnelljl@me.com
Abstract
Mesenteric ischemia is caused by stenosis of the mesenteric arteries and is associated with high morbidity and mortality. While surgical revascularization has been the standard treatment for symptomatic patients, recent advances in interventional devices and techniques have made endovascular treatment feasible and effective for this situation. However, there is limited data regarding the role of endovascular therapy in acute mesenteric ischemia. The goal of this manuscript is to report a case of percutaneous transluminal angioplasty with primary stenting for the treatment of an acute occlusion of the superior mesenteric artery and to discuss the role of endovascular treatment in acute mesenteric ischemia scenarios.
AMI is an uncommon condition caused by the severe stenosis or occlusion of the mesenteric arteries. It usually manifests as important abdominal pain (frequently related to food intake) and constitutes a dramatic situation in the emergency room. A key goal of the therapy in acute mesenteric artery occlusions is to rapidly reestablish blood flow into the vessel and to assess the viability of the ischemic bowel segment.
The open surgery is considered to be the the most appropriate therapy. However, endovascular treatment may be considered in some situations: acute mesenteric ischemia without evidence of peritoneal irritation (early stage ischemia), in patients with a very high operative risk infection of the peritoneal cavity with no available autologous vessel for grafting or compassionate treatment. The case presented in this manuscriptshows the feasibility of the endovascular therapy to treat acute mesenteric artery occlusion in this dramatic situation.
Keywords
INTRODUCTION
CASE DESCRIPTION
She had visited 4 different doctors and gone through different blood exams, endoscopy, colonoscopy, abdominal ultrasound and computed tomography without obtaining a specific diagnosis. Finally, CMeI was suspected and an abdominal angiotomography was performed.An important stenosis of the ostial and proximal portion of the mesenteric artery was observed (Figures 1 and 2). An Aortic and Mesenteric angiographywas indicated in order to confirm diagnosis and program appropriate treatment. However, two days before this exam she developed an intensive abdominal pain (similar to the prior episodes) that persisted after 60 minutes. She got to the hospital about 1 hour after the initial symptoms and hypotension (70/40mmHg) and bradycardia (44 bpm) were observed. No other alterations in neurological, cardiovascular or respiratory exam were observed. Signs of peritonitis were not present. No signs of ileus, pneumatosis intestinalis, bowel obstruction, perforation or wall thickening were found on plain abdominal radiographs.
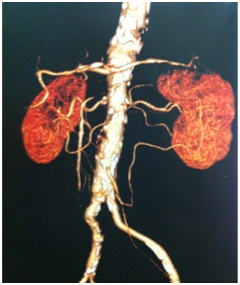 Figure 1: Important stenosis of the ostial and proximal portions of the superior mesenteric artery identified by abdominal angiotomography.
Figure 1: Important stenosis of the ostial and proximal portions of the superior mesenteric artery identified by abdominal angiotomography. Figure 2: Abdominal AngioCT showing an important stenosis of the Superior Mesenteric Artery.
Figure 2: Abdominal AngioCT showing an important stenosis of the Superior Mesenteric Artery. Figure 3: Recanalization of the Superior Mesenteric Artery obtained by the use of a coronary ballon cateter.
Figure 3: Recanalization of the Superior Mesenteric Artery obtained by the use of a coronary ballon cateter. Figure 4: Final Result obtained after the implantation of a coronary bare metal stent involving the ostial and proximal portions of the superior mesenteric artery.
Figure 4: Final Result obtained after the implantation of a coronary bare metal stent involving the ostial and proximal portions of the superior mesenteric artery.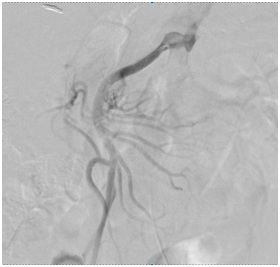 Figure 5: Final result of the procedure after stent implantation in the superior mesenteric artery with great improve in blood flow to the bowel vessels.
Figure 5: Final result of the procedure after stent implantation in the superior mesenteric artery with great improve in blood flow to the bowel vessels.Intervention
Outcome
Evolution
DISCUSSION
When the blood supply to the bowel becomes inadequate, patient experiences postprandial pain also known as intestinal angina. Weight loss and a fear of eating develop and can lead toimportant malnutrition. Persistent nausea or diarrhea can be present. Incapacitating gastroparesis may cause vomiting, postprandial heaviness, gastroduodenal bleeding and delayed gastric emptying [5]. Women who are heavy smokers are selectively affected. Without treatment at the early stage of gastroparesis the prognosis is extremely poor. Isolated cachexia often prompts costly investigations for malignancy [6]. As a result the diagnosis of CMI is often delayed.
Acute intestinal ischemia with infarction of the intestine and mesentery is a complication that is associated with a grim prognosis. Therefore, rapid diagnosis and treatment of a critical obstruction is mandatory for symptomatic patients. The case described in this manuscript developed abdominal pain that was not initially carachterized as intestinal angina because it was not well related to food intake. The weight loss that the patient developed led to expensive investigation for malignant causes. Her visit to different doctors and the use of multiple exams, without reaching a correct diagnose evidence the difficulties associated with the avaliation of these critical patients.
Some methods are indicated forthe detection of stenosis or occlusion of mesenteric arteries. These include fasting and postprandial doppler ultrasonography, magnetic resonance angiography and most importantly, computed tomographic angiography (specially indicated in patients with good renal function). However, angiography remains the gold standard and also the first step of every endovascular procedure [3]. In this related case, the presence of an important obstruction in the mesenteric artery as the main cause of patient’s symptoms was clearly observed in the angiotomography.
Treatment is required for patients with symptomatic MeI. The goals of treatment are to ensure symptom resolution, to correct nutritional status and to prevent intestinal infarction. Prophylactic revascularization in patients with asymptomatic MI remains unclear. Unfortunetly, nearly one-half of patients with asymptomatic lesions may experience acute intestinal ischemia as the first manifestation [7]. However, the natural history of mesenteric artery stenosis remains unclear and there is no formal indication to revascularize assymptomatic patients.
The conventional treatment for MeI consists of open endarterectomy or bypass surgery, which has a 15% to 47% morbidity rate and a 0% to 17% mortality rate with a high long-term artery patency (60-79%), and a high five-year survival rate (more than 60%) [8-12]. Thus surgical treatment is the reference standard: the immediate and long-term success rates are high. Although the invasiveness of conventional surgery is a disadvantage in several patients with MI, specially in those who have a high operative risk. Stenoses of mesenteric arteries are usually focall and are located at the ostium or proximal part of the vessel - two characteristics that make them accessible to endovascular treatment.Endovascular intervention is safer in the short term, with 0% to 11% mortality and 0% to 18% morbidity [13].
A meta-analysis of 16 studies (published between 1995 and 2006) comprising 328 patients with MeI who were treated using endovascular techniques shows that endovascular treatment is safe and is associated with very low morbidity and mortality rates. Stenting increases the immediate success rate and also increases the long-term risk of restenosis which is fairly well tolerated. Although the long-term patency rate is lower than reported with conventional surgery the low morbidity rate gives endovascular treatment a place of choice in the management of MI, particularly in higher-risk patients and in acutely ill patients [13]. However, there is limited data envolving the use of angioplasty followed (or not) by stent implantation in acute scenarios.
Acute Mesenteric Ischemia (AMeI) requires emergent conventional surgery to revascularize the artery and above all to visually assess the viability of the ischemic bowel segment. In general there is no formal role for endovascular treatment and surgical treatment should be indicated. Endovascular treatment may be considered in somespecific situations: in cases of acute mesenteric ischemia without evidence of peritoneal irritation (indicating early stage ischemia) in the presence of a very high operative risk in cases associated with peritoneal infection, in cases with no available autologous vessel for grafting or for compassionate treatment [14-16].
In a recente systematic review Ierardi et al., found that AMeI was predominantly caused by arterial emboli from cardiac arrhythmias (40-50%), thrombosis at preexisting lesions (25%) and other non-occlusive causes. The Superior Mesenteric Artery (SMA) was the commonest site of thromboembolic occlusion because of its oblique origin from the aorta. Abdominal pain, vomiting and nausea were the most common presenting symptoms [2].
The study of Arthurs, et al., represented the largest series of patients with AMI treated with endovascular therapy in one center. They retrospectively evaluated 70 patients with AMeI in whom endovascular revascularization was the preferred treatment (81%). The primary technique was thrombolysis infusion which was used in 48% of the population. Thirty-two percent of patients were treated with primary PTA and stenting. Aspiration thrombectomy in conjunction with thrombolysis was performed in 12% of patients. Successful endovascular treatment was achieved in 87% of cases, and the mortality rate was 36%, compared with 50% (P<0.05) in patients treated with traditional therapy.
Acute renal failure, myocardial and cerebral infarctions, bowel ischemia and short bowel syndrome are the most common complications reported in literature within acute percutaneouly revascularized patients. Potential complications related to the endovascular procedure included access-related bleeding (e.g. hematoma, pseudoaneurysm) and vessel trauma that can lead to arterial dissection or atheroembolization. The use of distal embolic protection devices may mitigate the risk of bowel necrosis as a consequence of distal embolization but there is a lack of data concerning their efficacy in the mesenteric circulation [2].
The clinical case described in this manuscript shows that angioplasty and stenting ot the mesenteric vessels, if performed early, can prevent intestinal infarction and obviate the need for laparotomy. This was also evidenced in other previous studies [17-19]. Other studies are necessary to assess long-term outcomes and to stablish the best treatment option to be considered in rapid diagnosed patients with AMeI. However, the low incidence of this acute condition makes such a trial extremely unlikely. This way the description of successful and insuccessful cases and series of cases migth still be very useful.
CONCLUSION
In the acute scencario criticischemia is a dramatic situation in the emergency room. A key goal of the therapy in acute mesenteric artery occlusion is to rapidly reestablish flow into the proximal arterial segments and to assess the viability of the ischemic bowel segment. The open surgery is stillconsidered to be the the most appropriate therapy. However, endovascular treatment may be considered in some situations: acute mesenteric ischemia without evidence of peritoneal irritation (early stage ischemia), in patients with a very high operative risk in patients with peritoneal infection patients with no available autologous vessel for grafting and for compassionate treatment. The case presented in this manuscript proves the feasibility of the endovascular therapy to treat acute mesenteric artery occlusions.
REFERENCES
- Atkins MD, Kwolek CJ, LaMuraglia, Brewster DC, Chung TK, et al. (2007) Surgical revascularization versus endovascular therapy for chronic mesenteric ischemia: a comparative experience. J Vasc Surg 45: 1162-1171.
- Ierardi AM, Tsetis D, Sbaraini S, Angileri SA, Galanakis N, et al. (2017) The role of endovascular therapy in acute mesenteric ischemia. Ann Gastroenterol 30: 526-533.
- Loffroy R, Steinmetz E, Guiu B, Molin V, Kretz B, et al. (2009) Role for endovascular therapy in chronic mesenteric ischemia. Can J Gastroenterol 23: 365-373.
- Hansen KJ, Wilson DB, Craven TE, Pearce JD, English WP, et al. (2004) Mesenteric artery disease in the elderly. J Vasc Surg 40: 45-52.
- Liberski SM, Koch KL, Atnip RG, Stern RM (1990) Ischemic gastroparesis: Resolution after revascularisation. Gastroenterology 99: 252-257.
- Casey KM, Quigley TM, Kozarek RA, Raker EJ (1993) Lethal nature of ischemic gastropathy. Am J Surg 165: 646-649.
- Rose SC, Quigley TM, Raker EJ (1995) Revascularization for chronic mesenteric ischemia: comparison of operative arterial bypass grafting and percutaneous transluminal angioplasty. J Vasc Interv Radiol 6: 339-349.
- Allen RC, Martin GH, Rees CR, Rivera FJ, Talkington CM, et al. (1996) Mesenteric angioplasty in the treatment of chronic intestinal ischemia. J Vasc Surg 24: 415-421.
- AbuRahma AF, Stone PA, Bates MC, Welch CA (2003) Angioplasty/stenting of the superior mesenteric artery and celiac trunk: Early and late outcomes. J Endovasc Ther 10: 1046-1053.
- Kasirajan K, O'Hara PJ, Gray BH, Hertzer NR, Clair DG, et al. (2001) Chronic mesenteric ischemia: Open surgery versus percutaneous angioplasty and stenting. J Vasc Surg 33: 63-71.
- Cunningham CG, Reilly LM, Rapp JH, Schneider PA, Stoney RJ (1991) Chronic visceral ischemia. Three decades of progress. Ann Surg 214: 276-287.
- Mateo RB, O'Hara PJ, Hertzer NR, Mascha EJ, Beven EG, et al. (1999) Elective surgical treatment of symptomatic chronic mesenteric occlusive disease: Early results and late outcomes. J Vasc Surg 29: 821-831.
- Kougias P, El Sayed HF, Zhou W, Lin PH (2007) Management of chronic mesenteric ischemia. The role of endovascular therapy. J Endovasc Ther 14: 395-405.
- Gallego AM, Ramírez P, Rodríguez JM, Bueno FS, Robles R, et al. (1996) Role of urokinase in the superior mesenteric artery embolism. Surgery 120: 111-113.
- Ramirez-Ponce MP, Mateos JC, Carrion N, Bellido JA (1996) Voltage-dependent potassium channels in white adipocytes. Biochem Biophys Res Commun 223: 250-256.
- VanDeinse WH, Zawacki JK, Phillips D (1986) Treatment of acute mesenteric ischemia by percutaneous transluminal angioplasty. Gastroenterology 91: 475-478.
- Kawarada O, Sonomura T, Yokoi Y (2006) Direct aspiration using rapid-exchange and low-profile device for acute thrombo-embolic occlusion of the superior mesenteric artery. Catheter Cardiovasc Interv 68: 862-866.
- Nishida A, Fukui K (2005) Images in clinical medicine. Transcatheter treatment of thromboembolism in the superior mesenteric artery. N Engl J Med 353: 4.
- Demirpolat G, Oran I, Tamsel S, Parildar M, Memis A (2007) Acute mesenteric ischemia: endovascular therapy. Abdom Imaging 32: 299-303.
Citation: O’Connell JL, Borges GC, Vilela R, de Almeida RP (2018) Recanalization of Acute Mesenteric Artery Occlusion by Percutaneous Transluminal Angioplasty Followed by Stent Implantation. J Angiol Vasc Surg 3: 017.
Copyright: © 2018 João Lucas O’Connell, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

